Challenges in Management of Misplaced Intrauterine Devices: A Case Series and Review of Literature
Alpana Singh1, Divya Chauhan2, Ayalur Gopalakrishnan Radhika3
1 Associate Professor, Department of Obstetrics and Gynaecology, University College of Medical Sciences, Delhi, India.
2 Senior Resident, Department of Obstetrics and Gynaecology, University College of Medical Sciences, Delhi, India.
3 Senior Specialist, Department of Obstetrics and Gynaecology, University College of Medical Sciences, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Divya Chauhan, 22-C, Pocket-A, SFS Flats, Mayur Vihar, Phase 3, Delhi, India.
E-mail: divyachauhan2009@gmail.com
Intrauterine Devices (IUD) have many advantages over other methods of contraception. At the same time, some complications may also occur. Missing string of IUD is a common problem and an IUD in uterus is easily removed by hysteroscopy. However, embedment of IUD in myometrium may pose challenges. Perforation of uterus by IUD is another serious complication. Hereby three such enlightening cases are presented.
Contraception, Embedment, Perforation
Introduction
IUD is a widely used method of contraception. It has many advantages over other contraceptive methods such as lack of hormonal side effects, high efficacy and long-lasting action. However, some serious complications have also been encountered with their use. Missing string of IUD can result from coiling or breakage of string, pregnancy, expulsion, embedding, uterine perforation and translocation of IUD [1]. Perforation poses management challenges. Removal of embedded IUD may also prove to be difficult.
Case 1
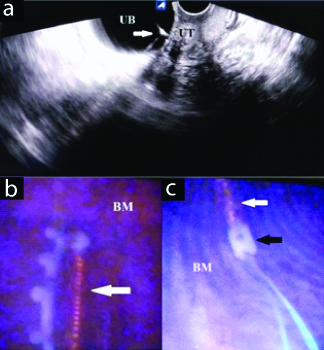
A 34-year-old woman, para 3 with all previous vaginal deliveries, came to emergency department with complaint of dysuria since IUD insertion. Interval IUD was inserted in government hospital 3 months back. She had undergone dilatation and curettage for unwanted pregnancy 6 weeks before IUD insertion. Immediately after insertion, she started having pain in lower abdomen and dysuria which had aggravated from past 15 days. On examination, she was haemodynamically stable. On abdominal examination, suprapubic tenderness was observed. Hypertrophied cervix with profuse curdy white discharge was noticed on speculum examination. Uterus was anteverted, normal size; both fornices were free. Ultrasonography revealed IUD in urinary bladder [Table/Fig-1a]. Uterine cavity was empty. Urine microscopy showed 8-10 pus cells per high power field along with budding fungal elements. Growth of non-albicans Candida species was observed on urine culture for which she was given oral fluconazole and clotrimazole vaginal pessary. On cystoscopy, bladder wall integrity was intact and IUD was removed with flexible forceps [Table/Fig-1b,c]. Postoperative period was uneventful.
a) Ultrasonography showing IUD (arrow) in Urinary bladder (UB) with empty Uterine cavity (UT); b) Cystoscopy showing Multiload 375 IUD (arrow) in urinary bladder; c) Cystoscopic removal of IUD (white arrow) using flexible forceps (black arrow).
BM: Bladder mucosa
Case 2
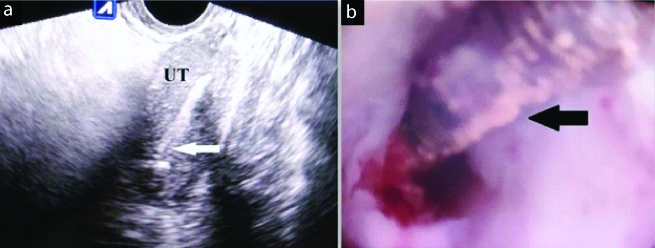
A 30-year-old woman, para 2, came to outpatient department after failed attempt at IUD removal at another hospital. She had 2 caesarean deliveries in the past and IUD was inserted postplacentally 6 years ago during last caesarean section. She desired to get her IUD removed as she wanted to conceive. She had no menstrual complaints. Her abdominal examination was normal. Speculum examination showed normal cervix and vagina with missing string. Vaginal examination was unremarkable. Ultrasound confirmed intrauterine presence of IUD [Table/Fig-2a]. On hysteroscopy, only stem and string of IUD were visualised; arms were not visible. Removal of IUD was attempted with the help of grasper but it failed as it was deeply embedded in the anterior uterine wall [Table/Fig-2b]. Laparotomy had to be done to remove the IUD. Intraoperatively, a lot of difficulty was encountered as a result of adhesions. The IUD was removed by hysterotomy.
a) Ultrasonography showing IUD (arrow) in Uterus (UT); 2b) Hysteroscopy showing deeply embedded IUD (arrow) in the anterior wall of uterus.
Case 3
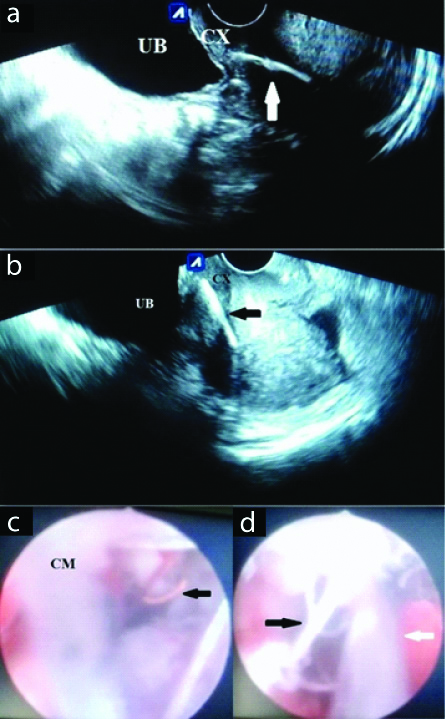
A 35-year-old para 2, with history of interval IUD insertion 7 years back, came for removal of IUD because of dyspareunia. She had regular menstrual cycles. On speculum examination, IUD string was not visible; cervix and vagina were healthy. Vaginal examination was suggestive of retroverted uterus of normal size. Both fornices were free and non-tender. Ultrasonography showed deeply embedded IUD in cervix, impending to perforate into the urinary bladder [Table/Fig-3a,b]. On hysteroscopy, it was found to be embedded in anterior wall of cervix at the level of internal os which was removed uneventfully [Table/Fig-3c,d].
a) transverse plane and b) sagittal plane shows: Ultrasonography showing IUD (arrow) embedded anteriorly in cervix (CX); C) Hysteroscopy showing embedded IUD (arrow); d) Hysteroscopic removal of embedded IUD (black arrow), white arrow: hysteroscope.
UB: Urinary bladder; CM: Cervical mucosa
Discussion
IUDs constitute 1.5% of contraceptive use in India [2]. They are highly efficacious, Long-acting Reversible Contraceptives (LARC). Other advantages which include one-time motivation, non-interference with sexual activity and absence of systemic side-effects.
Uterine perforation is a rare but serious complication of IUD. Its incidence is reported to be 1.6 per thousand insertions of copper IUD and 2.1 per thousand insertions of levonorgestrel IUD [3]. The incidence of uterine perforation is 1 per thousand copper IUD insertions in Guru Teg Bahadur Hospital (unpublished data). In a study which compared complication rates between postplacental and interval IUD insertions, no cases of uterine perforation were seen after 6 months of follow-up [4]. It results in severe abdominal pain but may be asymptomatic, remaining undetected for years. It is commonly detected during investigation of missing string [5].
Perforations can be of two types: complete and partial. When IUD passes through all the layers of uterus to lie freely in the peritoneal cavity or rarely, in other locations, it is called complete perforation. Pouch of Douglas is the commonest site of translocated IUD [5]. Complete perforation of uterus and urinary bladder was seen in the first case thereby resulting in intravesical location of IUD. Perforation of the urinary bladder is uncommon and leads to dysuria, increased frequency of micturition, suprapubic pain and hematuria. At least 40 cases of migration of IUD to the bladder have been reported in literature in last 10 years [6]. A case report revealed dyspareunia to be the major symptom of IUD migration to urinary bladder [6]. In this patient, the major symptom was pain in lower abdomen with dysuria.
In partial perforation, the IUD can be located within the uterine cavity with some part embedded in the myometrium or may lie completely within the myometrium or may protrude into the peritoneal cavity while still being fixed in the myometrium [6]. Cases 2 and 3 had embedded IUDs. Embedded IUDs should be removed carefully as there are high chances of trauma. Hysteroscopic removal of IUD was possible in case 3, whereas, case 2 had to undergo laparotomy for the same. Embedded IUD can perforate through the uterine wall due to the contractions of uterus, resulting in complete perforation [5]. [Table/Fig-4] showing the cases published in literature on misplaced IUDs [6-11].
Published literature on misplaced IUDs [6-11].
| Year | Author | IUD complication | Method of IUD retrieval |
|---|
| 2016 | Dimitropoulos K et al., [6] | Migration of IUD to bladder | Cystoscopy |
| 2017 | Neumann DA et al., [7] | IUD embedded in omentum | Laparoscopy |
| 2018 | Cheung ML et al., [8] | IUD in posterior cul-de-sacIUD perforation into bladderIUD in adnexal region | LaparoscopyLaparotomy with repair of bladderPatient referred to higher centre |
| 2018 | Huh JM et al., [9] | IUD perforated the colon | Endoscopy |
| 2019 | Vahdat M et al., [10] | Migration of IUD to bladder | Cystoscopy |
| 2019 | Lei Y et al., [11] | Migration of IUD to rectum | Endoscopy |
| 2019 | Present case series | Migration of IUD to bladderIUD embedded in anterior wall of uterusIUD embedded in cervix | CystoscopyLaparotomyHysteroscopy |
Uterine perforation can be caused by immediate trauma or it can occur over time by gradual erosion through the myometrium [12]. Risk factors for uterine perforation include insertion by improper technique, lactation, postpartum insertion, low parity and history of abortions [13].
IUDs located in the peritoneal cavity lead to inflammation and formation of peritoneal adhesions. Therefore, the misplaced IUD needs to be removed, even if the patient is asymptomatic. This is best achieved laparoscopically if the IUD is located in the peritoneal cavity. In long-standing cases, the IUD gets surrounded by dense adhesions which make removal by minimally invasive techniques difficult. Laparotomy is required if minimally invasive techniques fail [14].
Conclusion
Perforation is an uncommon but serious complication of IUD insertion. Most cases are asymptomatic and usually diagnosed incidentally while investigating missing string. IUD removal in such cases can be challenging. Occasionally, IUD removal may not be possible using minimally invasive techniques, especially if the IUD is embedded. Gynaecologists must be aware of various types of perforations of uterus caused by IUD and their management strategies. Patients with IUD should come for regular follow-up visits and missing IUD should be removed promptly.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
PLAGIARISM CHECKING METHODS: [Jain H et al.]
Plagiarism X-checker: Jun 03, 2019
Manual Googling: Aug 05, 2019
iThenticate Software: Sep 09, 2019 (3%)
[1]. Mishra S, Tale of the tails, the missing postpartum IUCD StringsJ Obstet Gynaecol India 2017 67(3):202-07.10.1007/s13224-016-0940-928546668 [Google Scholar] [CrossRef] [PubMed]
[2]. Makins A, Taghinejadi N, Sethi M, Machiyama K, Munganyizi P, Odongo E, FIGO postpartum intrauterine device initiative: Complication rates across six countriesInt J Gynecol Obstet 2018 143(Suppl.1):20-27.10.1002/ijgo.1260030225873 [Google Scholar] [CrossRef] [PubMed]
[3]. Barnett C, Moehner S, Do Minh T, Heinemann K, Perforation risk and intra-uterine devices: results of the EURAS-IUD 5-year extension studyEur J Contracept Reprod Health Care 2017 22(6):424-28.10.1080/13625187.2017.141242729322856 [Google Scholar] [CrossRef] [PubMed]
[4]. Chauhan D, Gainder S, Comparison of clinical outcomes following CuT-380A insertion in postplacental period with interval insertionInt J Reprod Contracept Obstet Gynecol 2017 6(9):4111-15.10.18203/2320-1770.ijrcog20174071 [Google Scholar] [CrossRef]
[5]. Rowlands S, Oloto E, Horwell DH, Intrauterine devices and risk of uterine perforation: current perspectivesOpen Access J Contracept 2016 7:19-32.10.2147/OAJC.S8554629386934 [Google Scholar] [CrossRef] [PubMed]
[6]. Dimitropoulos K, Skriapas K, Karvounis G, Tzortzis V, Intrauterine device migration to the urinary bladder causing sexual dysfunction: a case reportHippokratia 2016 20(1):70-72. [Google Scholar]
[7]. Neumann DA, Graversen JA, Pugh SK, Intrauterine device embedded in omentum of postpartum patient with a markedly retroverted uterus: a case reportJ Med Case Rep 2017 11:29910.1186/s13256-017-1480-329065904 [Google Scholar] [CrossRef] [PubMed]
[8]. Cheung ML, Rezai S, Jackman JM, Patel ND, Bernnaba BZ, Hakimian O, Retained intrauterine device (IUD): Triple case report and review of the literatureCase Rep Obstet Gynecol 2018 2018:936296210.1155/2018/936296230627466 [Google Scholar] [CrossRef] [PubMed]
[9]. Huh JM, Kim KS, Cho YS, Suh DK, Lee JU, Baek SD, Colonoscopic removal of an intrauterine device that had perforated the rectosigmoid colonAnn Coloproctol 2018 34:10610.3393/ac.2017.10.3029742863 [Google Scholar] [CrossRef] [PubMed]
[10]. Vahdat M, Gorginzadeh M, Mousavi AS, Afshari E, Ghaed MA, Cystoscopic removal of a migrated intrauterine device to the bladder; a case reportContracept Reprod Med 2019 4:710.1186/s40834-019-0089-x31304041 [Google Scholar] [CrossRef] [PubMed]
[11]. Lei Y, Iablakov V, Karmali RJ, Forbes N, Endoscopic removal of migrated intrauterine deviceACG Case Rep J 2019 6(6):01-03.10.14309/crj.000000000000009031616765 [Google Scholar] [CrossRef] [PubMed]
[12]. Esposito JM, Zarou DM, Zarou GS, A Dalkon shield imbedded in a myoma: case report of an unusual displacement of an intrauterine deviceAm J Obstet Gynecol 1973 117:578-81.10.1016/0002-9378(73)90128-2 [Google Scholar] [CrossRef]
[13]. Kaislasuo J, Suhonen S, Gissler M, Lähteenmäki P, Heikinheimo O, Intrauterine contraception: incidence and factors associated with uterine perforation- a population-based studyHum Reprod 2012 27(9):2658-63.10.1093/humrep/des24622763376 [Google Scholar] [CrossRef] [PubMed]
[14]. Kho KA, Chamsy DJ, Perforated intraperitoneal intrauterine contraceptive devices: diagnosis, management, and clinical outcomesJ Minim Invasive Gynecol 2014 21(4):596-601.10.1016/j.jmig.2013.12.12324462588 [Google Scholar] [CrossRef] [PubMed]