Lymphangiomas are benign tumours of the lymphatic vessels usually occurring in the head-neck region and axillary region, frequently affecting children and young adults. Most of the lymphangiomas are congenital. Lymphangiomas affecting abdominal organs are uncommon, of which pancreatic involvement is one of the rarest and seen in <1% cases. The cystic lesions commonly affecting the pancreas are pseudocysts, simple cysts, serous cystadenomas, Mucinous Cystic Neoplasms (MCNs), Intraductal Papillary Mucinous Neoplasms (IPMNs) and cystic pancreatic carcinomas. There are less than a hundred cases described in literature till date, with less than 10 cases reported from India. Here, the present authors report a rare case of cystic lymphangioma of the pancreas in an adult and describe its morphological characteristics and diagnostic modalities which help in differentiating it from other cystic lesions of the pancreas.
Lymphatic vessels, Lymphatic cyst, Pancreatic cyst
Case Report
A 45-year-old female presented in the outpatient department with complaint of abdominal pain of one year duration. The pain was intermittent and dull aching type with a dragging sensation. The pain was of mild to moderate intensity and was localised in the left hypochondrium with radiation towards the left lumbar region. She also complained of early satiety. There was no history of any fever, jaundice, vomiting, diarrhoea, weight loss, mucocutaneous bleed or haematuria. On clinical examination, there was an intrabdominal lump in the upper left quadrant that moved with change of posture. There was no associated hepatosplenomegaly. Abdominal tenderness and rebound tenderness of the whole abdomen were obvious. Initial laboratory findings revealed mild leukocytosis (11,300/Cumm) with neutrophilic predominance (82% of the leukocytes). Biochemical parameters including liver function test, lipid profile and serum amylase and lipase levels were within normal limits. Serum CEA and CA19-9 levels were also normal. An Ultrasound (USG) examination done elsewhere suggested a large hypoechoic pancreatic cystic mass measuring 15 cm × 12 cm. However, the USG plates were not available for review. The clinico-radiological differential diagnoses were serous cyst, mucinous cystic neoplasm and pancreatic pseudocyst.
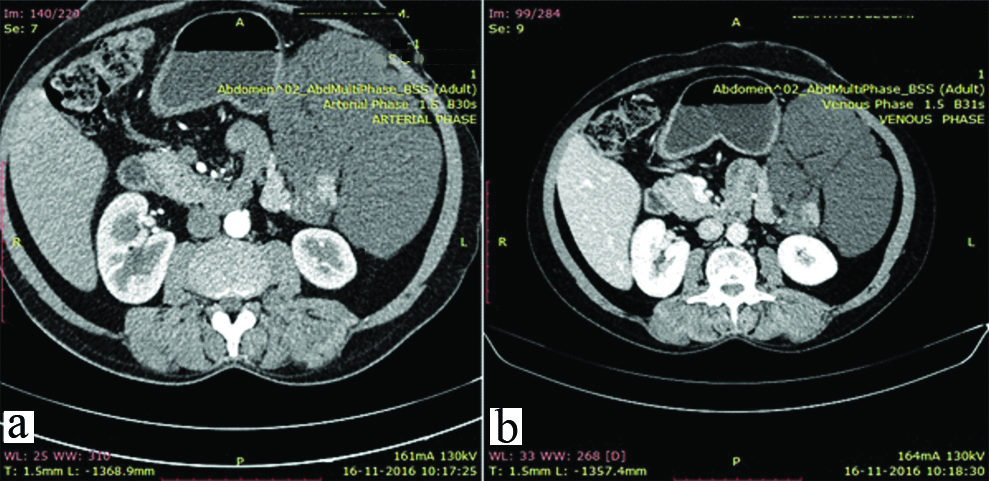
Subsequently, she was admitted to the Department of Gastro-Intestinal Surgery. During her hospitalisation, a contrast enhanced CT scan was performed which showed a large homogenously lobulated hypodense cystic mass without contrast enhancement in left upper quadrant, measuring 16 cm × 13 cm × 8 cm and encasing the tail of pancreas [Table/Fig-1]. The cystic mass contained hyperattenuating fluid. CT-guided aspiration was done and 5 mL of cyst fluid was taken out, which was straw clear in appearance. Microscopic examination showed only lymphomononuclear cells in the cystic fluid. PAS staining for mucin was negative. The possibility of a serous cyst or a pseudocyst was considered. Thereafter, the patient underwent laparotomy and on intraoperative exploration, there was a huge multilobulated cystic Space Occupying Lesion (SOL) arising from the distal part of body and tail of pancreas and extending through the mesocolon into the infracolonic compartment, pushing the stomach superiorly. The cyst also appeared to involve the hilum of the spleen. Rest of the pancreas was normal. There was no splenomegaly, ascites or any gross peritoneal deposit. En block excision of the cystic mass was done with distal pancreatectomy and splenectomy. The head of the pancreas and proximal part of the body was spared to retain the pancreatic secretory function.
CT scan showing a large homogenously lobulated hypodense cystic mass containing hyperattenuating fluid and without contrast enhancement in left upper quadrant, encasing the tail of pancreas; (a) Arterial phase, (b) Venous phase.
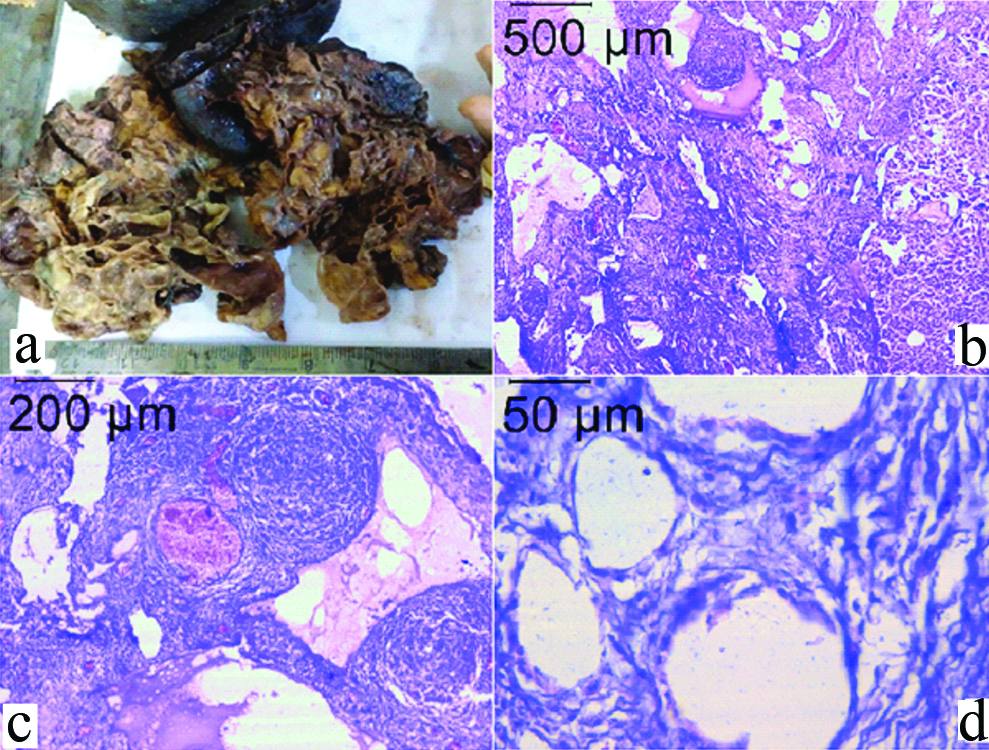
On gross examination, there was a multilobulated cystic mass measuring 17 cm × 14 cm × 8 cm, composed of multiple cysts of varying sizes arising from the distal part of the pancreas, and densely adhered to the spleen. The cyst wall was thin with thickness varying from 0.2 to 0.4 cm. The cysts contained straw coloured fluid. The distal pancreas measured 3.8 cm × 2.8 cm × 2.5 cm. The spleen was grossly unremarkable. On microscopic examination, the lesion showed numerous thin walled cysts of variable sizes and ectasia of the lymphatic vessels. All the cysts were lined by flattened endothelial cells and none of them had any epithelial lining anywhere. The cysts were associated with numerous reactive lymphoid follicles and cholesterol clefts along the wall of the cysts [Table/Fig-2a-d]. The rest of the distal pancreas and spleen were histologically within normal limits. So, a final diagnosis of cystic lymphangioma of pancreas was made. Post-operative recovery of the patient was uneventful. The patient has been doing fine on one year follow-up.
(a) Gross appearance of the multilobulated cystic mass densely adhered to the spleen, (b) Photomicrograph showing multiple cysts within the pancreatic parenchyma; part of normal pancreas is seen in the right, H&E-4x (c) Cysts were associated with numerous reactive lymphoid follicles, H&E-10x (d) Cysts were lined by flattened endothelial cells and none of them had any epithelial lining anywhere, H&E-40X.
Discussion
Lymphangiomas are slow-growing cystic lesions arising from lymphatic channels and mostly affecting children and young adults with a female predominance [1]. Majority of these lesions are found in the head-neck region (75%) and axilla (20%), with other uncommon sites of involvement being pleura, pericardium, groin, bones, liver, spleen, colon, omentum, and genital organs. Lymphangiomas arising from or in relation to the pancreas comprise less than 1% of all Lymphangiomas [2]. The first case of pancreatic lymphangioma was reported by Koch K, in 1913 as a form of benign cyst secondary to blocked regional lymphatic ducts [3]. However, since then, to the best of our knowledge, less than only hundred cases have been reported so far in literature with less than ten cases being reported from India [2,4]. The summary of all the cases of pancreatic lymphangioma reported from India has been summarised in [Table/Fig-3] [4-9].
Summary of cases of pancreatic lymphangioma reported from India.
| Authors | Year | Age (yrs) | Sex | Anatomical location | Greatest dimension (cm) | Clinical treatment |
|---|
| Lyngdoh TS et al., [5] | 2008 | Middle aged | F | Tail | 32.0 | Cystectomy |
| Ghatak S et al., [6] | 2011 | 20 | M | Head | 50.0 | Whipple’s Pancreato-duodenectomy |
| Bhatia V et al., [7] | 2011 | 20 | F | Tail | 8.0 | Cystectomy |
| Suhani et al., [8] | 2014 | 22 | F | Tail | 22.0 | En-bloc excision of cyst |
| Bihari C et al., [9] | 2016 | 26 | F | Body | 5.0 | Laparoscopic Cystectomy |
| Jayappa SN et al., [4] | 2018 | 54 | F | Tail | 21.6 | Distal pancreatectomy with Splenectomy |
| Halder et al.,* | 2019 | 45 | F | Tail | 16.0 | Distal pancreatectomy with Splenectomy |
*The present case has been included in this table [4-9].
Pancreatic lymphangiomas clinically manifest with various nonspecific symptoms, like vague abdominal pain, abdominal discomfort, dyspepsia and a palpable lump, due to the different sizes and locations of Lymphangiomas [10]. However, in some cases lymphangiomas may be symptomless and discovered as an incidental finding [2]. In the present case, the patient complained of a vague abdominal pain of around one year duration. The average size of pancreatic lymphangiomas is around 12 cm in greatest dimension [4], but in the present case the lesion was fairly large with the greatest dimension being 17 cm.
Common cystic lesions of the pancreas which should be differentiated from lymphangiomas include pancreatic pseudocysts, simple cysts, serous cystadenomas, mucinous cystic neoplasms, intraductal papillary mucinous neoplasms and cystic pancreatic carcinomas. Imaging findings may aid in preoperative diagnosis of intra-abdominal lymphangiomas, although none of the findings are diagnostic [4]. On USG, lymphangioma appears as a complex cystic mass with internal septa or internal echoes, with or without intracystic calcifications. CT scan findings usually show a thin-walled, low-density, uni or multil-oculated cystic mass with thin enhancing endocystic septae [2]. However, these findings will also be seen in pancreatic cystadenomas which are clinically far more common than lymphangiomas. Pancreatic pseudocysts are usually a sequel of acute or chronic pancreatitis, the findings of which will be reflected in USG or CT imaging. None of these changes were present in the present case and hence the possibility of pseudocyst was not considered. IPMNs may appear cystic but usually have a communication with the main pancreatic duct, which was absent in the present case. On MRI, cystic lymphangiomas appear hypodense on T1-weighted images and hyperintense on T2-weighted images. Moreover, MRI is more useful than CT to exclude any communication between the cystic lesion and the pancreatic duct [2]. Endoscopic Ultrasound (EUS) has recently come-up as a first-line procedure for the diagnosis of pancreatic lesions. EUS has a high sensitivity in periampullary or pancreatic head lesions, but for lesions located in the distal body or the tail of pancreas, its sensitivity may decrease. However, the origin of lymphangiomas is difficult to determine by imaging [11].
Image guided aspiration of the cyst fluid may suggest the nature of the cyst. Aspiration of simple cysts, serous cysts/cystadenomas or lymphangiomas usually yield clear thin yellowish or straw coloured fluids, composed of lymphomononuclear cells as in the present case. Aspirates from MCNs or IPMNs will yield mucin, which can be identified grossly as well as microscopically using mucin stains like PAS. Mucin staining of the aspirated fluid was done in the present case and was found to be negative. In addition, aspirates from MCNs and IPMNs will yield variable number of columnar epithelial cells with intracytoplasmic mucin, arranged in clusters, papillae or singles, with or without cytological atypia. Cystic carcinomas of pancreas will show cytomorphological malignant cells arranged in papillae, clusters or acinar pattern [2,4,11].
Histopathological examination will correctly help in differentiating cystic lymphangiomas from other cystic lesions of the pancreas. The gross appearance of cystic lymphangiomas are usually soft multiloculated masses containing serous or sero-sanguinous fluid. The cyst walls are usually thin without any solid areas. Histologically, dilated lymphatic channels of varying sizes are seen, separated by thin septae and intimately intermingled with the pancreatic parenchyma [4]. The cystic spaces are lined by flattened endothelial cells. Aggregates of lymphocytes may be found within the cyst lumen or adjacent stroma in cases of Lymphangiomas [2,4]. The present case showed all these characteristic findings along with numerous lymphoid follicles and cholesterol clefts within the stroma. Unlike lymphangiomas, pancreatic pseudocysts do not have any epithelial or endothelial lining and are lined by inflammatory granulation tissue. Multiloculated serous cysts or cystadenomas are usually lined by flattened cuboidal cells and do not show lymphocytes within the cyst lumen.
The treatment of choice in cystic lymphangioma is surgical resection and different options may be considered, including simple excision of the cyst, pancreatic resection, such as Whipple procedure or distal pancreatectomy, depending on the morphology and size of the cysts [11]. En-bloc resection of the pancreatic lymphangioma is the treatment of choice, which was done in the present case. Aspiration of cyst content or partial cystectomy is not recommended as it may result in recurrences. With complete excision of the cyst, long term prognosis is excellent [4,6].
Conclusion
Pancreatic lymphangiomas are rare lesions of the pancreas which should be considered in the differential diagnosis of cystic tumors of the pancreas, especially in women. Radiological examination may help in narrowing the differential diagnoses and guided aspiration of cyst fluid may further help in this regard. Complete excision of the cyst is the treatment of choice in all cases.
*The present case has been included in this table [
4-
9].
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
PLAGIARISM CHECKING METHODS: [Jain H et al.]
Plagiarism X-checker: Jun 22, 2019
Manual Googling: Jul 17, 2019
iThenticate Software: Sep 12, 2019 (14%)
[1]. Kanzaki M, Kikkawa T, Obara T, Onuki T, Successful excision of an isolated mediastinal cystic lymphangioma with bilateral thoracoscopic surgeryAnn Thorac Cardiovasc Surg 2011 17:570-72.10.5761/atcs.cr.10.0154221881369 [Google Scholar] [CrossRef] [PubMed]
[2]. Viscosi F, Fleres F, Mazzeo C, Vulcano I, Cucinotta E, Cystic lymphangioma of the pancreas: A hard diagnostic challenge between pancreatic cystic lesions-review of recent literatureGland Surg 2018 7:487-92.10.21037/gs.2018.04.0230505770 [Google Scholar] [CrossRef] [PubMed]
[3]. Koch K, Beiträge zur Pathologie der BauchspeicheldrüseVirchows Arch Path Anat 1913 214:180-206.10.1007/BF01994867 [Google Scholar] [CrossRef]
[4]. Jayappa SN, Rao P, Tandon AS, Bharathy KGS, Sikora SS, Large cystic lympangioma of the pancreas: A case reportAnn R Coll Surg Engl 2018 100:e12-14.10.1308/rcsann.2017.017829046074 [Google Scholar] [CrossRef] [PubMed]
[5]. Lyngdoh TS, Konsam R, Th B, Marak B, Giant cystic lymphangioma of pancreasANZ J Surg 2008 78(8):673-74.10.1111/j.1445-2197.2008.04615.x18796026 [Google Scholar] [CrossRef] [PubMed]
[6]. Ghatak S, Ray S, Sanyal S, Sonar PK, Khamrui S, Basu K, An unusual cause of acute abdomen in adults: Giant cystic lymphangioma of the pancreatic head. A clinical case and literature reviewJOP 2011 12(3):266-70. [Google Scholar]
[7]. Bhatia V, Rastogi A, Saluja SS, Kumar M, Bihari C, Kalayarasan R, Gupta NL, Cystic pancreatic lymphangioma. The first report of a preoperative pathological diagnosis by endoscopic ultrasound-guided cyst aspirationJOP 2011 12(5):473-76. [Google Scholar]
[8]. Suhani , Aggarwal L, Ali S, Thomas S, Giant retroperitoneal lymphangioma: A rare entityIndian J Surg 2014 76(5):402-04.10.1007/s12262-013-0989-y26396474 [Google Scholar] [CrossRef] [PubMed]
[9]. Bihari C, Rastogi A, Rajesh S, Arora A, Arora A, Kumar N, Cystic lymphangioma of pancreasIndian J Surg Oncol 2016 7(1):106-09.10.1007/s13193-015-0414-z27065694 [Google Scholar] [CrossRef] [PubMed]
[10]. Kawaguchi K, Motoi F, Ohtsuka H, Fukuyama S, Rikiyama T, Katayose Y, Cystic lymphangioma of the pancreas with spontaneous rupture: report of a caseCase Rep Gastroenterol 2011 5:288-94.10.1159/00032694321712979 [Google Scholar] [CrossRef] [PubMed]
[11]. Chen D, Feng X, Lv Z, Xu X, Ding C, Wu J, Cystic lymphangioma of pancreas: A rare case report and review of the literatureMedicine (Baltimore) 2018 97(28):e1123810.1097/MD.000000000001123829995757 [Google Scholar] [CrossRef] [PubMed]