Cystadenofibroma of Ovary- A Rare Cause of Postmenopausal Bleeding
Tanuja Muthyala1, Sujata Siwatch2, Shalini Gainder3, Minakshi Rohilla4, Vanita Jain5, Parikshaa Gupta6
1 Ex-Senior Resident, Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, India.
3 Additional Professor, Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, India.
4 Professor, Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, India.
5 Professor, Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, India.
6 Assistant Professor, Department of Cytology and Gynaecological Pathology, PGIMER, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sujata Siwatch, Department of Obstetrics and Gynaecology, PGIMER, Sector-12, Chandigarh, India.
E-mail: siwatch1@yahoo.com
Postmenopausal bleeding may be a presenting complaint for genital tract malignancy. Benign uterine causes predominate while endometrial cancer contributes 10% of symptomatic cases. Extra-uterine causes are rare and include carcinoma cervix or hormone secreting tumours of the ovary. We report a case of 50-year-old postmenopausal lady that presented with postmenopausal bleeding. On evaluation, she was found to have a complex adnexal mass, normal ovarian tumour markers and endometrial histology was normal on biopsy. She underwent exploratory laparotomy and total abdominal hysterectomy with bilateral salpingo-oophorectomy. The postoperative diagnosis was cystadenofibroma of ovary. We reported this case because of its rare incidence and varied symptomatology and presentation on imaging. One should consider diagnosis of a cystadenofibroma of ovary when a postmenopausal lady presents with a triad of an adnexal mass, postmenopausal bleeding with normal endometrial evaluation.
Adnexal mass, Bleeding per vaginam, Ovarian neoplasm
Case Report
A 50-year-old postmenopausal lady presented to the outpatient department with postmenopausal bleeding. She attained menopause at the age of 45 and had two such episodes one month apart, each lasting for two to three days. She was a multiparous lady, obese with no medical co-morbidities. She had medical or family history of genital malignancies. She was not on any postmenopausal hormonal therapy.
The general physical examination and local examination of vulva, vagina and cervix were normal. Liquid based cytology of the cervix was negative for malignant cells. Ultrasound revealed a uterus of postmenopausal size with endometrial thickness of 8 millimeters and a right adnexal mass of 9.8×7×7 cm which was multicystic and multiloculated with no solid components. Left ovary had a cyst, with septations, of around 4×5×5 cm. Computed tomography scan suggested similar findings. Her CA-125 was 20 mIU/mL, which was within the range.
Provisional diagnosis of benign ovarian tumour was kept as her tumour markers were within the normal limit. She underwent endometrial biopsy which revealed a proliferative endometrial pattern. Exploratory laparotomy was done as a possibility of malignant ovarian tumour could not be ruled out considering her age and complexity of the mass. Intra-operative findings were of a multi-loculated complex solid cystic right adnexal mass of 12×8 cm; left ovary had a simple cyst; Uterus was normal and there was no ascites. No evidence of metastatic disease in pelvis or abdomen was found. Peritoneal washings were sent for malignant cytology and total abdominal hysterectomy with bilateral salpingoophorectomy was performed. Her postoperative period was uneventful.
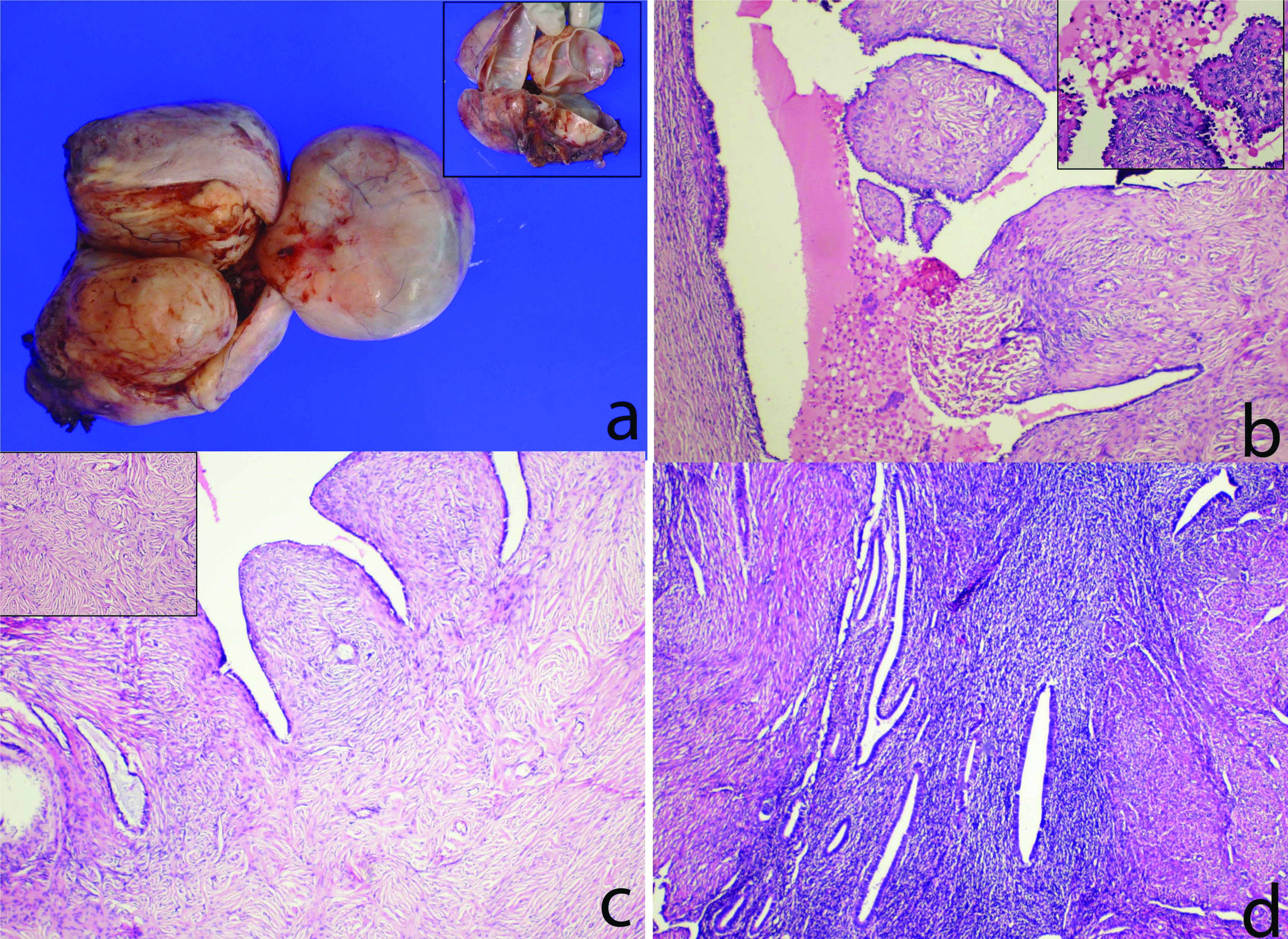
On histopathological examination, sections from left ovarian cyst showed multiple broad based papillae projecting into lumen with cuboidal epithelium and fibroblastic stroma, a focal area showing haemosiderin laden macrophages. Section from right ovarian cyst shown broad based papillae with fibroblastic stroma and scattered glands within stroma. Endometrium was in proliferative phase and myometrium shown focus of adenomyosis. Both fallopian tubes were free of tumour and peritoneal cytology was negative for malignant cells [Table/Fig-1]. She was followed-up for two years postoperatively and is doing well.
a) Gross specimen of uterus with right ovarian cyst, Inset: multiloculated cyst; b) Left ovarian cyst showing broad based papillae lined by cuboidal epithelium, projecting into the lumen with fibroblastic stroma and focal collection of haemosiderin laden macrophages (Haematoxylin and eosin, 40X), Inset: papillae with cuboidal epithelium (H&E, 100X); c) Right ovarian cyst showing broad based papillae with fibroblastic stroma and scattered glands within the stroma (H&E, 40X), Inset: dense fibroblastic stroma (H&E, 100X); d) Myometrium showing adenomyosis (H&E, 40X).
Discussion
Cystadenofibromas originate from the surface epithelium and ovarian cortex and constitute 1.7% of all benign ovarian tumours [1]. It has both epithelial and fibrous stromal components. Around 90% of these occur in women of 40 years and above, obese and if they are on hormone replacement therapy. Very rarely cystadenofibromas are reported in reproductive age group and teenagers as well [2]. It then requires a thorough preoperative evaluation to exclude a malignant aetiology so that a fertility sparing surgery is planned [1]. They are usually confined to one ovary; bilaterality is seen in 15% cases [3]. These tumours are either predominantly cystic, complex solid-cystic, multiloculated with thick septations (seen in 30% of cases) or predominantly solid with or without papillary projections (in around 50% cases). Few of these tumours may also demonstrate increased vascularity on color Doppler (characteristic pattern of high impedance and peripheral flow) [4,5]. Histology may be mucinous, serous, endometrioid or transitional epithelium.
The complex and varied presentation gives impression of a malignant ovarian tumour on imaging. Cho SM et al., in his study of 16 cases of cystadenofibroma evaluated by either CT scan or MRI showed that all of them were reported as malignant ovarian tumours [6]. On MRI, cystadenofibromas have a nodular or trabecular pattern. The finding that fibrous sepatations have low signal intensity on MRI, due to presence of a skeletal muscle component was first reported by Outwater EK et al., the cystic areas have high signal intensity on T2 weighted images which gives appearance of a black sponge [7]. The septations may show moderate enhancement on Gadolinium images [8,9].
When post-menopausal bleeding is the only presenting symptom in these women, endometrial biopsy is mandatorly done to rule out an endometrial carcinoma. Hormone producing malignant ovarian tumours like granulosa cell tumours may have a similar presentation but these tumours are usually solid. The cause for abnormal or postmenopausal uterine bleeding in woman with cystadenofibroma is attributed, by Czernobilsky B et al., to a possible but unproven endocrine effect of the tumour causing abnormal endometrial proliferation [10]. Singh N et al., reported a case of large functional benign endometroid cystadenofibroma of the ovary leading to endometrial cystic glandular hyperplasia and postmenopausal bleeding in a 75-year-old postmenopausal woman [11]. Immunohistochemical detection of sex steroid hormone or its biosynthesis enzymes such as P-450 aromatase, P-450 SCC, 3β-HSD and P-450 C17 in ovarian tumour tissue can be done to confirm the relationship with oestrogen synthesis by the tumour and its effect as genital bleeding.
Complications may be torsion or haemorrhage into the cyst which then may present as acute abdomen. Mechera R et al., reported a case of large bowel obstruction due to a large benign ovarian cystadenofibroma in a 60-year-old lady with Klippel feil syndrome. Gastrointestinal obstruction usually occurs as a complication of advanced ovarian cancer, but she had it following cystadenofibroma [12].
Management of serous cystadenofibroma of ovary is complete surgical removal of the tumour as they are unequivocally benign and have an excellent prognosis. No atypical or borderline cases have been reported till date. The diagnostic dilemma is that a malignant ovarian tumour persists at laparotomy as well and frozen section may prevent complete and extensive surgery especially in reproductive age group [1]. Cho DH reported a case of 34-year-old multiparous lady with a 6x3 cm complex adnexal mass, diagnosed as cystadenofibroma intraoperatively by frozen section. She was managed by laparoscopic right partial oophorectomy [13].
Fertility sparing surgery in the form of unilateral salpingo-oophorectomy is adequate in younger women if the tumour is confined to one ovary. However, since very few cases of cystadenofibroma were reported in woman of reproductive age, need for long term follow-up and the possible recurrence rate is unknown. In a study of 34 patients of benign serous cystadenofibroma of ovary by Czernobilsky B et al., the outcome with regard to tumour was favourable and similar in all patients whether the surgery was conservative like cystectomy/oophorectomy or extensive like total abdominal hysterectomy and bilateral salpingo-oophorectomy [10].
Conclusion
Postmenopausal bleeding is an important cause of concern in midlife women. Though the usual causes are confined to the uterus, ovarian cause is to be ruled out when endometrial histology is normal. The differential diagnosis of cystadenofibroma of ovary is thus to be kept when a peri or postmenopausal lady presents with a triad of postmenopausal bleeding, complex adnexal mass and a normal endometrial histology on biopsy.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
PLAGIARISM CHECKING METHODS: [Jain H et al.]
Plagiarism X-checker: Jul 09, 2019
Manual Googling: Jul 25, 2019
iThenticate Software: Aug 14, 2019 (9%)
[1]. Nisha M, Garima A, Sneh S, Parveen R, Bilateral serous papillary cystadenofibroma of the ovaries in a young femaleSouth Afr J Gynaecol Oncol 2012 4(2):69-70.10.1080/20742835.2012.11441199 [Google Scholar] [CrossRef]
[2]. Nasca D, Proliferating endometrioid cystadenofibroma of the ovary. Report of a case in a teenagerDiagn Gynecol Obstet 1982 2013:317-24. [Google Scholar]
[3]. Cotran RS, Kumar V, Collins T, Robbins pathologic basis of disease 1999 6th edPhiladelphiaW.B. Saunders [Google Scholar]
[4]. Jung DC, Kim SH, Kim SH, MR imaging findings of ovarian cystadenofibroma and cystadenocarcinofibroma: Clues for differential diagnosisKorean J Radiol 2006 7:1910.3348/kjr.2006.7.3.19916969050 [Google Scholar] [CrossRef] [PubMed]
[5]. Alcázar JL, Errasti T, Mínguez JA, Galán MJ, García-Manero M, Ceamanos C, Sonographic features of ovarian cystadenofibromas: spectrum of findingsJ Ultrasound Med 2001 20:915-19.10.7863/jum.2001.20.8.91511503928 [Google Scholar] [CrossRef] [PubMed]
[6]. Cho SM, Byun JY, Rha SE, Jung SE, Park GS, Kim BK, CT and MRI findings of cystadenofibromas of the ovaryEur Radiol 2004 14:798-804.10.1007/s00330-003-2060-z14504904 [Google Scholar] [CrossRef] [PubMed]
[7]. Outwater EK, Siegelman ES, Talerman A, Dunton C, Ovarian fibromas and cystadenofibromas: MRI features of the fibrous componentJ Magn Reson Imaging 1997 7:465-71.10.1002/jmri.18800703039170028 [Google Scholar] [CrossRef] [PubMed]
[8]. Takeuchi M, Matsuzaki K, Kusaka M, Shimazu H, Yoshida S, Nishitani H, Ovarian cystadenofibromas: Characteristic magnetic resonance findings with pathologic correlationJ Comput Assist Tomogr 2003 27(6):871-73.10.1097/00004728-200311000-0000714600453 [Google Scholar] [CrossRef] [PubMed]
[9]. Kim KA, Park CM, Lee JH, Kim HK, Cho SM, Kim B, Benign ovarian tumours with solid and cystic components that mimic malignancyAJR Am J Roentgenol 2004 182(5):1259-65.10.2214/ajr.182.5.182125915100129 [Google Scholar] [CrossRef] [PubMed]
[10]. Czernobilsky B, Borenstein R, Lancet M, Cystadenofibroma of the ovaryCancer 1974 34:1971-81.10.1002/1097-0142(197412)34:6<1971::AID-CNCR2820340616>3.0.CO;2-N [Google Scholar] [CrossRef]
[11]. Singh N, Tripathi R, Mala YM, Khurana N, Khan M, Large functional benign endometroid cystadenofibroma of the ovary leading to endometrial cystic glandular hyperplasia and postmenopausal bleedingBMJ Case Rep 2013 2013:bcr201301032310.1136/bcr-2013-01032323761571 [Google Scholar] [CrossRef] [PubMed]
[12]. Mechera R, Menter T, Oertli D, Hoffmann H, Large ovarian cystadenofibroma causing large bowel obstruction in a patient with Klippel-Feil syndrome: A case reportInt J Surg Case Rep 2016 20:17-20.10.1016/j.ijscr.2015.12.04626780471 [Google Scholar] [CrossRef] [PubMed]
[13]. Cho DH, Serous cystadenofibroma misdiagnosed as an ovarian malignancyBMJ Case Reports CP 2018 11:e22822310.1136/bcr-2018-22822330567152 [Google Scholar] [CrossRef] [PubMed]