Caesarean Section (CS) is the most common abdominal surgery in obstetrical practice. It is the mode of delivery of foetus through incision in the abdominal wall and the uterine wall after 28th weeks period of gestation. Sometime it may not be possible to carry out normal delivery safely due to maternal and/or foetal compromise [1]. Foetal distress, cephalo-pelvic disproportion, malpresentaion and placenta previa are some of the common causes which precludes safe vaginal delivary. In such situation CS plays a vital role in safe delivery. However, the unjudicial use of this surgical technique has led to the alarmingly high rate of CS delivery. The rate has increased dramatically over the past three decades both in the developed and in the developing world; 5% in early 1970s to more than 50% in some regions of the world in the late 1990s [1-3]. The increase in CS rate not only poses increase health risk to the mother but also increases the cost of health care [4]. The steady increase in CS has fueled the debate over acceptable rates of CS and the risk-benefit analysis in ensuring optimum maternal and perinatal outcomes in different populations with different access to health resources. WHO recommends CS rate of 15% and not to increase this threshold [5]. The rate of CS delivery is positively associated with postpartum antibiotic treatment and severe maternal morbidity and mortality [3]. Hence, this study was conducted to analyse the rate and indication for CS in our institute.
Materials and Methods
It was a retrospective study conducted in the Department of Obstetrics and Gynaecology, College of Medical Sciences- Teaching Hospital, Bharatpur, Nepal. It is a 1050 bedded private hospital with tertiary care facility. Before starting the study, ethical approval of the study was obtained from the Institutional review board (Reg. No. 23/76/77) of College of Medical Sciences. All the patients who underwent CS from February 2010 till February 2012 were included in the study and those who had any mode of delivery outside the hospital were excluded from the study. Various obstetrical parameters were analysed including rate and indications of CS.
Statistical Analysis
All data were analysed by using statistical package SPSS (version 10.0; SPSS Inc., Chicago, IL, USA). Descriptive analysis including range, mean, median, mode and standard deviation was used.
Results
Over the two years period, there were total of 1412 delivery in our hospital, out of which 412 (29.17%) had CS. The mean age of the patients who underwent CS was 24.44±4.23 years, ranging from 16 to 42 years. The mean period of gestation was 38.62±2.21 weeks (range 29.6 to 43.5 weeks). Most of the patients who underwent CS were Primigravida (54.4%), mean gravida was 1.74±1.17 (range 1-11) and 10 (2.4%) patients were grand multipara (2.3%). Out of 412 patients, most of them had LSCS on Emergency basis (n=326, 79.1%).
There were different indications for CCS as shown in [Table/Fig-1]. Hypertensive disorder of pregnancy accounted for CS delivery in 20 patients (4.8%), and severe preeclampsia (62%) was the most common cause followed by eclampsia (17%). Twenty five patients (6.1%) required CS delivery because of antepartum haemorrhage and Placenta Previa (n=16, 64%) was the commonest cause. There was no maternal mortality.
| Indication | Total number n=412 (%) |
|---|
| Maternal indication |
| Antepartum haemorrhage | 25 (6.1%) |
| Cephalopelvic Disproportion (CPD) | 13 (3.2%) |
| Arrest of descent and dilatation | 15 (3.6%) |
| Failed induction | 42 (10.1%) |
| Pregnancy induced hypertension | 20 (4.8%) |
| Previous CS | 70 (16.9%) |
| Foetal indication |
| Foetal distress | 40 (9.7%) |
| Oligohydraminos | 65 (15.8%) |
| Thick meconium stained liquor | 33 (8%) |
| Malpresentation | 56 (13.6%) |
| Miscellaneous | 33 (8%) |
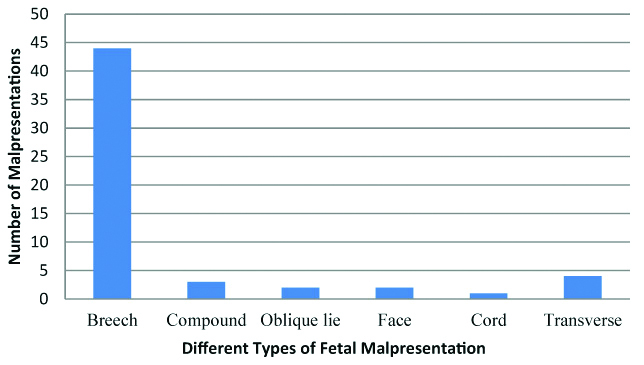
Out of 56 patients who had CS for malpresentation [Table/Fig-2], Breech presentation (78%) was the most common reason for CS, followed by Transverse presentation (7%), Compound presentation (5%), Oblique lie (4%), Face presentation (4%), and Cord prolapse (2%).
Different types of malpresentations.
Discussion
World Health Organisation (WHO) has suggested that a caesarean delivery rate of 15% should be taken as a threshold that should not be exceeded [5]. In certain condition like obstructed labour and complete placenta previa which occurs in 1-2% of all the birth, there is an absolute need of CS to save the maternal life. An extremely low rate also indicates the poor access to surgical care, which it true especially in economically challenged countries. The rate of at least 5% is necessary to deceased the maternal and foetal morbidity or mortality [5]. There is no consensus on the optimal rate of CS and varies widely. Although, CS is indicated in the complicated cases, the increase in CS rate above 10% has not been shown to improve maternal and foetal outcome, rather the rate above 15% have been shown to have adverse effect on the maternal and foetal outcome [5]. In the study by Souza J et al., they found that compared to spontaneous vaginal delivery, all other modes of delivery without medical indication was associated with the increased risk of death, admission to ICU, blood transfusion and hysterectomy, including antepartum CS [6].
CS rate vary according to the geographical region. A national wise survey from 1990-2011 showed that Nepal had the lowest rate of CS among the southern Asian countries (0.83% in 1996 to 4.59% in 2011) [5]. The study by WHO on Asian global survey on maternal and perinatal health (2007-08) [7], the CS rate ranged from 14.7 to 46.2%. Rate of CS in US is also as high as 32.8% [8]. The rate of CS has also been shown to vary between the rich and poor women. CS rates among the rich women were much higher but exceeded 15% only in Bangladesh, India and Pakistan, and highest been in Indian urban richer (21.75%). In Nepal, the caesarean rate (2003-2011) was highest among rich urban women (rural poorer=1.51% to urban richer=17.24%) [5]. CS delivery rate was also highest among highly educated mothers (13%), mothers in the highest wealth quintile (14%), urban births (15%), and first births (7%) [9]. Nepal is a financially underprivileged country, where most of the deliveries occurs at home and only one third of the deliveries occurred in the health facility; 26% are delivered in a public-sector health facility, and 7% in a private facility [9]. Our hospital is a Private medical institute, where most of the visiting patients are rich and educated mothers. This may explain the high rate of CS (29.17%) delivery in our hospital compared to National CS delivery rate (4.59% in 2011) [5]. During the WHO global survey (2005) [3], the median rate of CS was 33%, with the highest rates of caesarean delivery noted in private hospitals (51%, range 43-57). Other studies also correlate with the finding that cesarean delivery rate to be more in private hospitals as compared to government hospitals, almost three times more (45% to 80%) in private hospitals [10,11]. The rate of CS in our hospital is still very low as compared to private hospital of other part of the world.
One of the causes for increase in the CS rate is because of the maternal request, especially in the private hospital. This indication for CS was 1-48% in government hospital and in up to 60% in private clinics [12]. Similarly, according to Stjernholm YV et al., there is an increase in elective CS rate to 50.1%; and psychosocial indication (38.5%) was the most common indication followed by pathological foetal lie (21.4%) [13]. Most of our patients had emergency CS and only 20.9% patients had planned CS. Planned CS may decrease perinatal morbidity and mortality, pelvic floor dysfunction, early postpartum haemorrhage and obstetric shock [14]. The potential risks of caesarean delivery on maternal request should always be mentioned which include a longer maternal hospital stay, an increased risk of respiratory problems for the infant, and greater complications in subsequent pregnancies, including uterine rupture, abnormal placental implantation that may even require hysterectomy. Therefore, CS should be discouraged when there is no feto-maternal indication as it increases morbidity and mortality [6,7,15].
Different indications for CaesarianSection broadly classified into Maternal (e.g., CPD, Placenta Previa, Previous CS etc.,) and Foetal causes (e.g., Foetal distress, Malpresentation etc.,). The commonly reported indications for CS in Asia Global survey by WHO were Previous CS (24.2%), Cephalopelvic disproportion (22.6%), Foetal distress (20.5%), and Breech or other abnormal presentation (12.5%) [7]. In the study by Gao Y et al., nuchal cord was the most common reason for cesarean delivery (19.3%), followed by previous cesarean (13.6%), Foetal distress (11.8%), Malpresentation (11.0%) and Cesarean delivery on maternal request (9.1%) [16]. The study from eastern Nepal by Chhetri S et al., also had increased rate of CS deliveries from 29.2% to 33.7% in five years and the most common cause for CS delivery was constant; Meconium stained liquor (22.7%), Previous CS (15.6%), Breech presentation (12.1%), Foetal distress (6.5%), Non-progress of labour (6.5%), Cephalopelvic disproportion (5.3%) and Placenta Previa (5%) [17]. In our hospital major indication was Previous CS delivery (16.9%), Severe Oligohydraminos (15.8%), Malpresentation (13.6%), failed induction (10.1%) and Foetal Distress (9.7%), which is similar to above mentioned studies. Kambo I et al., found that, on the whole, repeat section contributed to 29% of their cases [18]. Previous CS delivery though shares major bulk for CS delivery in the subsequent pregnancy; several studies indicate that 33-75% of all women with previous cesarean delivery can be delivered vaginally particularly if the cesarean has been for a non-recurring indication with a smooth postoperative recovery [18,19].
Limitation
One of the major limitations is that the focus of this study was on private hospital and to only one, so the results cannot be generalised. Retrospective nature is the major limitation of this study.
Conclusion
Increased frequency of caesarean delivery do not necessarily indicate good quality care or services. The increased rate of CS is the big concern. Those who need a caesarean, it is essential to get one under optimum conditions and the others get proper care and support through labour so as to minimise damage and maximise satisfaction. Repeat CS may be avoided by giving trial of labour. There is a deem need for standardised collection of information on all aspects of childbirth to ascertain the incidence and causes of CS nationally so that the improvements in health care can be taken.