Varied Presentation, Location and Outcomes in Management of Left Atrial Myxomas in a Tertiary Care Institution: A Case Series
Rupesh Kumar1, Alok Kumar2, Sanjib Rawat3
1 Assistant Professor, Department of Cardiothoracic and Vascular Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
2 Ex Senior Resident, Department of Cardiothoracic and Vascular Anesthesiology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
3 Senior Resident, Department of Cardiothoracic and Vascular Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rupesh Kumar, Assistant Professor, Room 4018, 4th Floor, Department of Cardiothoracic and Vascular Surgery, Advanced Cardiac Center, Postgraduate Institute of Medical Education and Research, Chandigarh-160012, India.
E-mail: rkctvs@gmail.com
Primary tumours of heart are a rare entity, and are mostly benign. Among them myxomas is the most common, typically Left Atrial (LA) arising from inter-atrial septum. Here we present a case series in which five patients were operated, of which four were female and one was male. The mean age was 57.4±16.1 years. Shortness of breath was the most common chief complaint followed by palpitation, altered sensorium. Majority of the patients belonged to NYHA II and III and ASA (American Society of Anaesthesiologists) 2 category. All were pedunculated masses. Of the masses three originated from interatrial septum, one from LA appendage, and another from the base of anterior mitral leaflet (aorto-mitral mitral junction). Transseptal approach, via right atrium was used in most cases. The mean cross clamp time was 50.6 minutes and cardiopulmonary bypass time was 80.2 minutes. The mean Vasoactive-Inotropic Score (VIS) was 8.6, and mean intensive care unit stay was 3.6 days. Besides a patient requiring tracheostomy, there were no other complications. They are easily diagnosed with echocardiography and once operated they have an excellent recovery, and remain symptom free.
Benign tumour of heart, Cardiac tumours, Embolization
Introduction
Primary tumours of heart are a rare entity, and are mostly benign. Among them myxomas is the most common, typically Left Atrial (LA) arising from inter-atrial septum. They present with symptoms similar to mitral stenosis and is readily diagnosed with the help of transthoracic echocardiography [1].
Case 1
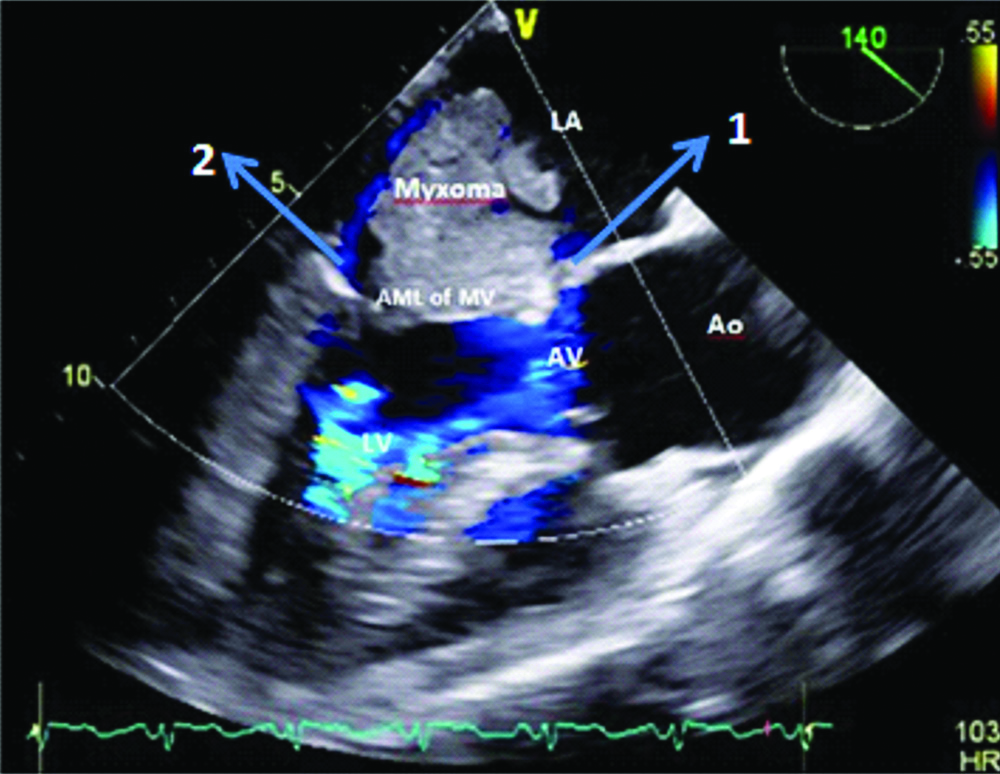
A 57-year-old diabetic female weighing 52 kg {Body Surface Area (BSA) 1.5} presented with complaints of shortness of breath (NYHA IV). On evaluation she found to have LA myxoma (attached to interatrial septum) with severe mitral valvular regurgitation {Vena Contracta (VC) of 6 mm with systolic reversal in pulmonary vein) [Table/Fig-1]. She also had severe tricuspid regurgitation (VC of 7 mm with systolic reversal in hepatic vein) and moderate Pulmonary Arterial Hypertension (PAH) {Right Ventricular Systolic Pressure (RVSP)=55+Right Atrial Pressure (RAP) in mm of Hg} underwent myxoma removal and mechanical mitral valve bileaflet prosthesis under normothermic Cardiopulmonary Bypass (CPB). The clamp time was 90 minutes and CPB time was 134 minutes. Patient was shifted to Intensive Care Unit (ICU) in stable condition with VIS score of 18. This patient got reintubated due to altered sensorium and hypernatremia and landed in tracheostomy for long term respiratory care.
Transoesophageal echocardiography, Mid oesophageal four chamber view demonstrating LA myxoma arising from interatrial septum: 1) and mitral regurgitation jet in color doppler; 2) LA: left atrium; LV: Left ventricle; RA: Right atrium RV: Right ventricle; MR: Mitral regurgitation.
Case 2
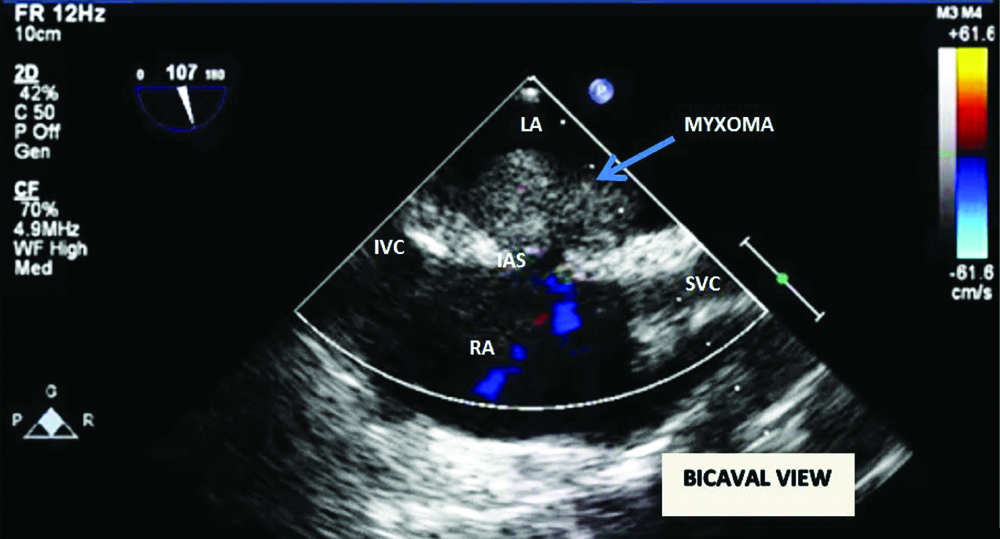
A 30-year-old female weighing 46 kg (BSA 1.3) presented with complaints of shortness of breath (NYHA III). On evaluation she was found to have LA myxoma (attached to interatrial septum) [Table/Fig-2]. She underwent myxoma removal under normothermic CPB. The clamp time was 25 minutes and CPB time of 41 minutes. Patient got shifted to ICU in stable condition with VIS score of 5. Recovery was uneventful with discharge from ICU after 3 days.
Transoesophageal echocardiography, Mid oesophageal bicaval view demonstrating LA myxoma arising from Interatrial septum (IAS).
LA: Left atrium; RA: Right atrium; SVCP: Superior venacava; IVC: Inferior vanacava
Case 3
A 68-year-old female weighing 60 kg (BSA 1.65) presented with complaints of shortness of breath (NYHA II) along with pain in the right hypochondrium. On evaluation she was found to have LA myxoma attached to interatrial septum with acute calculous cholecystitis underwent atrial myxoma removal under normothermic CPB and cholecystectomy. The aortic cross clamp time was 43 minutes and CPB time was 63 minutes. Patient was shifted to ICU in stable condition without any inotropes. Recovery was uneventful with discharge from ICU after 3 days.
Case 4
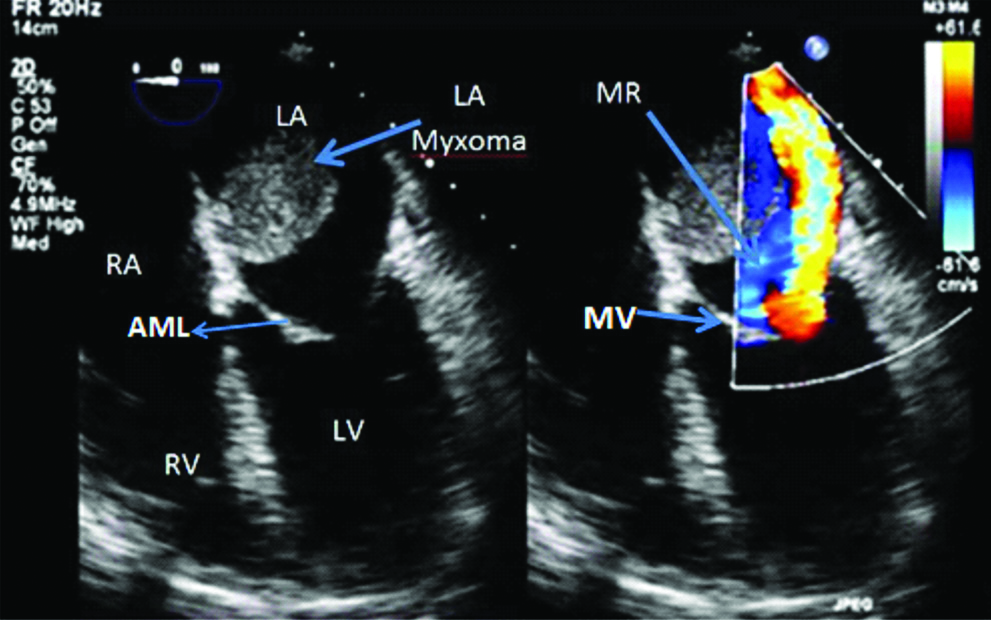
A 70-year-old male weighing 50 kg (BSA 1.4) presented with symptoms of altered sensorium and right upper and lower limb weakness along with shortness of breath (NYHA III). On evaluation he was found to have LA myxoma attached to the aorto-mitral junction on echocardiography [Table/Fig-3]. A contrast enhanced computer tomography of brain revealed infarct in the right middle cerebral artery territory. He underwent myxoma removal under normothermic CPB. The aortic cross clamp time was 50 minutes and cardiopulmonary bypass time was 85 minutes. Patient shifted to ICU in stable condition with VIS score of 12. Recovery was uneventful with discharge from ICU after 3 days.
Transoesophageal echocardiography, Mid oesophageal long axis view demonstrating LA myxoma arising from aortomitral junction.
LA: Left atrium; LV: Left ventricle; Ao: Aorta; AV: Aortic valve; AML: Anterior mitral leaflet; MV: Mitral valve
Case 5
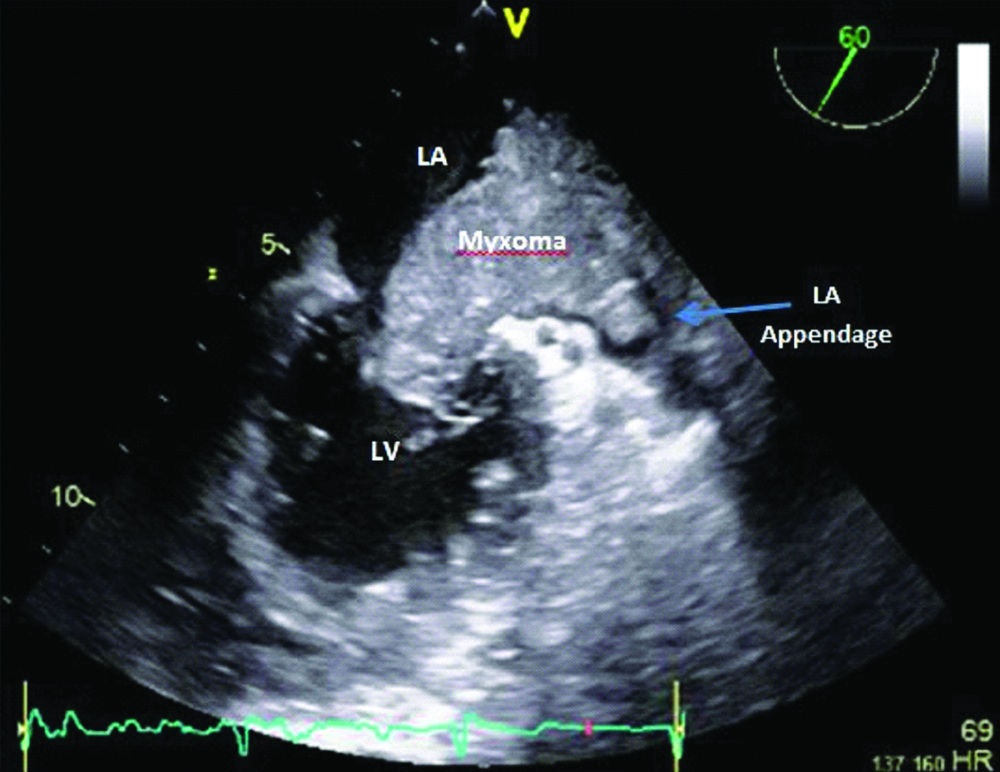
A 62-year-old hypertensive female weighing 48 kg (BSA 1.4) presented with complaints of shortness of breath (NYHA II). On evaluation she was found to have LA myxoma attached to the LA appendage [Table/Fig-4]. She underwent LA myxoma removal under normothermic CPB. The aortic cross clamp time was 45 minutes and CPB time was 78 minutes. Patient was shifted to ICU in stable condition with VIS score of 8. Recovery was uneventful with discharge from ICU after 3 days.
Transoesophageal echocardiography, Mid oesophageal comissural view demonstrating LA myxoma arising from LA appendage.
LA: Left atrium; LV: Left ventricle
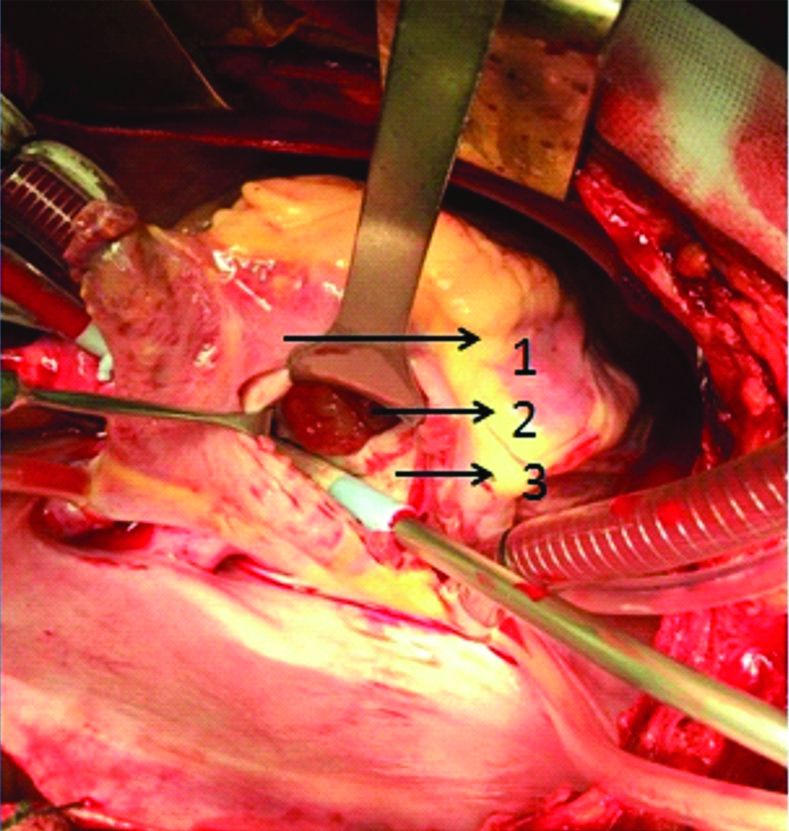
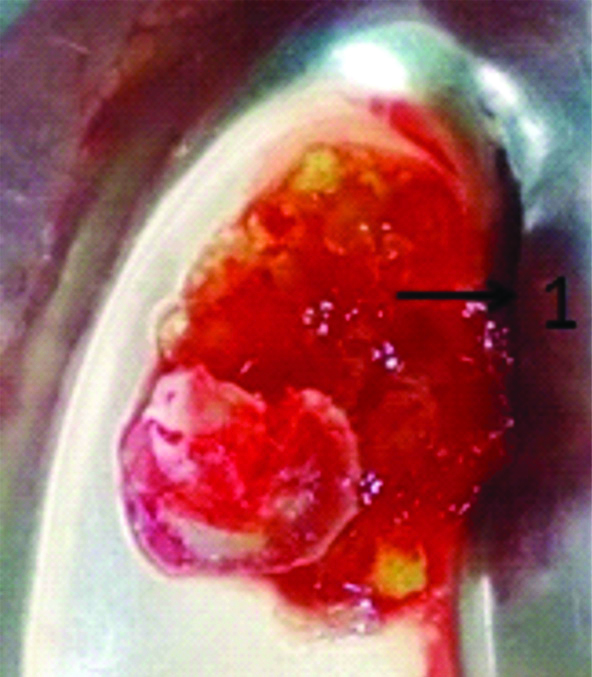
Tumours can be approached through right atrium (trans-septal) [Table/Fig-5]. Origin from interatrial septum is most common, but other sites are also routinely found. Complete excision of the tumour with 3 to 5 mm rim is to be done, with reconstruction of the defect. The specimen should be retrieved from the cardiac chambers en-mass with caution as it can break easily into fragments [Table/Fig-6]. These patients require minimal inotropic support and have a good postoperative recovery. Here we discuss our series of cases operated for LA myxoma [Table/Fig-7].
Intraoperative picture demonstrating trans-septal approach of left artrial myxoma removal under cardiopulmonary bypass. 1) right atrium, 2) left atrial myxoma, 3) interatrial septum.
Specimen of left atrial myxoma (1=left atrial myxoma).
Preoperative, intraoperative and postoperative features of patients undergoing operation for left atrial myxoma.
| Name | Age | Sex | Weight | Height | BSA | NYHA | AXC (mins) | CPB (mins) | MV duration | ICU stay | Euro score | VIS score |
|---|
| Case 1 | 57 | F | 52 | 158 | 1.5 | 4 | 90 | 134 | 61 | 6 | 8/11.85% | 18 |
| Case 2 | 30 | F | 46 | 159 | 1.3 | 3 | 25 | 41 | 0 | 3 | 3/5.96% | 5 |
| Case 3 | 68 | F | 60 | 164 | 1.65 | 2 | 43 | 63 | 2 | 3 | 3/3.07% | 0 |
| Case 4 | 70 | M | 50 | 170 | 1.4 | 3 | 50 | 85 | 10 | 3 | 2/3.51% | 12 |
| Case 5 | 62 | F | 48 | 148 | 1.4 | 2 | 45 | 78 | 19.5 | 3 | 4/3.24% | 8 |
| Mean±SD | 57.4±16.1 | F-80%, M-20% | 51.2±5.4 | 159.8±8.1 | 1.45±0.13 | | 50.6 ±23.9 | 80.2±34.4 | 18.5±24.9 | 3.6±1.34 | | 8.6±6.84 |
NYHA: New York heart association; BSA: Body surface area in Kg/m2; AXC: Aortic cross clamp time in minutes; CPB: Cardiopulmonary bypass time in minutes; MV duration: Mechanical ventilation time in hours; ICU: Intensive care unit; VIS: Vasoactive inotropic score
Discussion
Myxoma is the most common primary intracardiac tumour, which has an incidence of 0.02% in the general population [1]. It is more common in the LA and mainly originates from an area in the atrial septum near the fossa ovalis [2]. Right Atrial (RA) myxomas are less common. Less commonly, it could be found in the aorta, pulmonary artery, ventricles, vena cava, or even other organs [3]. In our series, three originated from interatrial septum, one from LA appendage, and one from the base of anterior mitral leaflet (aorto-mitral junction).
The current concept of origin of myxomas is believed to be from multipotent mesenchymal cells present in entrapped embryonic foregut. The early stages of growth is attributed to the angiogenesis by Vascular Endothelial Growth Factor (VEGF) produced by the tumour [4].
Majority of the cardiac myxomas (over 90%) occur sporadically and such sporadic tumours are seen chiefly in women between the third and sixth decades of life [5]. The pathogenesis of sporadic myxoma is poorly understood, but a mutation in protein kinase A type I-A in chromosome 17 can lead to Carney’s complex, a familial cardiac myxoma [6]. Carney syndrome accounts for the majority of familial cases with an incidence of 7%. It is an autosomal dominant syndrome characterised by cardiac and extra-cardiac myxomas, spotty skin pigmentation, endocrine hyperactivity, and other tumours (such as testicular sertoli cell tumours, pituitary adenoma and thyroid tumours) [7].
Cardiac myxomas have varied clinical presentation. Typically, patients are asymptomatic or present with nonspecific signs and symptoms [8]. In our series four had cardiac symptoms and one had embolic symptoms. The commonly occurring clinical presentations are: cardiac (67%), embolic (29%), and systemic (34%) symptoms.
Commonly observed symptoms are dyspnea, orthopnea, paroxysmal nocturnal dyspnea, cough, haemoptysis, oedema and fatigue [9]. Embolization of systemic or pulmonary circulation is common. Most embolic events are related to cardiac myxomas involve the cerebral arteries [10], but emboli also may involve renal, coronary, or lower limb arteries [11]. Constitutional symptoms (e.g., fever, weight loss, rash, malaise, nausea, vomiting) are seen in around 30% patients [12]. Augmented release of interleukin 6 from myxoma cells causes systemic symptoms. On investigation, findings as anaemia, elevated Erythrocyte Sedimentation Rate (ESR), C-reactive protein, or globulin level are seen [13].
The typical imaging modalities used for diagnostic purposes include echocardiography, CT scan and cardiac MRI [14]. Diagnosis with two-dimensional echocardiography is usually adequate with good sensitivity detecting 95% of myxomas, however transoesophageal echocardiography has a sensitivity approaching 100% [15]. Echocardiography easily defines the location, shape, size, and relations of mass with intracardiac components.
CT scan and cardiac MRI can also be used as an alternate modalities. Myxomas appear as spherical/ovoid shaped intra-cavitary masses with heterogeneous composition [16]. Both cardiac MRI and CT produces high resolution images but still MRI is preferred because T1 and T2 weighted sequences helps in determining the chemical microenvironment present within the tumour and helps in diagnosing exact nature of the tumour [17].
Once a presumptive diagnosis of myxoma has been made on imaging studies, surgical resection is the treatment of choice. The surgical approach for atrial myxomas should be the following: (1) to allow minimal manipulation of the tumour; (2) to provide adequate exposure for complete resection of the tumour; (3) to allow inspection of all four heart chambers; (4) to minimise recurrence [10]. Damaged valves may require annuloplasty or prosthetic replacement in case of destruction of the annulus or valve leaflets. Recurrence occurs in around 3% of the tumours, and the risk of recurrence is higher in younger patients, in familial forms of myxoma, and in multilocular myxomas [18,19].
Conclusion
Myxomas are the most frequent cardiac tumours and it may be totally asymptomatic or symptomatic. The two most common symptoms are Chronic heart failure and systemic embolization, however it is precisely related to the type of tumour and its location. Surgery is the treatment of choice with extremely good rate of survival and need for re-operation is less but still yearly follow-up with echocardiography is mandatory as cases with familial history has tendency to recur.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 05, 2019
Manual Googling: Aug 22, 2019
iThenticate Software: Sep 06, 2019 (15%)
[1]. Vale MDP, Sobrinho AF, Sales MV, Teixeira MM, Cabral KC, Giant myxoma in the left atrium: Case reportBrazilian Journal of Cardiovascular Surgery 2008 23(2):276-78.10.1590/S0102-7638200800020002018820794 [Google Scholar] [CrossRef] [PubMed]
[2]. Diaz A, di Salvo C, Lawrence D, Hayward M, Left atrial and right ventricular myxoma: An uncommon presentation of a rare tumourInteractive Cardiovascular and Thoracic Surgery 2011 12(4):622-23.10.1510/icvts.2010.25566121273256 [Google Scholar] [CrossRef] [PubMed]
[3]. Croti UA, Braile DM, Souza AS, Cury PM, Right ventricle and tricuspid valve myxomaBrazilian Journal of Cardiovascular Surgery 2008 23(1):142-44.10.1590/S0102-7638200800010002618719845 [Google Scholar] [CrossRef] [PubMed]
[4]. Amano J, Kono T, Wada Y, Zhang T, Koide N, Fujimori M, Ito K, Cardiac myxoma: Its origin and tumor characteristicsAnn Thorac Cardiovasc Surg 2003 9(4):215-21. [Google Scholar]
[5]. Yoon DH, Roberts W, Sex distribution in cardiac myxomasAm J Cardiol 2002 90(5):563-65.10.1016/S0002-9149(02)02540-7 [Google Scholar] [CrossRef]
[6]. Yin Z, Kirschner LS, The Carney complex gene PRKAR1A plays an essential role in cardiac development and myxomagenesisTrends Cardiovasc Med 2009 19:44-49.10.1016/j.tcm.2009.04.00519577711 [Google Scholar] [CrossRef] [PubMed]
[7]. Wilkes D, Charitakis K, Basson CT, Inherited disposition to cardiac myxoma developmentNat Rev Cancer 2006 6:157-65.10.1038/nrc179816491075 [Google Scholar] [CrossRef] [PubMed]
[8]. Rodriguez-Cruz E, Rao PS, (2016) Pediatric Cardiac Tumors, Clinical PresentationMedscape Reference 4 January 2016 [Google Scholar]
[9]. Kolluru A, Desai D, Cohen GI, The etiology of atrial myxoma tumor plopJ Am Coll Cardiol 2011 57(21):e37110.1016/j.jacc.2010.09.08521596227 [Google Scholar] [CrossRef] [PubMed]
[10]. Vaideeswar P, Gupta R, Mishra P, Lanjewar C, Raut A, Atypical cardiac myxomas: A clinicopathologic analysis and their comparison to 64 typical myxomasCardiovasc Pathol 2012 21:180-87.10.1016/j.carpath.2011.07.00121839650 [Google Scholar] [CrossRef] [PubMed]
[11]. Yadav S, Alvarez JM, Catastrophic presentation of atrial myxoma with total occlusion of abdominal aortaInteract Cardiovasc Thorac Surg 2009 9:913-15.10.1510/icvts.2009.21251419696050 [Google Scholar] [CrossRef] [PubMed]
[12]. Watts G, Sadashivan D, Gopalan V, Sharma S, Left atrial myxoma presenting with acute pancreatitisThe Internet Journal of Thoracic and Cardiovascular Surgery 2007 8(2)10.5580/274a [Google Scholar] [CrossRef]
[13]. Aggarwal SK, Barik R, Sarma TC, Iyer VR, Sai V, Mishra J, Clinical presentation and investigation findings in cardiac myxomas: New insights from the developing worldAm Heart J 2007 154(6):1102-07.10.1016/j.ahj.2007.07.03218035082 [Google Scholar] [CrossRef] [PubMed]
[14]. Yadav S, Alvarez JM, Catastrophic presentation of atrial myxoma with total occlusion of abdominal aortaInteract Cardiovasc Thorac Surg 2009 9:913-15.10.1510/icvts.2009.21251419696050 [Google Scholar] [CrossRef] [PubMed]
[15]. Kaya H, Gökdeniz T, Tuncer A, Ozkan M, Left atrial myxoma demonstrated by real-time three-dimensional transoesophageal echocardiographyTurkish Cardiology Association Archives 2010 38(3):222 [Google Scholar]
[16]. Araoz PA, Mulvagh SL, Tazelaar HD, Julsrud PR, Breen JF, CT and MR imaging of benign primary cardiac neoplasms with echocardiographic correlationRadiographics 2000 20:1303-19.10.1148/radiographics.20.5.g00se12130310992020 [Google Scholar] [CrossRef] [PubMed]
[17]. Rahmanian PB, Castillo JG, Sanz J, Adams DH, Filsoufi F, Cardiac myxoma: Preoperative diagnosis using a multimodal imaging approach and surgical outcome in a large contemporary seriesInteract Cardiovasc Thorac Surg 2007 6(4):479-83.10.1510/icvts.2007.15409617669910 [Google Scholar] [CrossRef] [PubMed]
[18]. Perek B, Misterski M, Stefaniak S, Ligowski M, Puślecki M, Jemielity M, Early and long-term outcome of surgery for cardiac myxoma: Experience of a single cardiac surgical centreCardiology Poland 2011 69(6):558-64. [Google Scholar]
[19]. Mendoza C, Bernstein E, Ferreira A, Multiple recurrences of nonfamilial cardiac myxomas: A report of two casesTex Heart Inst J 2007 34(2):236-39. [Google Scholar]