Brachial plexus blocks are among the most commonly performed peripheral nerve blocks in clinical practice and its use in upper extremity procedures have led to improved postoperative pain control, decreased narcotic use, and decreased narcotic-associated side effects such as nausea and vomiting [1,2]. It can be used as the sole anaesthetic technique or in combination with general anaesthesia for intraoperative and postoperative analgesia [3].
The interscalene approach is used commonly for the procedures involving the shoulder, including the lateral two-thirds of the clavicle, proximal humerus and shoulder joint [3]. Roots (C5-C7) are most densely blocked with this approach. However, the ulnar nerve originating from C8 and T1 may be spared which limits its usefulness for distal surgical procedures [4,5].
Various drugs have been used as an adjuvant to local anaesthetics in brachial plexus block to improve the quality of block and to increase the duration of postoperative analgesia with varying results [6,7]. MgSO4 has been reported to be effective in perioperative pain treatment and in blunting somatic, autonomic and endocrine reflexes provoked by noxious stimuli [8,9]. Magnesium has shown greater analgesic potential when added to local anaesthetics in peripheral nerve block.
Materials and Methods
After obtaining approval from institutional academic and ethical committee and written informed consent, this study was conducted in Indira Gandhi Medical College and Hospital, Shimla from August 2016 to July 2017. Sixty patients of either sex, ASA grade I-II and 20-60-year-old were scheduled for upper extremity surgeries were included in this randomised, double blind study. Sample size was recruited on the basis of time duration of the study. All the patients who came in this time period fulfilling the inclusion criteria were included in the study.
Patients with severe pulmonary disease or contralateral phrenic nerve palsy, cardiac, renal or hepatic disease, pre-existing neurological deficit, significant coagulopathy, hypersensitivity to local anaesthetics and study drugs, local sepsis at the site where needle for block is to be inserted and refusing for spinal anaesthesia were excluded from the study.
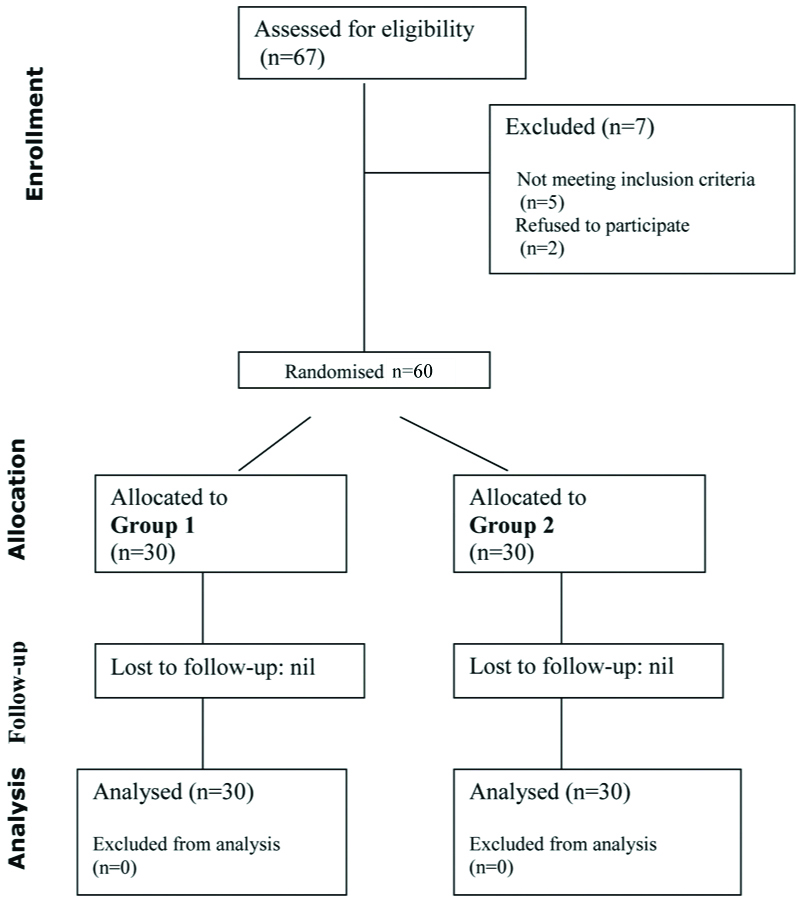
All the patients kept for surgery underwent a pre-anaesthetic evaluation and written informed consent was taken one day prior to the surgery. Visual Analogue Score (VAS) for pain was explained to all the candidates in the preoperative visit where zero corresponded to no pain and 10 corresponds to worst unbearable pain. The enrolled patients after fulfilling all the inclusion and exclusion criteria were randomly allocated to two equal groups (30 patients in each group) using computer generated random number list [Table/Fig-1]. The syringes were loaded with drug by a person not involved in administering the injections and in further evaluation of the patients and the drugs given were disclosed at end of the study. The investigator administering the injection and observing the effects were unaware of the drug injected. In the operation theatre peripheral I.V. line was secured, baseline non-invasive monitoring started and premedication with midazolam 2 mg was given intravenously before the procedure. The patient was positioned supine with the head turned away from the side to be injected. Shoulder roll was kept for enhancing neck extension. The patient neck area was cleaned with chlorhexidine and draped. The ultrasound probe was placed in a sterile probe sheath. We used a SonoSite micro maxx ultrasound machine with HLF38/13-6 MHz 25 mm linear array transducer. Once an optimal view of the nerve roots was established in medial to lateral approach and colour doppler imaging confirmed the absence of blood vessels in the trajectory of the needle, the needle was inserted to a point 1 cm lateral to the lateral edge of the ultrasound probe after giving local (1 mL of 2% lignocaine) in needle puncture site. Nerve block needle was inserted “in plane” with the ultrasound probe, allowing visualisation of the entire needle. Once the needle tip was adjacent to the brachial plexus, an assistant aspirated and then injected 1 mL of local anaesthetic. The optimal needle location was shown by visualising the spread of the local anaesthetic as hypoechoic area around the nerve roots. Once the ideal local anaesthetic spread was visualised, the assistant injected a local anaesthetic taking care to aspirate intermittently after every 3 mL injection of drug solution to avoid any intravascular placement. Group 1 received 20 mL of 0.5% bupivacaine with 0.5 mL of 50% MgSO4 (Total volume=20.5 mL). Group 2 received 20 mL of 0.5% bupivacaine with 0.5 mL of normal saline (Total volume=20.5 mL). Block was evaluated every 3 minutes till 15 minutes after the injection of local anaesthetic or minimum grade 3 was achieved in sensory and motor blockade till maximum of 15 minutes. Motor blockade assessment was performed by modified bromage scale (Grade 1- Able to raise the extended arm to 90 degrees for a full two seconds, Grade 2- Able to flex the elbow and move the fingers but unable to raise the extended arm, Grade 3- Unable to flex the elbow but able to move the fingers, Grade 4- Unable to move the arm, elbow or the fingers). Grade 2 corresponded to onset of motor blockade and Grade 3 onwards was taken as complete blockade.
Assessment of sensory block was done by using Hollmen’s scale (Grade 1- Normal sensation of pin prick, Grade 2- Pin prick felt as sharp pointed but weaker compared with the same area in other extremity, Grade 3- Pin prick felt as touch with blunt object, Grade 4- No perception of pin prick.) Onset of sensory blockade was taken as minimum Grade 2 and complete blockade was Grade 3 and above.
After confirmation of Grade 3 of sensory and motor blockade or completion of 15 minutes, patients were given general anaesthesia with 100 μg Fentanyl, propofol (1.5-2.5 mg/kg), and atracurium (0.5 mg/kg) and surgery was allowed to proceed. General anaesthesia was maintained with O2: N2O: Isoflurane (33%: 66%: 0-1%) after tracheal intubation. Mean Arterial Pressure (MAP), Heart Rate, Respiratory Rate and SpO2 were recorded during surgery at 0, 5, 10, 15, 30 minutes and after every 15 minutes till end of surgery. At the end of surgery, neostigmine 2.5 mg and glycopyrrolate 0.4 mg were given to reverse residual neuromuscular blockade. After extubation patients were shifted to post anaesthesia care unit. Pain assessment was done by using VAS. Postoperative block assessment was done at 0 hour in post anaesthesia care unit then 2 hourly intervals up to 8 hours followed by 4 hourly intervals up to 24 hours. Patient with (VAS ≥4) were given rescue analgesic injection diclofenac 1.5 mg/kg (max75mg i/m). The duration of both sensory and motor blockade and duration of analgesia (first request of an analgesic) was recorded by interviewing the patient in the postoperative period. The duration of sensory blockade was time interval between the onset of sensory blockade and the first post operative rescue analgesic (VAS Score ≥4). The duration of motor blockade was time interval between the onset of motor blockade and complete recovery of motor functions.
The time of administering first rescue analgesia and the cumulative consumption of rescue analgesics was recorded during the first postoperative 24 hours. All the patients were observed perioperatively and postoperatively.
Primary outcome of the study was the onset and duration of interscalene block and secondary outcomes were the haemodynamic parameters, postoperative VAS scores, time to first rescue analgesic and the cumulative dose of rescue analgesics in first 24 hours postoperatively.
Statistical Analysis
The data of the study was recorded in the chart and results were evaluated using statistical tests (Student’s t-test and chi-square test whichever was applicable) with SPSS software version 23.0.
Results
Demographic data (age, sex, weight, duration of surgery) and baseline parameters were comparable between both the groups (p>0.05) [Table/Fig-2].
| Group I Mean±Sd | Group II Mean±Sd | p-value |
|---|
| Age (years) | 39.27±13.28 | 41.23±12.05 | 0.550 |
| Weight (kg) | 60.37±7.12 | 61.73±6.00 | 0.425 |
| Duration of surgery (min) | 119.50±11.47 | 118.0±12.29 | 0.627 |
| Sex | Female | 10 | 8 | 0.78 |
| Male | 20 | 22 |
p>0.05=not significant, p<0.05=significant (*), p<0.00=highly significant (**)
The mean time of onset of sensory blockade (minimum Grade 2 by Hollmen’s scale) was comparable between Group I and Group II (p>0.05). The mean time of onset of motor block (minimum Grade 2 by modified bromage scale) in Group I was also comparable to Group II (p>0.05) [Table/Fig-3].
Comparison of block characteristics between the two groups.
| Group I Mean±Sd | Group II Mean±Sd | p-value |
|---|
| Mean onset time for sensory block- GRADE 2 (in min) | 6.56±0.306 | 6.68±0.280 | 0.128 |
| Mean onset time for motor block- GRADE 2 (in min) | 7.81±0.291 | 7.92±0.289 | 0.153 |
| Mean duration of sensory block (min) | 759.93±63.93 | 568.37±50.87 | <0.001** |
| Mean duration of motor block (min) | 350.17±14.35 | 300.27±20.89 | <0.001** |
| Mean duration of analgesia (min) | 759.93±63.93 | 568.37±50.87 | <0.001** |
| No. of rescue analgesics in 24 hours | 1.83±0.379 | 2.60±0.498 | <0.001** |
p>0.05=not significant, p<0.05=significant (*), p<0.00=highly significant (**)
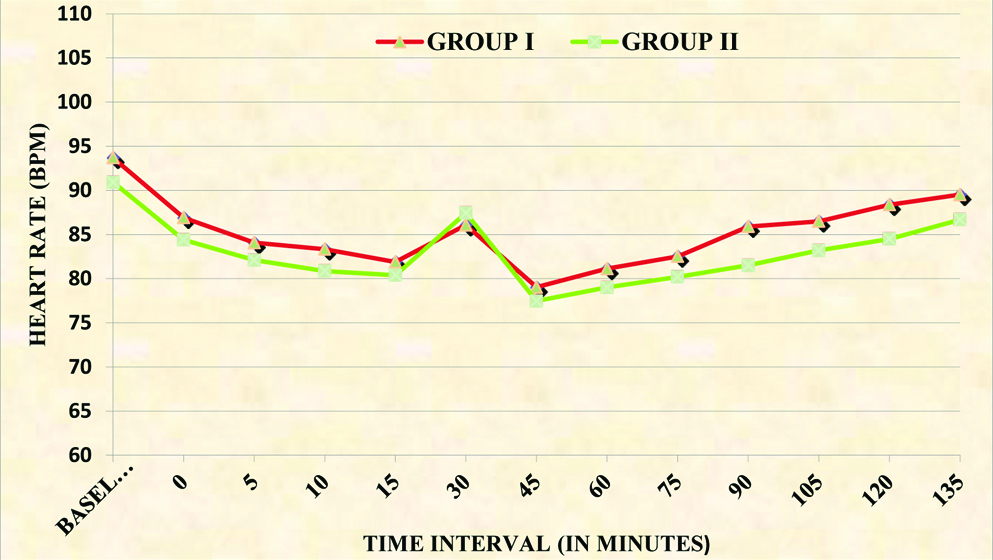
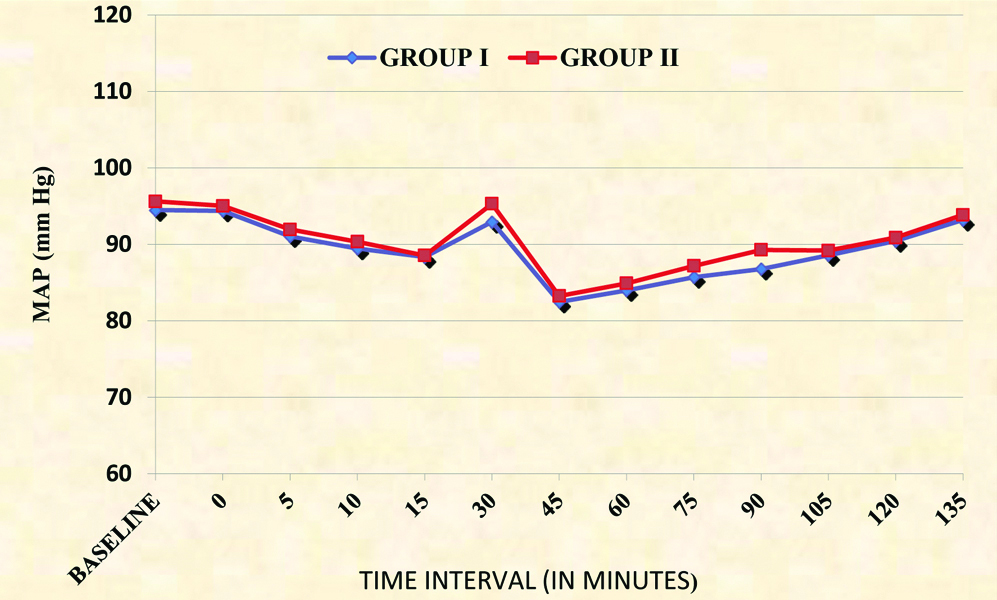
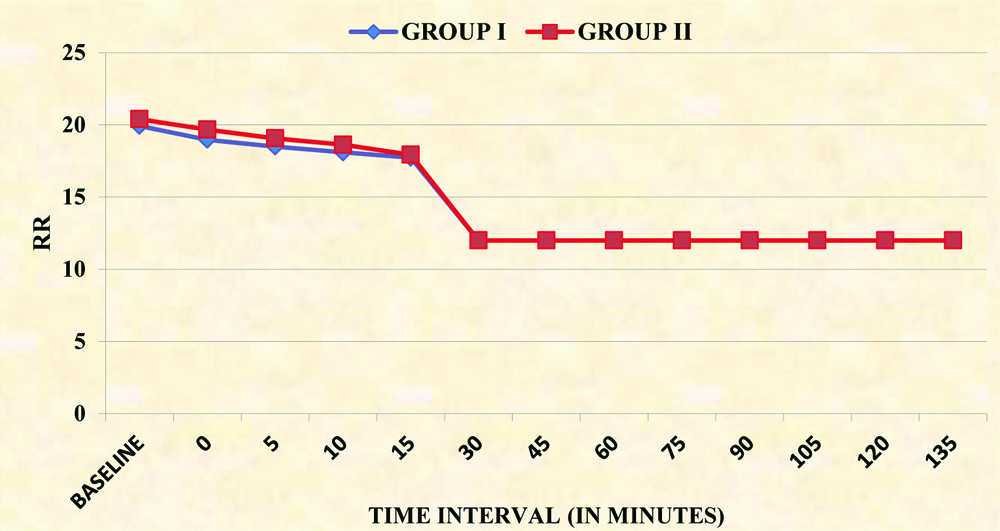
Haemodynamic parameters were comparable between the two groups [Table/Fig-4,4,5 and 6]. The mean duration of sensory block in Group I was significantly more as compared to Group II (p<0.001). The mean duration of motor block was significantly more in Group I as compared to Group II (p<0.001). The mean duration of analgesia in Group I was also longer than in Group II (p<0.001) [Table/Fig-3].
Intergroup comparison of heart rate (bpm).
Intergroup comparison of Mean Arterial Pressure (MAP).
Intergroup comparison of Respiratory Rate (RR).
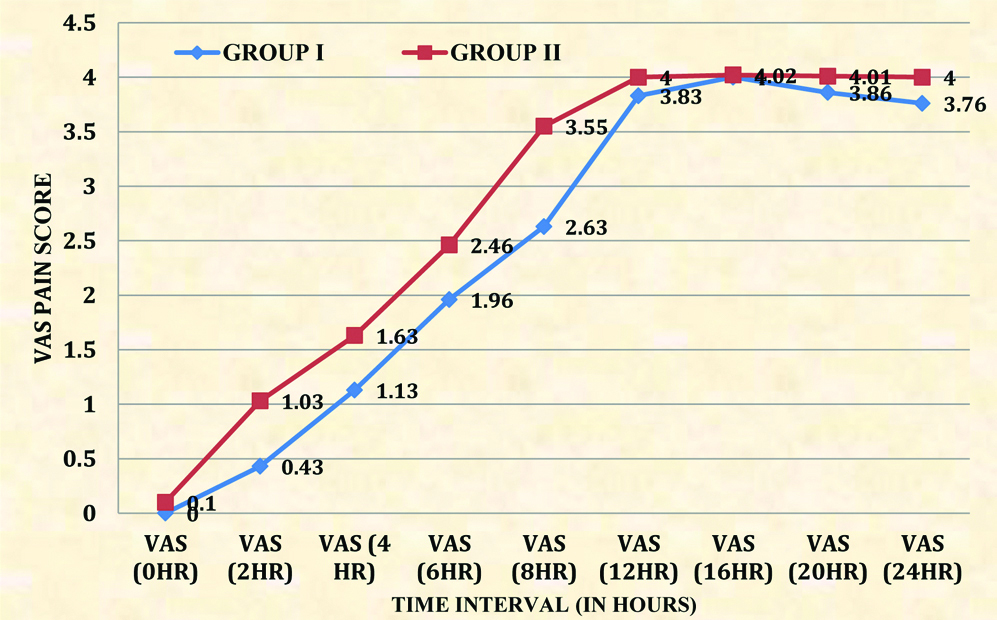
Postoperative VAS scores were significantly less in group I as compared to group II [Table/Fig-7]. The number of rescue analgesics required in first 24 hours in Group I was significantly less than the Group II [Table/Fig-3].
Intergroup comparison of Visual Analogue Scale (VAS).
Discussion
In this study, the effect of MgSO4 250 mg as an adjuvant to 20 mL of 0.5% bupivacaine was compared with saline in interscalene block. The block was supplemented with general anaesthesia. Grossi P et al., also suggested that supplementing interscalene block with general anaesthesia avoids the stress experienced by the patient who is awake while undergoing surgery [10]. Brachial plexus block, when used in combination with general anaesthesia, has been shown to reduce intraoperative anaesthetic and postoperative analgesic requirement [11,12].
In this study, 20 mL of local anaesthetic was used, which was in accordance to the volume of drug used in various studies on ultrasound guided interscalene brachial plexus block for providing preoperative anaesthesia and analgesia [13,14]. Higher volume of local anaesthetic for interscalene block was associated with increased incidence of complications like horner’s syndrome, phrenic nerve paralysis, recurrent laryngeal nerve block as proved in various studies [15,16]. In these studies, 30-40 mL of local anaesthetic volume was used.
In the present study, the dose of 250 mg of MgSO4 was used in accordance to study done by Reddy KN et al., [17]. Various studies have shown that low dose [18,19] of MgSO4 (150 mg, 200 mg) has resulted in delayed block onset and high dose [20,21] of MgSO4 (500 mg, 600 mg) either didn’t alter or delayed the rapidity of block onset or insignificantly hastened the onset of block. Therefore we used the dose of 250 mg MgSO4 in our study owing to unpredictable effect of MgSO4 in different doses.
The time to onset of sensory and motor block was comparable in this study (p>0.05) which was similar to a studies done by Lee AR et al. and Fahmy NG et al., [18,21]. Time of onset of sensory block was between 14-16 minutes in these studies whereas it was 6-8 min in the present study for grade 2 hollman and modified bromage scale. Onset of grade 3 block in this study was also at 10-15 min interval. The results of this study were not concurrent with those of Klein SM et al., and Casati A et al., [22,23]. Klein SM et al., had reported shorter onset of less than 6 minutes but they had used larger volume (30 mL) of the drugs with freshly prepared ephinephrine and used premedication with midazolam (1-5 mg) and fentanyl (50-250 micrgram) in their patients [22]. Casati A et al., reported longer onset of blocks (22-28 minutes) as they had not used ultrasound but had used nerve stimulators [23].
The duration of sensory and motor block was significantly prolonged in the group receiving MgSO4 as an adjuvant in the present study. Various other studies also found statistically significant prolonged duration of sensory and motor block on addition of MgSO4 to different local anaesthetics in various techniques for brachial plexus blocks [18-21]. Choi IG et al., did not find any prolongation of analgesia in patients getting axillary block with ropivacaine and 200 mg MgSO4 than the saline group and this could be because of the axillary block with less volume of ropivacane by blind trans-arterial technique and also as they had used 200 mg of MgSO4 [24].
In this study, there was statistically significant difference in VAS scores postoperatively. The number of rescue analgesics required in first 24 hours was significantly less in the group receiving MgSO4 as an adjuvant to local anaesthetic.
MgSO4 as an adjuvant may be used to decrease the dose of local anaesthetics in peripheral nerve blocks so as to decrease their toxicity. Further research is desirable to find out the optimal dose of MgSO4 by comparing different doses with minimum side effects. Moreover, a longer postoperative follow-up should be advocated so as to rule out any long term side effects of using MgSO4 in interscalene block.
Limitation
General anaesthesia was given to all the patients after 15 minutes of the interscalene block. So we could not assess for the partial effect intraoperatively. Postoperative analysis could have been for longer time to see for the long term complications of the block and the side effects of MgSO4.
Conclusion
To conclude, the use of MgSO4 (250 mg) as an adjuvant to 20 mL 0.5% bupivacaine in ultrasound guided interscalene brachial plexus block significantly prolonged the duration of sensory blockade, motor blockade and duration of analgesia. It significantly decreased the requirement of rescue analgesics in first 24 hours. Hence, we strongly recommend the addition of MgSO4 (250 mg) as an adjuvant to 0.5% bupivacaine in interscalene block.
p>0.05=not significant, p<0.05=significant (*), p<0.00=highly significant (**)
p>0.05=not significant, p<0.05=significant (*), p<0.00=highly significant (**)