Ideal methods of skin incision which provide quick and adequate exposure with minimal blood loss are being studied by surgeons. To demonstrate the safety and efficacy of diathermy for dividing subcutaneous, muscular and fascial layers numerous human studies have been performed [1]. Diathermy is increasingly being used for tissue dissection; however, its extensive use for skin incisions was curtailed because of poor wound healing and excessive scarring [2]. Stainless steel scalpels are used to make incisions traditionally. These incisions are bloody and painful. Many advanced techniques like laser, plasma scalpel, cavitron surgical aspirator etc., have been used to minimise surgical blood loss but the above mentioned methods are costly and unavailable at peripheries.
Cutting diathermy is commonly used by many surgeons to make skin incisions without a scalpel and to divide the deeper tissues. Diathermy is less often used for skin incisions due to the fear of tissue damage, increase in infection rates, scarring and postoperative pain. Nevertheless; it is frequently used by some surgeons for skin incisions. To evaluate the efficacy of diathermy over scalpel in making skin incision, various studies have been undertaken and the results vary [3-7].
The use of diathermy has become ubiquitous in the majority of surgical specialities for its convenience and advantages with respect to haemostasis and sharps safety. However, its use for incising epidermis and dermis of the skin remains controversial because of the fear of thermal burns, resulting in a scar that is cosmetically inferior to that resulting from the use of a scalpel. Skin incisions taken with diathermy prevent postoperative complications such as pain, wound infection, and scarring [4,8-10]. Charring and necrosis are very little in incision taken by cutting diathermy than coagulation diathermy [8].
The present study was undertaken to compare the cosmetic outcome of cutting diathermy against scalpel for skin incision during Elective Abdominal Surgery.
Materials and Methods
Patients between age of 18 and 60 years and both sexes, admitted in Poona Hospital and Research Centre between July 2017 and October 2018, were selected. They were scheduled for elective open abdominal clean procedures and consented to participate in the study after explaining potential advantages, and risks. Permission was obtained from Ethics Committee (Letter No: RECH/EC/2017-18/375) and Scientific Advisory Committee (Letter no: RECH/SAC/2017-18/374) of the institution for this randomised study.
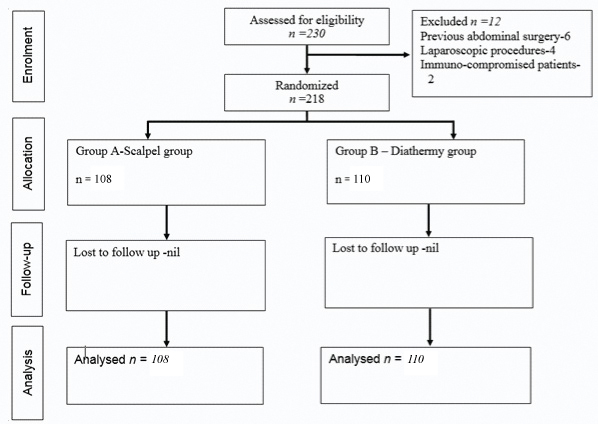
Exclusion criteria were immuno-compromised patients, patients undergoing laparoscopic procedures, emergency operative procedures, patients who had undergone previous open abdominal surgery, patients on anti-coagulant therapy, and contaminated surgeries. Based on a previous study [11], setting an alpha error at 0.05, and power at 80%, sample size of 70 patients for each group was calculated by a formula [12]. Patients were randomised for skin incision using random number tables into two groups; Group A (n=110)- Scalpel group and Group B (n=108)-Cutting diathermy group [Table/Fig-1].
Detailed history of the patient was taken and complaints were recorded. Clinical examination was done. Relevant preoperative investigations were done as mentioned in the pre-tested study proforma.
All procedures were carried out under general or spinal anaesthesia. All patients received standard prophylactic antibiotic prior to surgery. Just prior to skin incision, an envelope containing type of incision was opened by the senior operation theatre nurse. Patient and observer were unaware of the type of the incision taken. In Group A, skin (epidermis+dermis) was incised with scalpel and haemostasis was achieved by coagulation diathermy. In Group B, skin (epidermis + dermis) was incised with cutting diathermy using pure sine wave current and a power setting of 25 watts. Haemostasis was achieved by coagulation diathermy. The subcutaneous and fascial layers were incised using diathermy in both the groups. For each surgery type, the standard incision was taken. (e.g., Rocky Davis for Appendectomy, Midline for Laparotomy, Kocher for Open Cholecystectomy). All the surgeries performed were clean. There was no spillage of abdominal contents in wound. Method of closure was the standard for each surgery type. All incisions were closed with monolayer closure and skin with 3-0 interrupted suture.
Postoperative wound pain was measured using VAS score after 6, 12, 24 and 48 hours. For VAS score >4, injection diclofenac sodium 75 mg intramuscular or paracetamol 1 gm intravenous was given. For seven days post-surgery wound complications such as seroma (collection of serous discharge in suture site), haematoma (collection of blood clots) and abscess (collection of purulent material) were noted. At periods of 1, 3 and 6 months after surgery, patient’s surgical scars were evaluated by using POSAS [13]. Primary outcome measures were scar cosmesis at 1, 3 and 6 month intervals using POSAS whereas, secondary outcome measures were postoperative pain using VAS score, and postoperative complications.
Statistical Analysis
Data on categorical variables are shown as n (% of cases) and the data on continuous variables are presented as mean and SD. The inter-group comparison of categorical variables was done using chi-square test or Fisher’s-exact test. The statistical significance of inter-group difference of means of continuous variables was tested using unpaired t-test. The underlying normality assumption was tested before statistical analysis. The p-values <0.05 were considered to be statistically significant. Data were statistically analysed using Statistical Package for Social Sciences (SPSS version 21.0, IBM Corporation, USA) for MS Windows.
Results
A total of 218 patients were included in the study; 108 were allocated to scalpel and 110 to diathermy group, randomly. There was no statistically significant difference in mean age, gender and type of surgery distribution between the two groups [Table/Fig-2]. The distribution of mean VAS score at 6, 12, 24, and 48 hours was significantly higher in Group A (scalpel) compared to Group B (diathermy). The distribution of mean total score of POSAS patient scale and mean total score of POSAS observer scale at 1 month and 3 months was significantly higher in Group B (diathermy) compared to Group A (scalpel), whereas mean total score of POSAS patient scale and mean total score of POSAS observer scale at 6 months did not differ significantly between two study groups [Table/Fig-3]. The distribution of mean overall score of POSAS patient scale at 1 month, 3 months and 6 months did not differ significantly between the two study groups. The distribution of mean overall score of POSAS observer scale at 1 month and 3 months was significantly higher in Group B (diathermy) compared to Group A (scalpel), whereas mean overall score of POSAS observer scale at 6 months did not differ significantly between the two study groups [Table/Fig-3]. The distribution of overall incidence of postoperative complications did not differ significantly between the two study groups.
Characteristic of patients at baseline.
| Characteristics | Group A (n=108) | Group B (n=110) | p-value |
|---|
| Age in years (mean±SD) | 43.5±11.9 | 41.5±12.1 | 0.220 * |
| Gender (%) | 0.203** |
| Male | 67 (62.0) | 67 (60.9) |
| Female | 41 (38.0) | 43 (39.1) |
| Type of procedure (%) |
| Appendectomy | 10 (9.3) | 11 (10.0) | 0.344*** |
| Hernia repair | 49 (45.4) | 45 (40.9) |
| Open cholecystectomy | 7 (6.5) | 10 (9.1) |
| Laparotomy | 20 (18.5) | 30 (27.3) |
| Other | 22 (20.4) | 14 (12.7) |
*Unpaired t-test was used; **Chi-square test was used; ***Fisher’s-exact test was used
| Characteristics | Group A (n=108) | Group B (n=110) | p-value |
|---|
| VAS score (mean±SD) |
| 6 hour | 5.7±1.2 | 3.9±1.3 | 0.001* |
| 12 hour | 6.2±1.6 | 4.4±1.4 | 0.001* |
| 24 hour | 6.4±1.6 | 3.8±1.5 | 0.001* |
| 48 hour | 5.0±1.6 | 3.2±1.1 | 0.001* |
| POSAS patient scale (Total out of 60, mean±SD) |
| 1 month | 23.4±3.8 | 25.5±4.3 | 0.001* |
| 3 months | 21.7±3.0 | 22.6±3.2 | 0.037* |
| 6 months | 20.3±2.7 | 20.5±2.9 | 0.539* |
| POSAS patient scale (Overall out of 10, mean±SD) |
| 1 month | 3.5±0.85 | 3.7±0.76 | 0.080* |
| 3 months | 3.1±0.75 | 3.1±0.64 | 0.845* |
| 6 months | 2.8±0.67 | 2.8±0.67 | 0.680* |
| POSAS observer scale (Total out of 60, mean±SD) |
| 1 month | 21.7±3.0 | 25.0±3.9 | 0.001* |
| 3 months | 20.7±2.7 | 21.7±3.1 | 0.010* |
| 6 months | 19.2±2.6 | 19.6±3.2 | 0.295* |
| POSAS observer scale (Overall out of 10, mean±SD) |
| 1 month | 2.9±0.73 | 3.8±0.7 | 0.001* |
| 3 months | 2.9±0.63 | 3.2±0.59 | 0.001* |
| 6 months | 2.7±0.60 | 2.8±0.59 | 0.174* |
| Postoperative complications (%) |
| Nil | 98 (90.7) | 103 (93.6) | 0.777** |
| Haematoma | 2 (1.9) | 1 (0.9) |
| Seroma | 5 (4.6) | 5 (4.5) |
| Infection | 2 (1.9) | 1 (0.9) |
| Dehiscence | 1 (0.9) | 0 (0.0) |
POSAS: Patient and observer scar assessment scale; VAS: Visual analogue scale; *Unpaired t-test was used; **Fisher’s-exact test was used
Discussion
The present study was conducted to compare cosmetic outcome, postoperative pain and wound complications between skin incision taken by scalpel and cutting diathermy.
Patients included in both groups were aged between 18 and 60 years. Age factor was comparable with previous study in which Chauhan HR and Charpot RV, reported age ranged from 16 to 73 years with a mean of 46±14.9 years [14].
In the present study, the mean VAS score at 6, 12, 24 and 48 hours was significantly higher in scalpel group compared to diathermy group. Lower mean VAS score in diathermy group was also reported by a previously conducted study [9]. Thermal effect of diathermy on sensory nerve fibers causes disruption of transmission of nerve impulses. This may be the reason for lower mean VAS score in diathermy group. Diathermy causes total or partial injury of cutaneous nerves localised on the incision causing diminished postoperative pain [9]. Kearns S et al., stated that diathermy produced significantly less postoperative pain on the first and second postoperative day when compared to scalpel incisions [4]. Chalya PL et al., reported significantly reduced mean VAS score with diathermy incision as compared to scalpel incision on postoperative day one (p=0.001), two (p=0.011) and three (p=0.021) [15]. Prakash LD et al., stated that there was no significant difference in postoperative pain between diathermy incision and scalpel incision group [16]. A comparative randomised controlled clinical trial of diathermy versus scalpel incision reported that there was no significant difference in postoperative pain assessed by VAS at 1, 3, 5,7,10 days after surgery between two groups. They further stated that there was no statistically significant difference in postoperative wound infection assessed by presence of redness, pus discharge, or seroma at 1, 3, 5, 7, 10 days after surgery between two groups [17]. According to Okereke CE et al., cutting diathermy or scalpel technique when used for the patients who underwent open appendectomy for uncomplicated acute appendicitis, there was no significant difference with respect to post-operative pain, wound infection and surgical scar cosmesis in either group [18]. Priya N et al., stated that diathermy is better than scalpel as diathermy provided some benefit with respect to postoperative wound pain and safety [10].
In the present study, mean total POSAS patient scale was significantly higher in diathermy group at 1 month (p= 0.001) and 3 months (p=0.037). Mean total score of POSAS observer scale at 1 month (p=0.001) and 3 months (p=0.01) was significantly higher in diathermy group as compared to scalpel group. Mean overall POSAS observer scale was also higher in diathermy group at 1 month (p=0.001) and 3 months (p=0.001). Chau JK et al., reported that there was no significant difference in mean POSAS scale or patient’s overall satisfaction score (p=0.518). Similarly, no significant differences in objective assessment were noted between scalpel and diathermy incision group at 6 months postoperatively (p=0.732) [19]. These findings are comparable to the index study. Aird LN and Brown CJ, reported in their meta-analysis that no significant difference was noted in scar cosmesis or wound infection rates between the two groups [1]. Aird L et al., conducted a study on 66 patients and found no statistically significant difference between the diathermy and scalpel groups with respect to mean VAS scores (4.9 vs 5.0; p=0.837), mean POSAS total scores (19.2 vs 20.0; p=0.684), subjective POSAS total scores (20.2 vs 21.3); p=0.725), and wound infection rates (5 of 30 versus 5 of 32; p=1.000) at 6 months follow-up. However, pain scores on day 1 after operation were significantly lower in the diathermy group (mean 1.68 vs 3.13; p = 0.018), but there was no statistically significantly difference in pain scores between the two groups from days 2 to 5 [11].
If thermal energy is used for skin incision, there may be concerns regarding collateral heat damage. This may lead to impaired wound healing, necrosis at wound edges leading to wound infection [8,20]. In our study, incidence of wound infection in the scalpel group was 1.9% whereas, in the diathermy group, it was 0.9% (p>0.05). Similar finding were reported by previous studies [3,15,21]. Ragesh KV et al., reported that postoperative infection rates were comparable in diathermy and scalpel group of patients [22]. Due to minimal charring and necrosis when using diathermy, rate of infection is not higher in diathermy incision as compared to scalpel [3]. However, few studies conducted in the past reported increased rate of wound infection in the diathermy group [8,23-26]. Stupart DA et al., noted cosmetically equivalent results of cutting diathermy and scalpel to make abdominal skin incisions. They further recommended the routine use of cutting diathermy for skin incisions in abdominal surgery [27]. Complication rates between the two groups showed no statistically significant difference.
Limitation
Sample size was small. Further research should be conducted at multiple sites with larger sample size. Follow-up period was of 6 months only and factors such as diabetes mellitus, haemoglobin %, body mass index were not taken into consideration.
Conclusion
Scalpel group patients showed significantly higher Mean VAS score as compared to the diathermy group. Mean total score of POSAS patient scale, mean total score of POSAS observer scale, and mean overall score of POSAS observer scale at 1 month and 3 months were significantly higher in the diathermy group compared with the scalpel group, but they did not differ significantly at 6 months.
*Unpaired t-test was used; **Chi-square test was used; ***Fisher’s-exact test was used
POSAS: Patient and observer scar assessment scale; VAS: Visual analogue scale; *Unpaired t-test was used; **Fisher’s-exact test was used