A Rare Case of Extensive Brain Calcinosis and Features of Parkinsonism Secondary to Iatrogenic Hypoparathyroidism
Kalaimani Sivamani1, R Prasanna Venkatesh2, A Tumbanatham3, Siva Ranganathan Green4
1 Assistant Professor, Department of General Medicine, Mahatma Gandhi Medical College and Research Institute, Puducherry, India.
2 Assistant Professor, Department of General Medicine, Mahatma Gandhi Medical College and Research Institute, Puducherry, India.
3 Associate Professor, Department of General Medicine, Mahatma Gandhi Medical College and Research Institute, Puducherry, India.
4 Associate Professor, Department of General Medicine, Mahatma Gandhi Medical College and Research Institute, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kalaimani Sivamani, Assistant Professor, Department of General Medicine, Mahatma Gandhi Medical College and Research Institute, Pillaiyarkuppam, Puducherry-607402, India.
E-mail: kalaimani.sivamani@gmail.com
Extensive intracranial calcification is rare in iatrogenic hypoparathyroidism and Parkinsonism at the time of diagnosis is uncommon. We report a case of a 55-year-old woman who presented to us 20 years after thyroid surgery with symptoms of hypocalcaemia and clinical features of Parkinsonism. On detailed evaluation, patient was found to have extensive calcification involving the basal ganglia, periventricular white matter and cerebellum and serum parathormone was low. With calcium and calcitriol supplementation there was symptomatic improvement however features of parkinsonism persisted. We present this case to highlight the unusual presentation of Parkinsonism in a patient with post-thyroidectomy hypoparathyroidism with brain calcinosis. This case also underscores the importance of regular follow-up of patients after thyroid surgery to detect hypoparathyroidism, the treatment of which could prevent future morbidity to the patient.
Calcification, Hypocalcaemia, Parathormone, Thyroidectomy
Case Report
A 55-year-old female presented with complaints of swelling of the right leg for 20 days following minor trauma to the dorsum of the foot. Other relevant history included spasms of the hand and perioral and acral paresthesia for past six months. There was also history of cognitive decline for the past one year. There was no history of seizures or headache. Significant medical history included thyroid surgery 20 years back, the details of which were not available and cataract surgery on both eyes 10 years back. Patient had not been previously evaluated for these complaints. On examination, patient was conscious, drowsy at the time of admission, blood pressure was 110/70 mm Hg with a pulse rate of 70/min. There was no pallor or icterus or lymphadenopathy. There was cellulitis of right leg with an ulcer over the dorsum of right foot. Other findings included mask like facies, a horizontal scar over the front of neck indicating prior thyroid surgery without any palpable swelling in the thyroid region. There was no mucocutaneous candidiasis or vitiligo. Cardiovascular and respiratory system examination were normal.
CNS examination revealed bradykinesia and cog wheel rigidity at the wrist however there was no tremors, deep tendon reflexes were normal and plantar was flexor. There was carpal spasm initially and Chvostek sign was positive and hence patient was further evaluated for hypocalcaemia. Investigations revealed an elevated leucocyte count of 20000, haemoglobin was 10 gm/dL, serum calcium was 3.1 mg/dL, albumin was 2.8 gm/dL, corrected serum calcium was 4.1 mg/dL, magnesium 1.1 mg/dL, potassium of 3 mEq/L, phosphate 5.6 mg/dL, and alkaline phosphatase of 145 U/mL. ECG showed prolonged QTc of 500 milliseconds. In view of severe hypocalcaemia, hyperphosphatemia, normal alkaline phosphatase levels the possibility of hypoparathyroidism was considered and iPTH was done which was 1.9 pg/mL (normal range 10 to 65 pg/mL). Patient was also found to have vitamin D deficiency with 25 hydroxyvitamin D (Vitamin D2) level being undetectable however with a normal vitamin D3 levels. Thyroid profile revealed a low free T4 (0.0905 ng/dL) and elevated TSH of 43 mIU/L.
Patient was initially treated with intravenous calcium gluconate infusion in view of symptomatic hypocalcaemia with prolonged QTc in ECG and also IV magnesium sulfate to correct hypomagnesemia. Intravenous antibiotics were given to treat cellulitis, thyroxine 50 mcg was added for hypothyroidism. Symptoms of carpal spasm and acral paresthesia improved after 24 hours of calcium infusion and oral calcium tablets was started (2 gm/day) along with calcitriol 0.25 mcg/day.
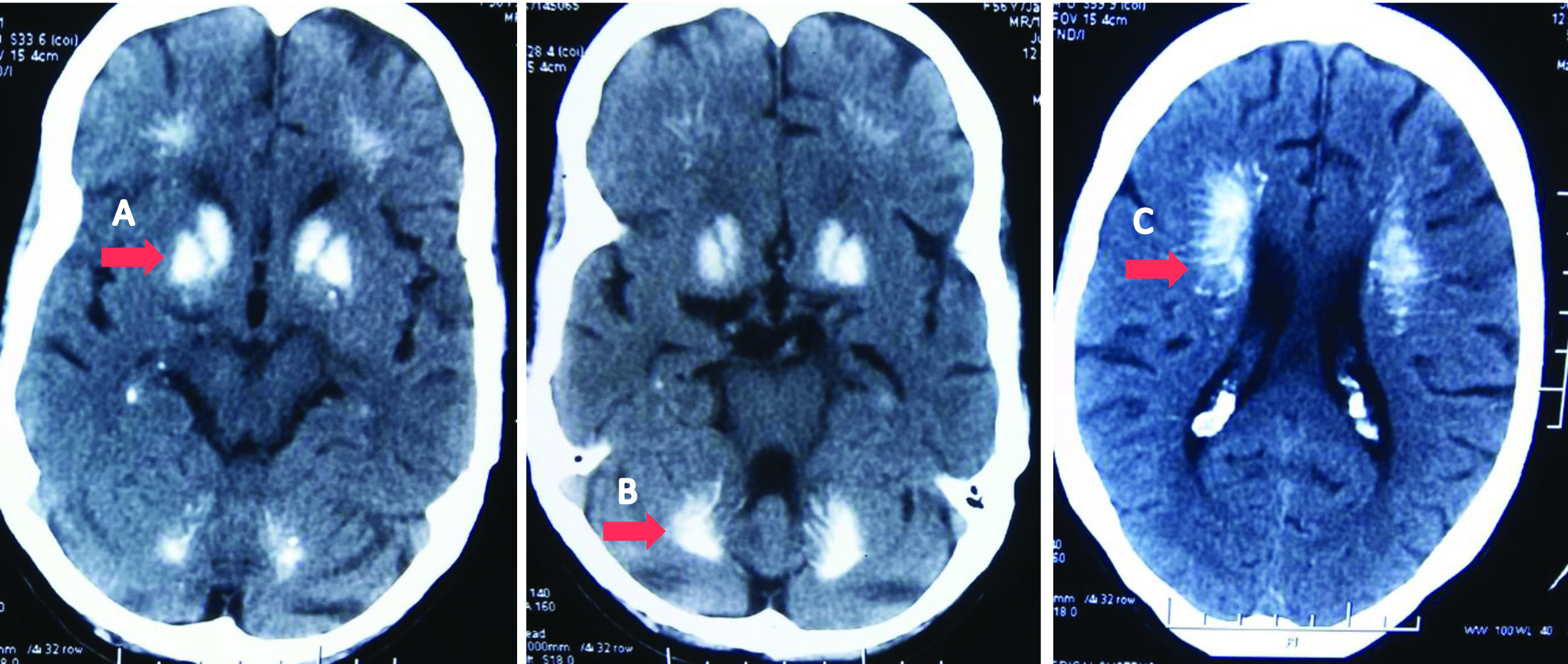
Ultrasonography of the neck was done which showed residual thyroid tissue, the parathyroid glands could not be visualised. A non-contrast CT of the brain was done in view of extrapyramidal features which showed extensive intracerebral calcification involving the basal ganglia, cerebellum, subcortical white matter of the frontal and parietal lobes [Table/Fig-1]. Ultrasonography of the kidneys did not reveal any calculi or nephrocalcinosis. Twenty four hour urine calcium was within normal limits. With treatment Trousseau and Chvostek sign became negative after 48 hours of admission, QTc normalised and serum calcium improved to 6.5 mg/dL (corrected calcium 7.5 mg/dL) after 7 days of treatment. The cellulitis of right leg resolved with antibiotics and patient was discharged.
Axial CT brain showing (A) Bilateral symmetrical calcification in basal ganglia (B) Bilateral symmetrical calcification in dentate nuclei of cerebellum (C) Bilateral periventricular calcification.
Discussion
Hypoparathyroidism is among the uncommon endocrine disorders in clinical practice. The causes for hypoparathyroidism include genetic, autoimmune, infiltrative or inadvertent injury during thyroid surgery. Hypoparathyroidism presents with symptoms of hypocalcaemia including seizures and tetany. Parkinsonism and movement disorders are rare manifestations. Physiological intracranial calcification is seen in 0.3 to 1.5% of cases [1]. Among the pathological cause for basal ganglia calcification hypoparathyroidism and pseudohypopathyroidism are the most common. Roentgenographic observation of symmetrical cerebral calcification associated with parathyroid insufficiency was first reported by Eaton LM and Haines SF, in 1939 [2]. Calcifications outside the basal ganglia are rare in iatrogenic hypoparathyroidism and few cases have been reported in literature [3-18].
Hypocalcaemia can be due to Parathyroid Hormone (PTH) deficiency, vitamin D deficiency, drugs or genetic causes. The evaluation of hypocalcaemia includes measurement of serum calcium and ionised calcium, albumin, phosphate, magnesium and alkaline phosphatase. The presence of hypocalcaemia and hyperphosphatemia indicate hypoparathyroidism as in the index case and measurement of intact parathormone levels will confirm the diagnosis. A similar biochemical profile is seen in pseudohypoparathyroidism however, PTH would be elevated in this case. The diagnosis of hypoparathyroidism usually requires excluding other causes of hypocalcaemia like hypomagnesemia and vitamin D deficiency. Hypomagnesemia is known to cause decreased secretion of parathormone and also resistance to PTH, however hypocalcaemia is usually mild in this scenario and gets promptly corrected with magnesium replacement. Though the index patient had hypomagnesemia it was not severe enough to cause significant hypocalcaemia. This patient also had vitamin D deficiency as evidenced by almost undetectable levels of 25 hydroxy vitamin D, however it solely cannot explain the hypocalcaemia as serum phosphorus tends to be low and PTH elevated in cases of vitamin D deficiency, which was otherwise in this case.
The common causes of hypoparathyroidism include post-surgical, autoimmune, infiltrative diseases and genetic causes. The incidence of hypoparathyroidism after thyroidectomy is 0.5 to 6.6% [19]. It may be transient or permanent and this is probably the case in the index patient. Though autoimmune diseases of the parathyroid can occur alone or as a part of autoimmune polyglandular syndrome, this seems unlikely in index patient. Hypoparathyroidism and pseudohypoparathyroidism are the two common conditions associated with basal ganglia calcification and patients can present with features of Parkinsonism as in this case. There are reports of improvement in the extrapyramidal manifestations with the correction of calcium and phosphate levels though improvement may not occur in all patients [20-25].
In a study involving 97 patients of hypoparathyroidism, the most common presenting symptom was seizures in approximately 50% of the patients [26]. Though the index patient had severe hypocalcaemia and also intracerebral calcification, there was no history of seizures, probably due to the physiological adaptations to the chronic hypocalcaemia. Another well-known presentation of hypoparathyroidism is with cataract. This patient was operated for cataract 10 years back, workup for the early onset cataract at that time may have led to an early diagnosis of hypoparathyroidism and an early treatment could have prevented the intracerebral calcification and the neurological consequences. In another study by Goswami R et al., out of 145 patient with idiopathic hypoparathyroidism 73.8% cases had basal ganglia calcification and Parkisonian features were present only in two cases [27].
Conclusion
This case highlights some of the unusual manifestations of postoperative hypoparathyroidism-extensive intracranial calcification and Parkinsonism, which can be prevented by regular long term follow-up post-surgery, considering the fact that the manifestations can be subtle and the presentation late.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
PLAGIARISM CHECKING METHODS: [Jain H et al.]
Plagiarism X-checker: Jul 24, 2019
Manual Googling: Aug 22, 2019
iThenticate Software: Sep 04, 2019 (3%)
[1]. Wong EM, Dahl M, Basal ganglia calcification in idiopathic hypoparathyroidismBCMJ 2013 55(10):462-65. [Google Scholar]
[2]. Eaton LM, Haines SF, Parathyroid insufficiency with symmetrical cerebral calcification: report of three cases, in one of which the patient was treated with dihydrotachysterolJournal of the American Medical Association 1939 113(9):749-53.0.1001/jama.1939.02800340019006 [Google Scholar] [CrossRef]
[3]. Bhimani S, Sarwar M, Virapongse C, Rojas R, Freilich M, Computed tomography of cerebrovascular calcifications in postsurgical hypoparathyroidismJournal of Computer Assisted Tomography 1985 9(1):121-24.10.1097/00004728-198501000-000223968258 [Google Scholar] [CrossRef] [PubMed]
[4]. Lang C, Huk W, Pichl J, Comparison of extensive brain calcification in postoperative hypoparathyroidism on CT and NMR scanNeuroradiology 1989 31(1):29-32. [Google Scholar]
[5]. Jorens PG, Appel BJ, Hilte FA, Mahler C, De Deyn PP, Basal ganglia calcifications in postoperative hypoparathyroidism: A case with unusual characteristicsActa Neurologica Scandinavica 1991 83(2):137-40.10.1111/j.1600-0404.1991.tb04663.x1902012 [Google Scholar] [CrossRef] [PubMed]
[6]. Heckmann JG, Lang CJ, Neundörfer B, Reversible dementia due to coexisting diseaseThe Lancet 2000 355(9220):207510.1016/S0140-6736(05)73530-3 [Google Scholar] [CrossRef]
[7]. Adorni A, Lussignoli G, Geroldi C, Zanetti O, Extensive brain calcification and dementia in postsurgical hypoparathyroidismNeurology 2005 65(9):150110.1212/01.wnl.0000182293.34015.a916275848 [Google Scholar] [CrossRef] [PubMed]
[8]. Rizvi I, Ansari NA, Mujahid Beg M, Shamim D, Widespread intracranial calcification, seizures and extrapyramidal manifestations in a case of hypoparathyroidismNorth American Journal of Medical Sciences 2012 4(8):36910.4103/1947-2714.9952322912949 [Google Scholar] [CrossRef] [PubMed]
[9]. Balachandran VK, Malavika B, Extensiveintra-cerebral calcification and uncontrolled seizures due to hypo-parathyroidismKerala Medical Journal 2013 6(3):76-78. [Google Scholar]
[10]. Zisimopoulou V, Siatouni A, Tsoukalos G, Tavernarakis A, Gatzonis S, Extensive bilateral intracranial calcifications: a case of iatrogenic hypoparathyroidismCase Reports in Medicine 2013 2013:93218410.1155/2013/93218423509468 [Google Scholar] [CrossRef] [PubMed]
[11]. Agarwal R, Lahiri D, Biswas A, Mukhopadhyay J, Maity P, Roy MK, A rare cause of seizures, parkinsonian, and cerebellar signs: Brain calcinosis secondary to thyroidectomyNorth American Journal of Medical Sciences 2014 6(10):54010.4103/1947-2714.14328725489568 [Google Scholar] [CrossRef] [PubMed]
[12]. Misra AP, Mishra R, Gupta A, Extensive cerebral calcification in hypoparathyroidism studiesJ of Evolution of Med and Dent Sci 2014 37(3):6:9589-93.10.14260/jemds/2014/3241 [Google Scholar] [CrossRef]
[13]. Chowdhury AW, Majumder SN, Amin MG, Islam KN, Saleh MA, Sabah KM, Recurrent seizure: An uncommon presentation of post thyroidectomy hypoparathyroidismJournal of Medicine 2015 16(1):56-58.10.3329/jom.v16i1.22406 [Google Scholar] [CrossRef]
[14]. Uyar T, Paksoy K, Çokluk C, Extensive bilateral basal ganglia and cerebellar calcification in Fahr’s syndrome after thyroidectomyMovement Disorders 2016 31(suppl. 2) [Google Scholar]
[15]. Kalsifikasyon İH, Diffuse cerebral calcification due to iatrogenic hypoparathyroidismTurk J Neurol 2017 23:130-31.10.4274/tnd.02693 [Google Scholar] [CrossRef]
[16]. Petrarca M, Scipioni R, Di Giosia P, Giorgini P, Ferri C, A case of brain calcifications in postsurgical hypoparathyroidismInternal and Emergency Medicine 2017 12(1):113-15.10.1007/s11739-016-1430-x26968176 [Google Scholar] [CrossRef] [PubMed]
[17]. Kamath SD, Rao BS, Delayed post-surgical hypoparathyroidism: The forgotten chameleon!J Clin Diagn Res 2017 11(2):OD07-09.10.7860/JCDR/2017/23609.926028384917 [Google Scholar] [CrossRef] [PubMed]
[18]. Ramos-Lopes J, Brás A, Morgadinho A, Moreira F, Acute generalized chorea, dystonia and brain calcifications: A case reportActaMedicaportuguesa 2019 32(5):402-06.10.20344/amp.1102631166902 [Google Scholar] [CrossRef] [PubMed]
[19]. Shoback D, HypoparathyroidismNew England Journal of Medicine 2008 359(4):391-403.10.1056/NEJMcp080305018650515 [Google Scholar] [CrossRef] [PubMed]
[20]. Berger JR, Ross DB, Reversible parkinson syndrome complicating postoperative hypoparathyroidismNeurology 1981 31(7):881-81.10.1212/WNL.31.7.8817195511 [Google Scholar] [CrossRef] [PubMed]
[21]. Uncini A, Tartaro A, Di Stefano E, Gambi D, Parkinsonism, basal ganglia calcification and epilepsy as late complications of postoperative hypoparathyroidismJournal of Neurology 1985 232(2):109-11.10.1007/BF003139104020389 [Google Scholar] [CrossRef] [PubMed]
[22]. Friedman JH, Chiucchini MI, Tucci JR, Idiopathic hypoparathyroidism with extensive brain calcification and persistent neurologic dysfunctionNeurology 1987 37(2):30710.1212/WNL.37.2.3073808313 [Google Scholar] [CrossRef] [PubMed]
[23]. Tambyah PA, Ong BK, Lee KO, Reversible parkinsonism and asymptomatic hypocalcaemia with basal ganglia calcification from hypoparathyroidism 26 years after thyroid surgeryAmerican Journal of Medicine 1993 94(4):444-45.10.1016/0002-9343(93)90159-M [Google Scholar] [CrossRef]
[24]. Abe S, Tojo K, Ichida K, Shigematsu T, Hasegawa T, Morita M, A rare case of idiopathic hypoparathyroidism with varied neurological manifestationsInternal Medicine 1996 35(2):129-34.10.2169/internalmedicine.35.1298680101 [Google Scholar] [CrossRef] [PubMed]
[25]. Ramis JN, Ibáñez AE, Irigoín RR, Artigas CF, Comas LM, Extrapyramidal symptoms due to calcinosis cerebri in a patient with unknown primary hypoparathyroidismEndocrinologia y nutricion (English Edition) 2012 1(59):69-71.10.1016/j.endoen.2011.03.003 [Google Scholar] [CrossRef]
[26]. Bhadada SK, Bhansali A, Upreti V, Subbiah S, Khandelwal N, Spectrum of neurological manifestations of idiopathic hypoparathyroidism and pseudohypoparathyroidismNeurology India 2011 59(4):58610.4103/0028-3886.8434221891938 [Google Scholar] [CrossRef] [PubMed]
[27]. Goswami R, Sharma R, Sreenivas V, Gupta N, Ganapathy A, Das S, Prevalence and progression of basal ganglia calcification and its pathogenic mechanism in patients with idiopathic hypoparathyroidismClinical Endocrinology 2012 77(2):200-06.10.1111/j.1365-2265.2012.04353.x22288727 [Google Scholar] [CrossRef] [PubMed]