A Case of Parotid Gland Lymphoma: A Rare Entity
Manika Khare1, Zai Wade2, Sunil Garg3
1 Consultant, Department of Pathology, Apex Hospitals, Jaipur, Rajasthan, India.
2 Consultant, Department of Pathology, Apex Hospitals, Jaipur, Rajasthan, India.
3 Consultant, Department of Ear, Nose and Throat, Apex Hospitals, Jaipur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manika Khare, 3/293, Malviya Nagar, Jaipur, Rajasthan, India.
E-mail: drmanika09@gmail.com
Dear Editor,
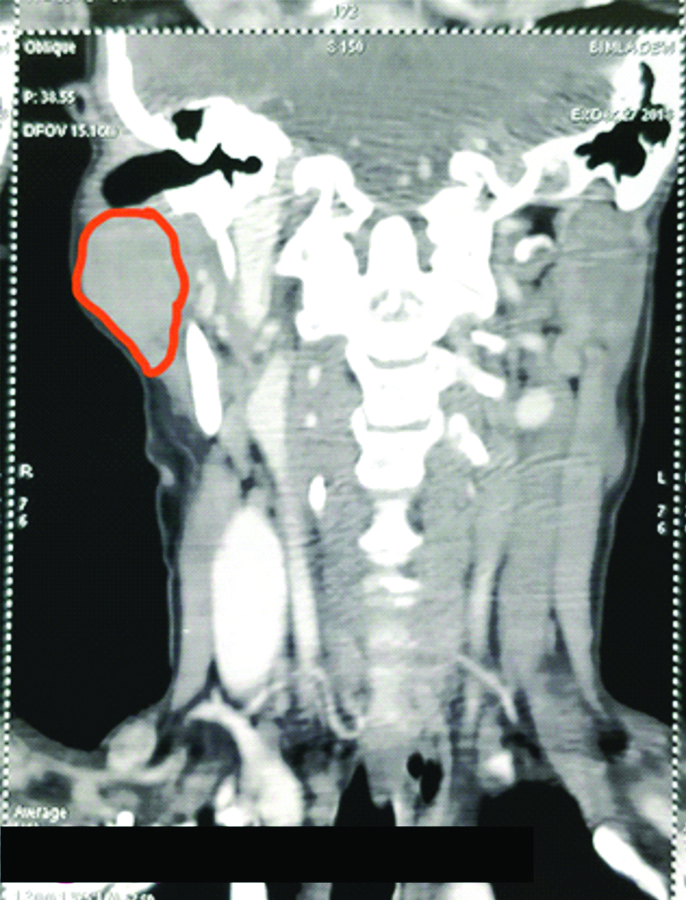
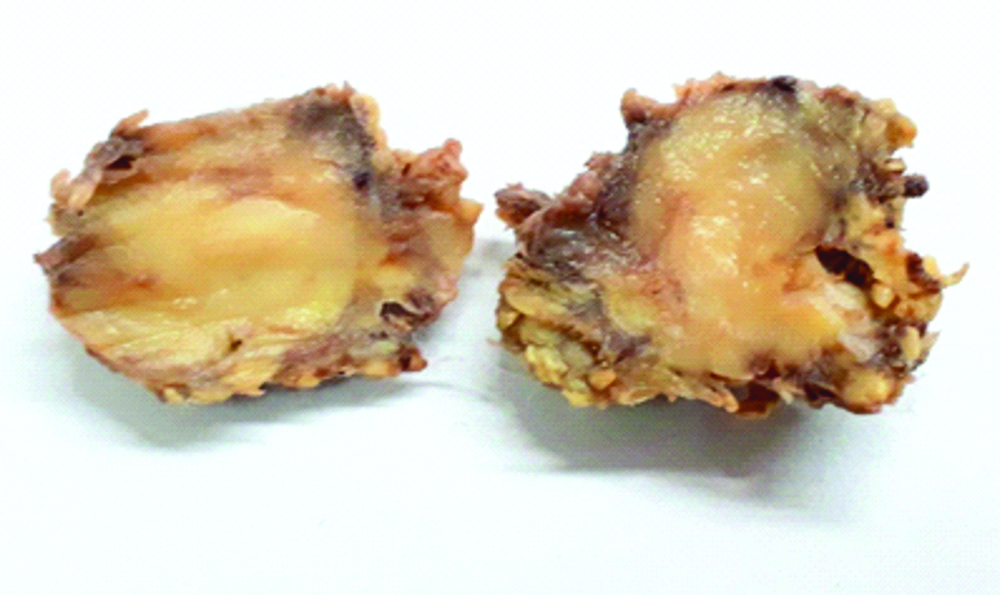
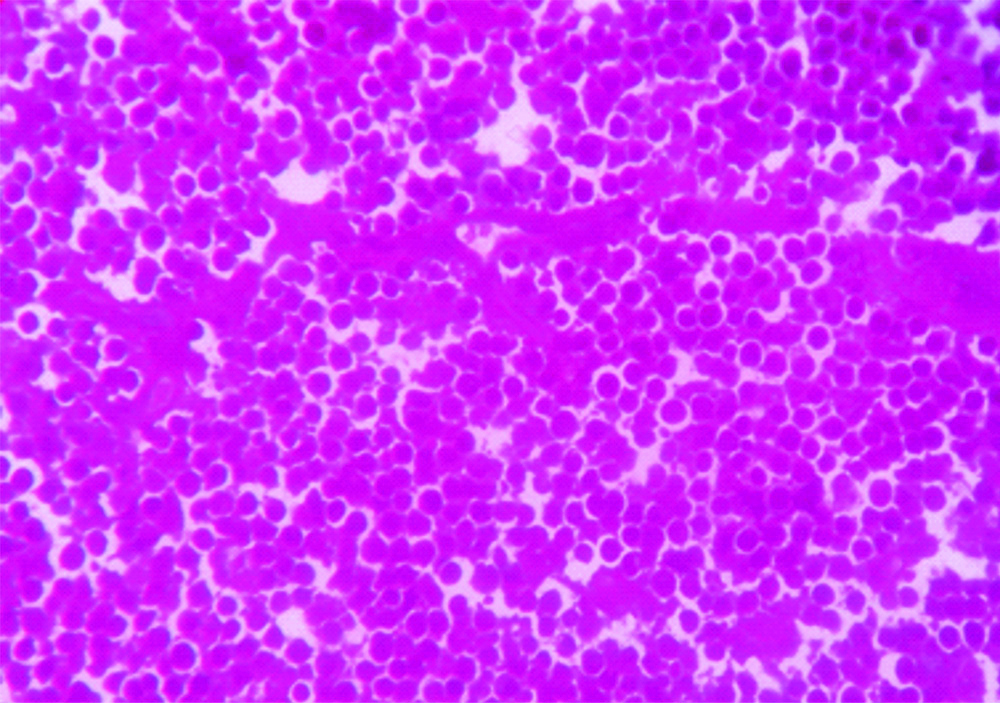
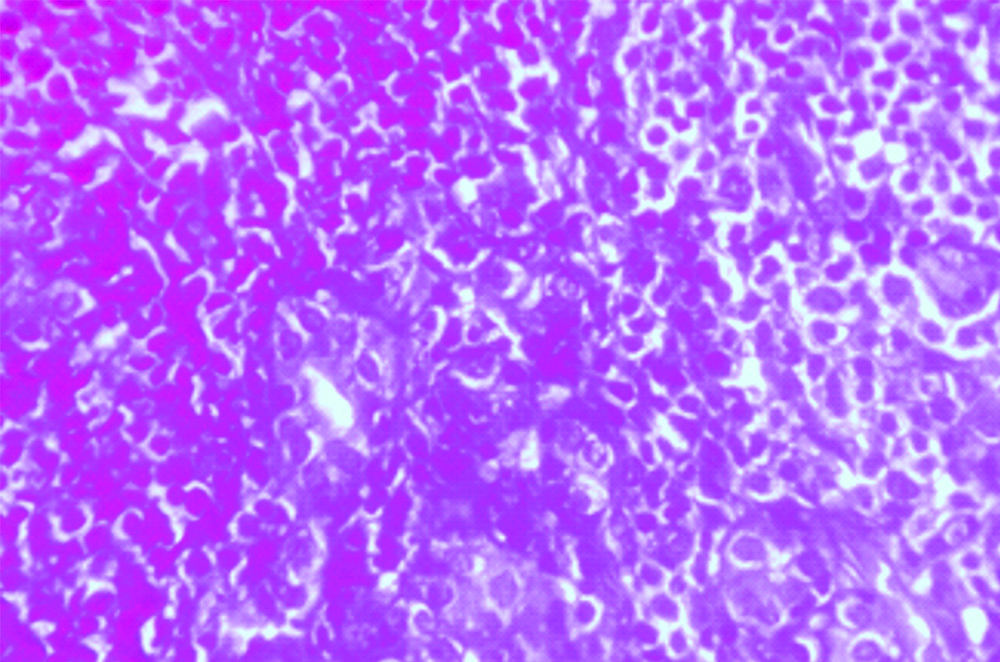
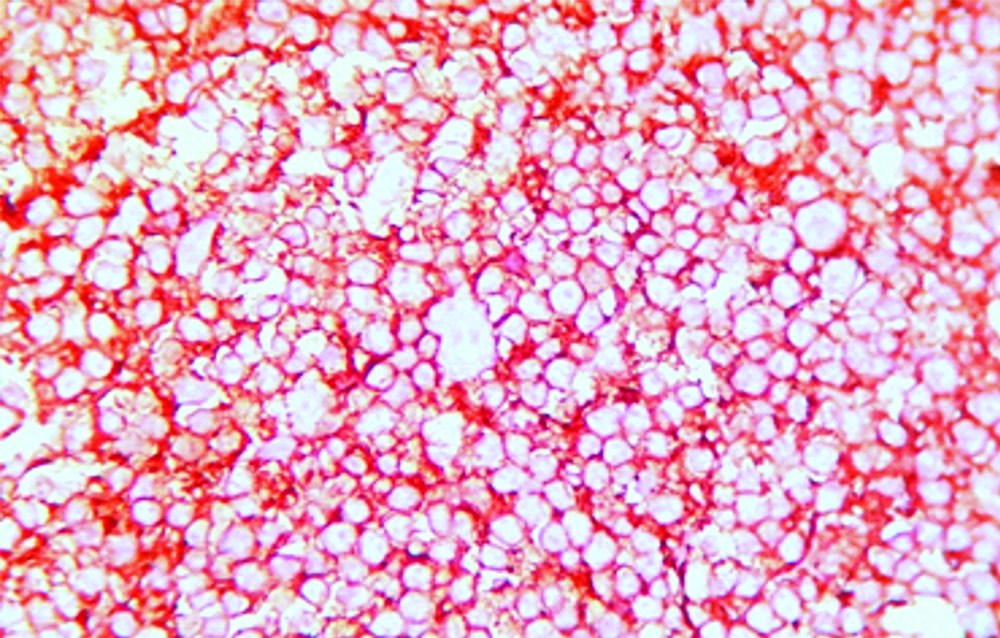
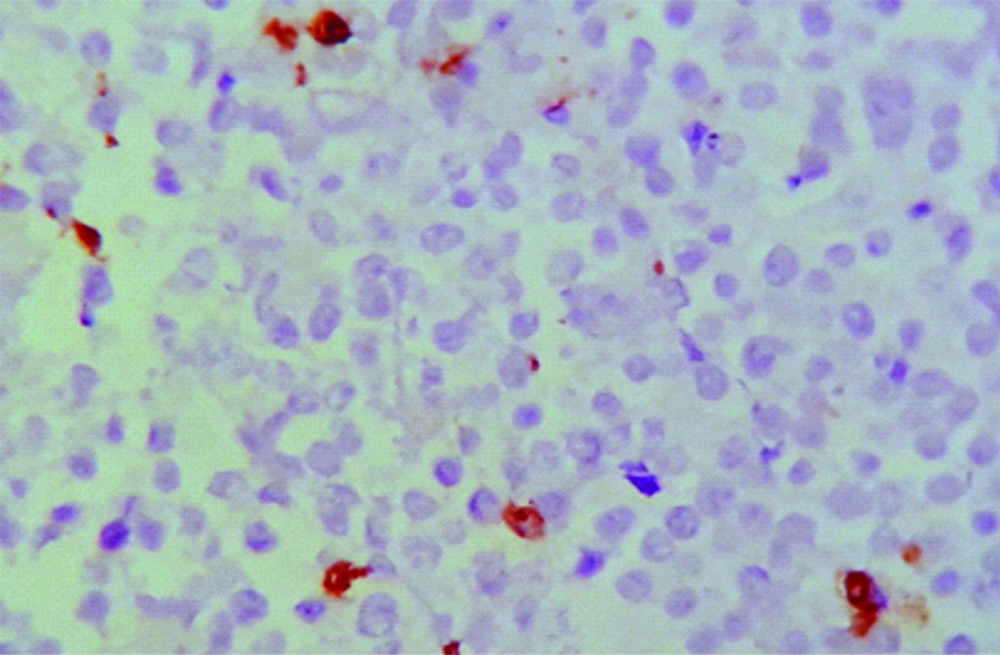
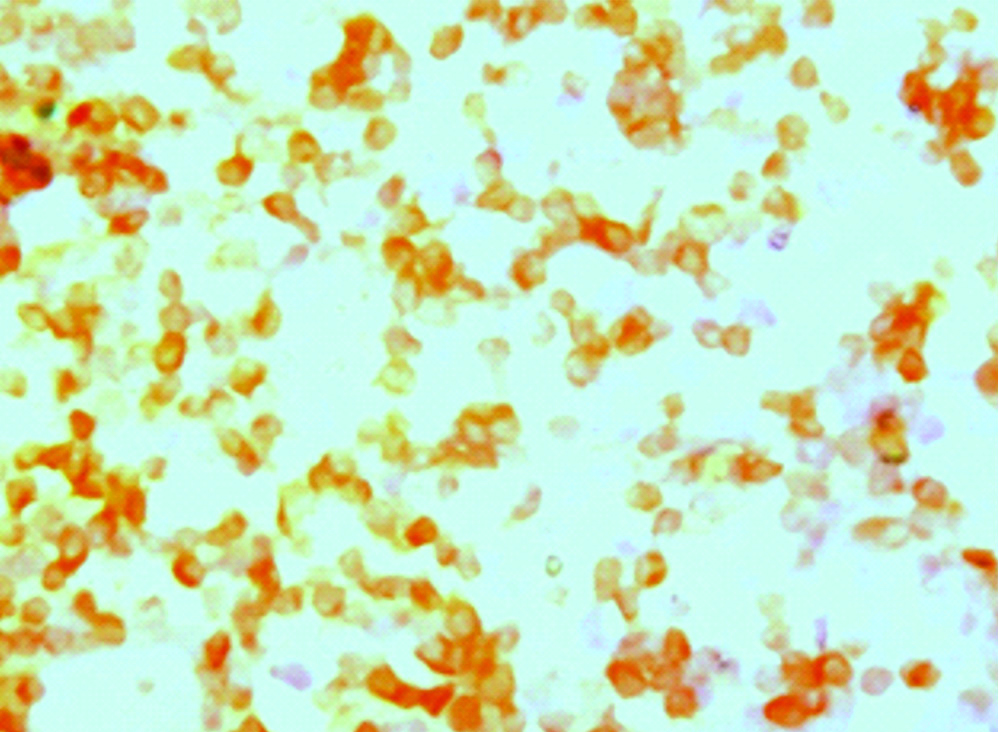
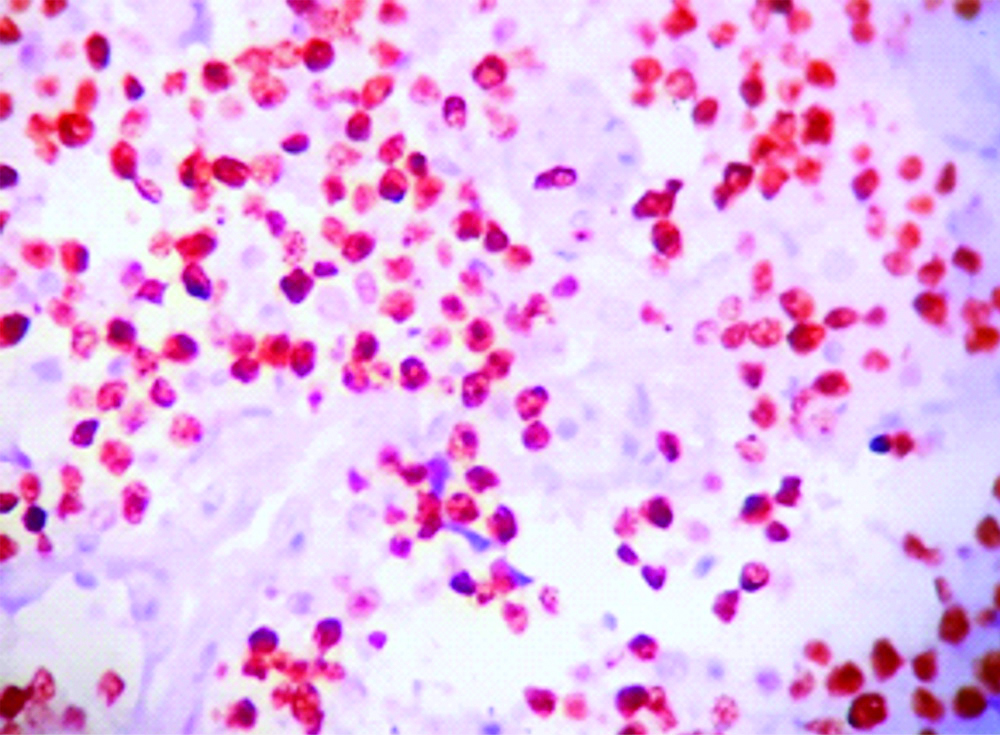
Lymphoma is the second most common neoplasm of the head and neck region after squamous cell carcinoma [1]. In the parotid tumours the prevalence of the lymphoma is very rare, accounting to just 1-4% of cases [2], due to which clinician do not consider lymphoma as one of the differential when he is evaluating a parotid mass. In the present case a 55-year-old female presented to the ENT OPD with a complaint of gradually increasing swelling in the right parotid region since three months which was not associated with any pain. On clinical examination a diffuse swelling was present in the right parotid region measuring approximately 2.5×2.5 cm, with overlying unremarkable skin. On palpation swelling was soft to firm in consistency, well circumscribed. No other significant past medical or hereditary history was there. Based on clinical findings, possibility of pleomorphic adenoma was kept. Computed tomography of the patient showed a well circumscribed contrast enhancing mass in right parotid gland measuring 3×3 cm [Table/Fig-1]. Based on above findings possibility of benign parotid gland neoplasm was given. Patient consent was taken and was operated. Lazy S incision was given, surrounding soft tissue was dissected, dissection of the facial nerve was done and superficial parotidectomy was done. Grossly, single well circumscribed grey brown soft tissue mass was received measuring 2.5×2×0.5 cm. Cut section of the specimen was grey white with slightly infiltrating margins [Table/Fig-2]. Represented sections from the tumour were submitted for the histopathological examination. On microscopic examination, it showed a tumour composed of atypical lymphoid cells arranged in sheets, invading adjacent adipose tissue and salivary glands [Table/Fig-3,4]. Based on microscopic findings, diagnosis of Non Hodgkin lymphoma (large cell type) was given. Immunohistochemistry was done for further confirmation of the diagnosis and further categorisation of the lymphoma. On immunohistochemistry tumour cells were diffusely positive for CD20 and negative for CD3 [Table/Fig-5,6]. Tumour cells showed positivity for CD10 and BCl6 and negative for MUM1. Cells showed focal positivity for BCl2 and showed c-myc positivity in approximately 80% of cells [Table/Fig-7,8,9 and 10]. Ki67 was positive in more than 90% of cells [Table/Fig-11]. Based on above findings diagnosis of Diffuse Large B Cell Lymphoma (DLBCL), germinal center type with double hit was given, which express both BCL-2 and c-myc and are associated with poor prognosis. PET Scan of the patient was done thereafter to look for involvement of other lymph nodes. This case was stage I as only single lesion was identified on PET scan. Except post surgery changes no other evidence of any lesion was appreciated. After that we lost follow-up of the patient.
CT image showing well defined mass in the right parotid region.
Gross specimen, cut section showing grey white mass with infiltrative margins.
Microphotograph showing lymphoid cells present in sheets, cells are monomorphic in appearance (H&E,40X).
Photomicrograph showing atypical lymphoid cells infiltrating in adjacent parotid gland (H&E,40X).
IHC slide showing diffuse CD20 positivity in tumour cells.
IHC slide showing tumour cells are negative for CD3.
IHC slide showing tumour cells positive for BCL6.
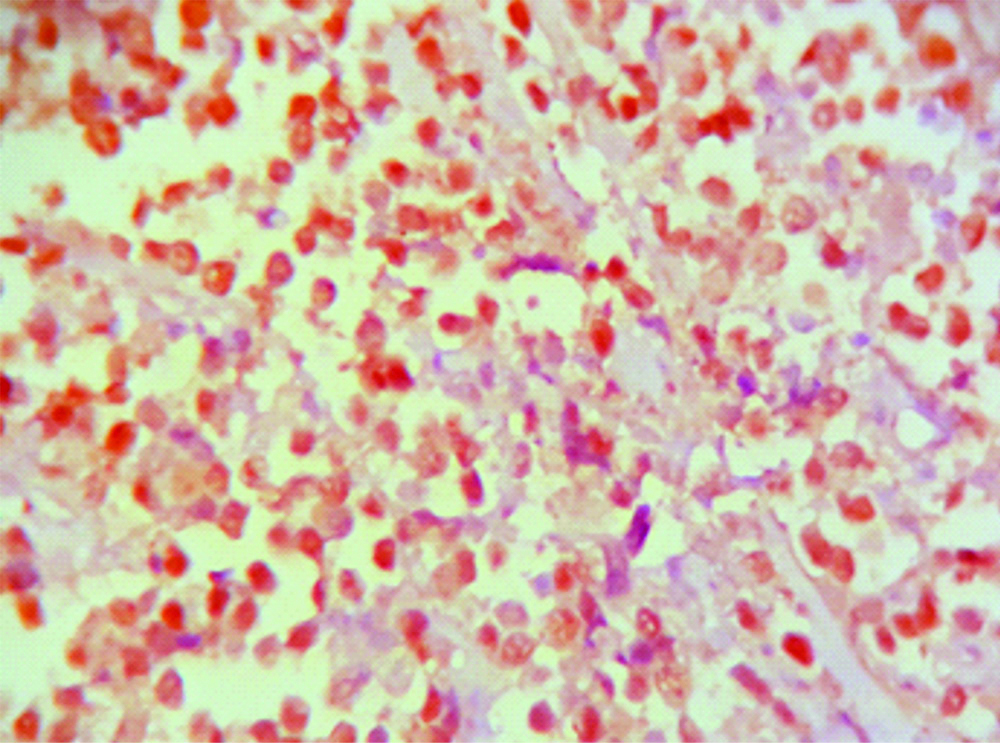
IHC slide showing tumour cells positive for CD10.
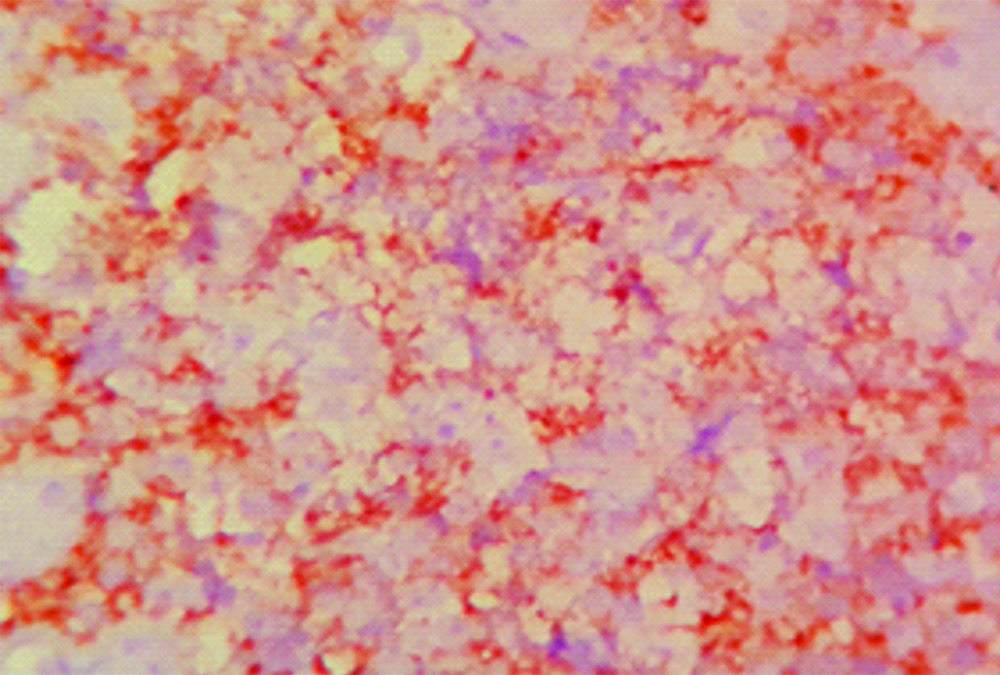
IHC slide showing focal BCL2 positivity.
IHC slide showing tumour cells positive for c-myc.
IHC slide showing Ki67 approx 90%.
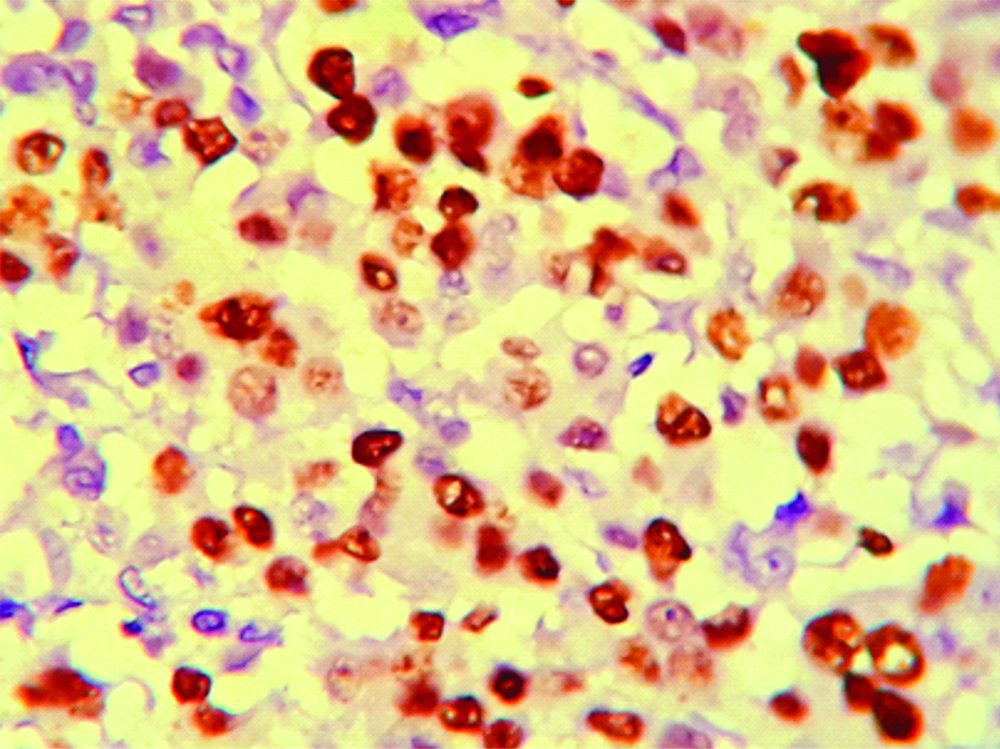
Malignant lymphomas of the parotid are usually seen in the adult groups i.e., more than 50 years with peak age at 55 years [3]. The lymphomas may arise within the gland or from intraparotid lymph nodes. If only the lymph nodes are involved without parenchyma infiltration then it should be considered of nodal origin [4]. The DLBCL is a high grade lymphoma associated with destruction of salivary gland parenchyma with tumour cells invading between residual parotid gland parenchyma. This case was primary parotid gland lymphoma as it was distructing surrounding tissue. Most NHLs arising in the salivary glands are B cell lineage including low grade B cell lymphoma of Mucosa Associated Lymphoid Tissue (MALT), follicular lymphoma and DLBCL [5]. Initial evaluation for parotid tumours should include Magnetic Resonance Imaging (MRI) or CT to determine tumour size, shape, and location. The final diagnosis of DLBCL is made with the help of histopathological examination and immunohistochemistry. These tumours are strongly positive for B cell marker that is CD20. These tumours are subdivided into germinal and non germinal centre type based on CD10, MUM1 and BCL6. For further categorisation into Double-Hit Lymphomas (DHLs) c-myc is applied and its expression is noted. Once the diagnosis of NHL is formed it is important to evaluate the patient for the other systemic involvements, to further decide for the therapy of the patient. The Ann Arbor or International Prognostic Index (IPI) scoring system is used to stage the disease [6]. This case was stage I as only single lesion was identified on PET scan. Aggressive lymphomas like DLBCL are assumed to have poor prognosis due to dissemination of the disease even though if there is no evidence of multiple lesions of radiological screening, due to which these cases are treated with chemotherapy and rituximab-CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) and radiotherapy both. Localised low-grade lymphoma is treated with radiotherapy. DHLs are a subtype of DLBCL with concurrent chromosomal rearrangements involving the MYC and BCL2 and/or BCL6 genes, accounting approximately 2-10% of newly diagnosed DLBCL [7]. These lymphomas are associated with poor prognosis with R-CHOP treatment. Total of 6-8 cycles are given to patient, followed by the radiotherapy if the disease is residual or extranodal site have bulky disease.
Primary parotid gland lymphomas are very rare. Histopathology is the gold standard for the diagnosis of the parotid gland lymphoma. Immunohistochemistry plays a key role in confirming the diagnosis and to further categorise it. DHLs are associated with poor prognosis so early diagnosis and treatment plays an important role for the patient.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
PLAGIARISM CHECKING METHODS: [Jain H et al.]
Plagiarism X-checker: Jun 01, 2019
Manual Googling: Aug 23, 2019
iThenticate Software: Sep 06, 2019 (11%)
[1]. Nassie DI, Berkowitz M, Wolf M, Kronenberg J, Talmi YP, Parotid mass as presenting symptom of lymphomaIsr Med Assoc J 2010 12:416-18. [Google Scholar]
[2]. Dispenza F, Cicero G, Mortellaro G, Marchese D, Kulamarva G, Dispenza C, Primary non-Hodgkins lymphoma of the parotid glandBraz J Otorhinolaryngol 2011 77:639-44.10.1590/S1808-8694201100050001722030974 [Google Scholar] [CrossRef] [PubMed]
[3]. Loggins JP, Urquhart A, Preoperative distinction of parotid lymphomasJ Am Coll Surg 2004 199:58-61.10.1016/j.jamcollsurg.2004.03.00415217631 [Google Scholar] [CrossRef] [PubMed]
[4]. Barnes L, Eveson JW, Reichart P, Sidransky D, Tumours of the salivary glandsWorld Health Organisation-Classification of Tumours, Pathologyand Genetics of Head and NeckTumours 2005 5LyonIARC Press:209-81. [Google Scholar]
[5]. Borovecki A, Korac P, Ventura RA, Perisa MM, Banham AH, Dominis M, MALT1, BCL10 and FOXP1 in salivary gland mucosa-associated lymphoid tissue lymphomasPatholInt 2007 57(1):47-51.10.1111/j.1440-1827.2007.02056.x17199743 [Google Scholar] [CrossRef] [PubMed]
[6]. Lister TA, Crowther D, Sutcliffe SB, Glatstein E, Canellos GP, Young RC, (November 1989). Report of a committee convened to discuss the evaluation and staging of patients with Hodgkin’s disease: Cotswolds meetingJ Clin Oncol 1989 7:1630-36.10.1200/JCO.1989.7.11.16302809679 [Google Scholar] [CrossRef] [PubMed]
[7]. Pedersen MO, Gang AO, Poulsen TS, Knudsen H, Lauritzen AF, Nielsen SL, MYC translocation partner gene determines survival of patients with large B-cell lymphoma with MYC- or double-hit MYC/BCL2 translocationsEur J Haematol 2014 92:42-48.10.1111/ejh.1221224118498 [Google Scholar] [CrossRef] [PubMed]