Trans-catheter Device Closure of Ruptured Sinus of Valsalva Aneurysms using PDA Occluder Devices
Nathaniel Samson1, Lijo Varghese2, Oommen George3, George Joseph4, Paul George5, John Roshan6
1 Assistant Physician, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
2 Associate Professor, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
3 Professor, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
4 Professor, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
5 Professor, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
6 Professor, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Lijo Varghese, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
E-mail: lijo97@gmail.com
Introduction
Ruptured Sinus of Valsalva (RSOV) is a rare congenital heart disease. Indian data regarding trans-catheter device closure of RSOV is limited. In the current study we aim to look at the feasibility of using a Patent Ductus Arteriosus (PDA) occluder device for this purpose as it is a much economical alternative to the conventional devices.
Aim
To study the immediate and intermediate term follow-up after RSOV device closure using PDA device.
Materials and Methods
This retrospective analysis, from a large tertiary care hospital in South India, included 24 patients who underwent trans-catheter device closure of RSOV between December 2004 and December 2017, mostly using PDA occluders devices. Patient demographics, clinical characteristics, procedural and device related variables; immediate outcomes during hospital stay were collected from medical records. Follow-up data for residual shunt and complications were also collected. For the descriptive analysis, all continuous variables are expressed as mean values and standard deviation or median with range as appropriate, and discrete variables are presented as percentages.
Results
Of the 24 patients 75% were males; the mean age was 35 years (range: 12-61 years). Twenty three PDA occluders (Lifetech, Cardi-O-Fix) and 1-vascular plug were used in total. Successful device closure was achieved in 21 patients (87.5%) and the result was sustained at 6 months follow-up (median follow-up was 8 months). There was one procedure related mortality (immediate) due to aneurysm rupture, one patient was referred for surgical closure (one week after percutaneous procedure) due to persistent shunt across the defect and another referred for surgery due to device embolization (after 24 hours of the procedure). No other procedure related complications such as significant aortic regurgitation or coronary artery occlusion occurred.
Conclusion
Trans-catheter device closure of RSOV using PDA device occluder is a safe, feasible, effective and economical modality of treatment with good short-term and intermediate outcomes. In carefully selected patients this provides an attractive alternative to surgical closure, thereby avoiding the inherent morbidity of sternotomy and cardiopulmonary bypass.
Aortic regurgitation, Duct occluders, Ruptured aneurysm, Trans-catheter intervention
Introduction
Sinus of Valsalva Aneurysm (SVA) is a rare cardiac anomaly which is usually congenital (incidence of 0.1% and accounts for 3.5% of all congenital heart disease) and can rarely be acquired (complication of bacterial endocarditis, syphilis, Behcets disease, trauma) [1]. Associated cardiac anomalies such as ventricular septal defect or aortic regurgitation may be present in 30-40% cases. The pathology has been attributed to weakness of the elastic lamina at the junction of the aortic media and the annulus fibrosis. Most patients with un-ruptured SVAs may remain asymptomatic and thus undetected. Due to continuous exposure to the high aortic pressures, 35% of all SVAs rupture mostly into the right side of the heart leading to continuous left to right shunt and symptoms. Seventy percent originate from the right coronary sinus; 80% of patients with RSOV are symptomatic [1] and they usually present with acute to subacute onset exertional dyspnea and palpitations, at times heart failure and even cardiogenic shock [2].
Prompt recognition of the anomaly and further treatment is crucial for the patient’s survival. Untreated RSOVs patients have an average survival of 1 year only [2]. Traditionally, RSOVs have been treated using surgical techniques with either a primary closure (in small defects) or a patch closure (in larger defects). However, since the first trans-catheter device closure of RSOV was done by Cullen S et al., in 1994 using a Rashkind umbrella [3], the procedure has been used in many centers. The advantages of a percutaneous procedure over an open closure has attracted physicians world over to attempt device closure of RSOV using a variety of devices such as PDA or VSD occluder or Amplatzer Vascular plug with good immediate and intermediate outcomes [4-6]. Indian studies regarding the same are limited except the study by Mahimarangaiah J et al., in which all the above devices have been successfully used [7].
The aim of the study was to assess the feasibility of closing RSOV using a PDA device due to its economical and anatomical advantages. Here we present patients who underwent trans-catheter closure of RSOVs over the last 13 years with PDA device.
Materials and Methods
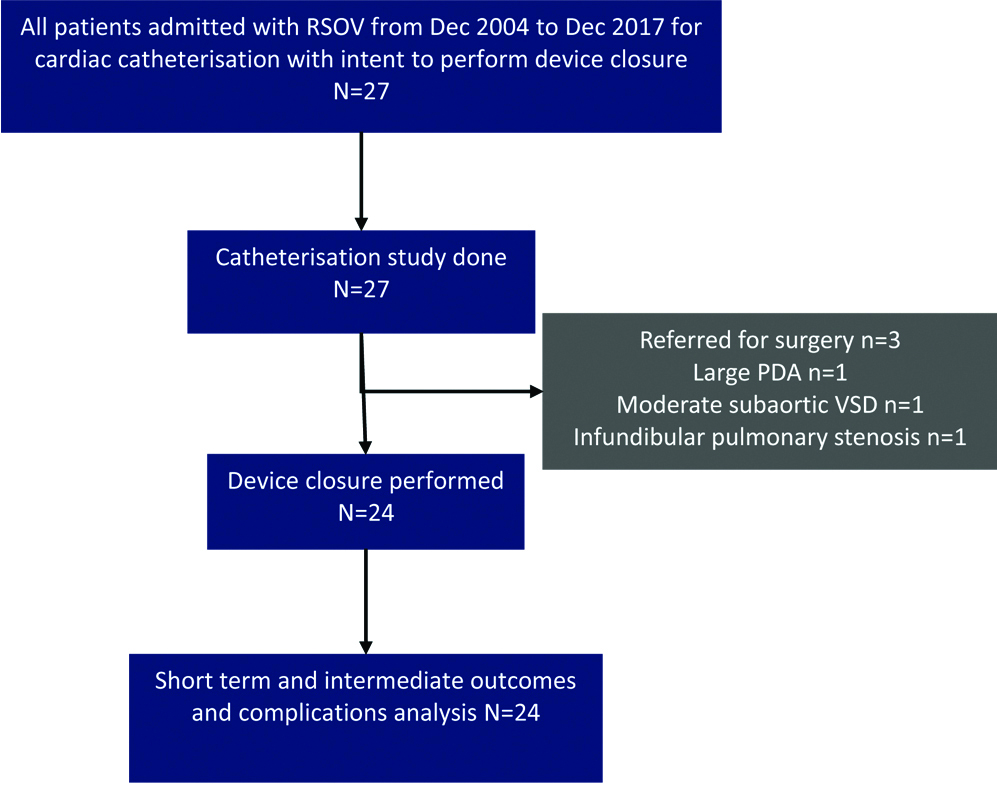
A retrospective study was conducted in March 2019 after taking the clearance from the Institutional Review and Ethics committee (approval letter number 4240/19). The medical records from December 2004 to December 2017 were reviewed retrospectively. There were 27 patients who were admitted with a diagnosis of RSOV for trans-catheter closure of the defect. Of these trans-catheter device closure was performed on 24 patients and 3 patients were referred for surgical closure due to associated cardiac lesions requiring surgery (one patient had infundibular pulmonary stenosis, the second had moderate sized sub-aortic ventricular septal defect not amenable to trans-catheter device closure and the third patient had a large PDA which could not be closed with a device). After the routine blood investigations, electrocardiography, chest radiography, transthoracic and transesophageal echocardiography, the patients were admitted for trans-catheter device closure once written consent was obtained.
The data regarding patient’s demographic details, chief symptoms at presentation, electrocardiography reports, echocardiographic details and details about follow-up were obtained from the medical records. Procedural details were collected from the medical records and by reviewing the angiographic images.
Statistical Analysis
All continuous variables are expressed as mean values and standard deviation or median with range as appropriate, and discrete variables are presented as percentages.
Results
There were 24 patients who underwent trans-catheter device closure of RSOV [Table/Fig-1]. There were 18 males (75%). The median age of the patients was 34.5 years. Most of the patients were in NYHA class II (n=19), 4 patients were in NYHA class III/IV (in heart failure) and one patient was in NYHA class I. The most common symptom was dyspnea which was found in 20 patients (83.3%) [Table/Fig-2]. The mean diameter of the defect as measured by echocardiogram prior to the procedure was 6.3±1.7 mm. In 17 (71%) patients the RSOV was from the right coronary cusp and in 7 (29%) patients it was from the non-coronary cusp. In majority the RSOV was draining into the right ventricle in 13 (54.1%) patients [Table/Fig-3]. The median hospital stay was 3 days.
This depicts the total number of patients in whom RSOV device closure was attempted.
| Total N=24 (%) |
|---|
| Age-mean (years) | 34.9±12.3 years |
| Males | 18 (75%) |
| Symptoms |
| Dyspnoea | 20 (83.3%) |
| Palpitation | 14 (58.3%) |
| Preceding chestpain | 3 (12.5%) |
| History of CCF | 3 (12.5%) |
| NYHA Class I | 1 (4.1%) |
| Class II | 19 (79.1%) |
| Class III/IV | 4 (16.6%) |
| Haemoglobin gm% (Mean) | 13.2±1.8 gm% |
| Creatinine mg/dL | 0.9±0.2 mg/dL |
| Total N=24 (%) |
|---|
| Size of defect-mean | 6.35±1.7 mm |
| Mean aortic pressure | 85±15 mm Hg |
| Mean PA pressure | 25.4±8.6 mm Hg |
| Ruptured sinus |
| RCC (Right coronary cusp) | 17 (70.8%) |
| NCC (Non coronary cusp) | 7 (29.1%) |
| Draining chamber |
| RCC to right atrium | 4 (16.6%) |
| RCC to right ventricle | 10 (41.6%) |
| RCC to right ventricular outflow tract | 2 (8.3%) |
| RCC to left ventricle | 1 (4.1%) |
| NCC to right atrium | 4 (16.6%) |
| NCC to right ventricle | 3 (12.5%) |
| Associated aortic valve regurgitation |
| Nil | 16 (66.6%) |
| 1+ | 5 (20.8%) |
| 2+ | 3 (12.5%) |
| Arteriovenous loop | 23 (95.8%) |
| Arterio-arterial loop | 1 (4.1%) |
| Median fluoroscopy time | 13.5 minutes |
| Median procedure time | 55 minutes |
| Residual shunt |
| Immediate post device release | 5 (20.8%) |
| 24 hours post procedure | 1 (4.1%) |
| Significant increase in aortic regurgitation | 0 |
| Post procedure LV systolic dysfunction | 1 (4.1%) |
| Median duration of hospital stay | 3 days |
Procedural Details
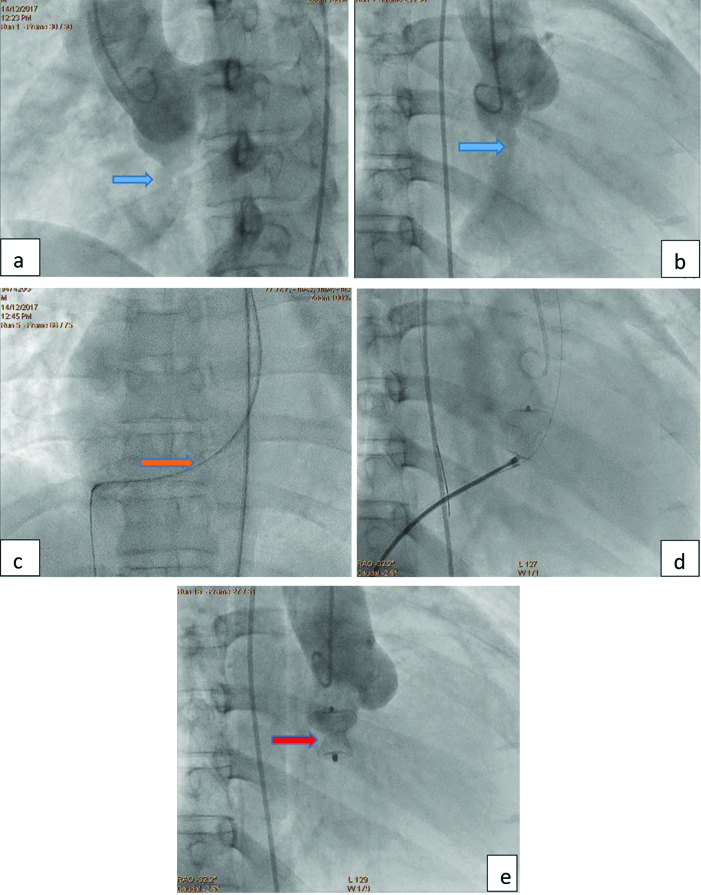
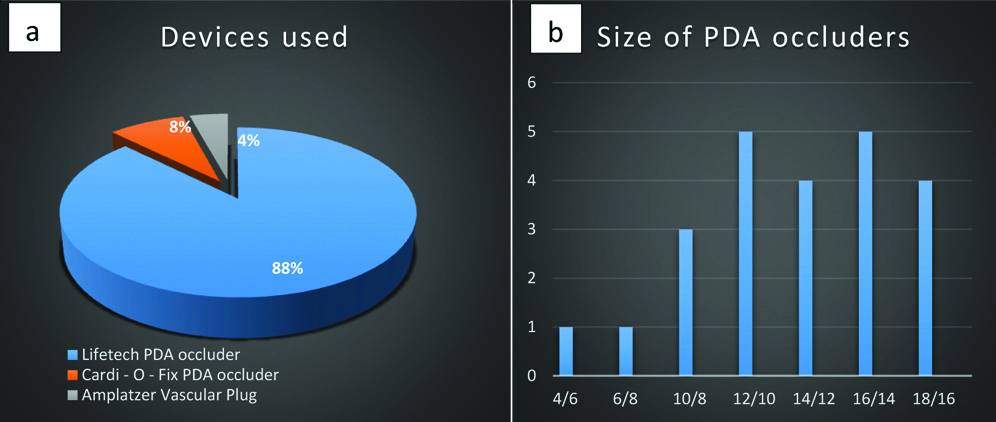
The mean diameter of the defect according to the angiographic measurement was 6.3±1.7 mm [Table/Fig-3]. An arterio-venous guide wire circuit was created in all patients [Table/Fig-4] except one in whom the RSOV was draining into the left ventricle and hence an arterio-arterial guidewire circuit had to be established. In 21 patients Heart and CeraLifetech PDA occluder (both ShenZhenLifetech Scientific Inc., China) sizes ranging from 10 to 18 mm were used, in 2 patients Cardi-O-Fix PDAOccluder (Starway Medical Corporation, China), sizes of 12 and 14 mm were used and in one patient AmplatzerTM Vascular Plug II of size 8 mm (AGA Medical Corporation, Golden Valley, Minnesota, USA) was used, as shown in [Table/Fig-5]. The median fluoroscopic time was 13.5 minutes and the mean procedure time was 62.8±17.8 minutes. Access site haemostasis was achieved by manual compression in all cases.
AV loop.
a. Aortogram in LAO view
b. Aortogram in RAO view
(Blue arrow indicates the defect in both the views)
c. Establishing Arteriovenous (AV) guidewire circuit (Orange arrow indicates the AV loop)
d. RAO view showing the device positioned across the defect
e. RAO view showing final aortogram and no residual flow across the shunt
(Red arrow shows the device after successful deployment)
a) It shows the devices used (all except one was PDA occluder). b) Various PDA occluder device sizes used.
Complications
Post procedure there was no increase in aortic regurgitation in any of the patients-five patients (20.8%) had trivial shunt at the end of the device closure angiographically, 1 patient had intra-procedure rupture of the aneurysmal sac during device deployment resulting in mortality. One patient had significant shunt at the end of the procedure which persisted beyond 1 week and was subsequently referred for surgical closure. A third patient had to be referred for surgery because of device embolization into branch pulmonary artery on the left side, detected by echo on day 2 post procedure. There were no access site complications, stroke, or coronary occlusions due to device impingement in any of the patients. One patient developed pulmonary oedema post procedure which was successfully managed medically.
Follow-Up
The median follow-up was after 8 months. All patients except one, had no residual shunt as assessed by transthoracic echocardiogram at 6 months follow-up. The one patient with a residual shunt had a gradient of 96 mm Hg across the shunt, suggesting that the shunt was restrictive. All patients who successfully underwent trans-catheter device closure were in NYHA class I at follow-up and asymptomatic. All patients had normal LV systolic function and normal LV dimensions at follow-up.
Discussion
In the present series, successful device deployment without immediate or intermediate complications was achieved in 21 of the 24 patients (87.5%) in whom the procedure was attempted. All but one patient had complete occlusion of the defect and no residual shunt across the defect at 6 months follow-up. The rate of successful closure of RSOV in the present series was similar compared to data from other studies which are approximately 75-85% [4-7].
RSOVs are more common in Asian males and various reports have quoted a male: female ratio ranging from 1.7:1 to 4:1 [8,9]. In the present series the male: female ratio was 3:1. Clinical presentation of RSOVs can be myriad-ranging from asymptomatic individuals to patients with overt heart failure. In the present series the most common symptom was dyspnea followed by palpitations. All patients were admitted for cardiac catheterization study with intent to perform a device closure. However, in 3 patients the procedure was not performed due to reasons stated earlier and they were referred for surgical closure.
There are multiple variables that affect the probability of a successful device closure including the size and morphology of the defect, the proximity of defect to the respective coronary arteries, the degree of aortic valve incompetence, vascular accessibility and the choice of device used for the procedure [7]. In the present series an arteriovenous guidewire circuit was established in all patients but one in whom the defect was draining into the left ventricle and consequently an arterio-arterial guidewire circuit was established. PDA occluders were used in 23 patients (95.8%) with sizes ranging from 12/10 mm to 18/16 mm and in one patient an Amplatzer Vascular plug II-8 mm size was used. PDA occluders are cost effective and also offer the advantage of being available across a wide range of sizes which made us choose them more often over the other available devices. In the study by Mahimarangaiah J et al., PDA devices were used in 70% of the patients [7].
There are a number of complications that have been reported after trans-catheter device closure of RSOV. Some of them include device slippage and embolization requiring surgical retrieval, aortic valve regurgitation, coronary occlusion due to device impingement, right ventricular outflow tract obstruction due to protrusion of the device, device infection, haemolysis, and Left Ventricular (LV) systolic dysfunction post procedure [4-7]. The patient with pulmonary oedema post procedure, secondary to LV systolic dysfunction, had normal LV systolic function at 3 month follow-up.
Limitation
This was a single center retrospective analysis and the sample size is relatively small. Given that the disease is uncommon, we have tried to analyse data of last 13 years. Considering that the study was done in a large tertiary care referral centre, an inherent referral bias cannot be excluded. Follow-up echocardiogram data, though not available for all patients at 6 months post procedure, was available at varying time periods during the course of their follow-up.
Conclusion
From the results of the data we can conclude that trans-catheter device closure of RSOVs is a safe, feasible and effective modality of definitive treatment with favourable short and intermediate outcomes in carefully selected patients. Hence the procedure provides an attractive alternative to surgical closure, thereby avoiding the inherent morbidity of sternotomy and risks of cardiopulmonary bypass.
Author Declaration:
Financial or Other Competing Interests: No
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? NA (Retrospective Study)
For any images presented appropriate consent has been obtained from the subjects. NA
PLAGIARISM CHECKING METHODS: [Jain H et al.]
Plagiarism X-checker: Jul 24, 2019
Manual Googling: Aug 05, 2019
iThenticate Software: Sep 04, 2019 (5%)
[1]. Kirklin JW, Barratt-Boyes BG, Congenital sinus of Valsalva aneurysm and aortico-left ventricular tunnel. In: Kirklin JW, Barratt-Boyes BG,, edsCardiac Surgery 2003 3rd edNew YorkChurchill-Livingstone:911-27. [Google Scholar]
[2]. Shah RP, Ding ZP, Ng AS, Quek SS, A Ten-Year review of ruptured sinus of Valsalva: Clinico-pathological and echo-Doppler featuresSingapore Med J 2001 42:473-76. [Google Scholar]
[3]. Cullen S, Somerville J, Redington A, Trans-catheter closure of a ruptured aneurysm of the sinus of ValsalvaBr Heart J 1994 71:479-80.10.1136/hrt.71.5.4798011415 [Google Scholar] [CrossRef] [PubMed]
[4]. Kerkar PG, Lanjewar CP, Mishra N, Nyayadhish P, Mammen I, Transcatheter closure of ruptured sinus of Valsalva aneurysm using the Amplatzer duct occluder: immediate results and mid-term Follow upEur Heart J 2010 31:2881-87.10.1093/eurheartj/ehq32320829209 [Google Scholar] [CrossRef] [PubMed]
[5]. Tong S, Zhong L, Liu J, Yao Q, Shu M, Song Z, The immediate and Follow up results of trans-catheter occlusion of the ruptured sinus of Valsalva aneurysm with duct occluderJ Invasive Cardiol 2014 26:55-59. [Google Scholar]
[6]. Zhao SH, Yan CW, Zhu XY, Li JJ, Xu NX, Jiang SL, Trans-catheter occlusion of the ruptured sinus of Valsalva aneurysm with an Amplatzer duct occluderInt J Cardiol 2008 129:81-85.10.1016/j.ijcard.2007.06.02217659794 [Google Scholar] [CrossRef] [PubMed]
[7]. Mahimarangaiah J, Chandra S, Subramanian A, Srinivasa KH, Usha MK, Manjunath CN, Trans-catheter closure of ruptured sinus of valsalva: different techniques and mid-term Follow upCatheterization and Cardiovascular Interventions 2016 87(3):516-22.10.1002/ccd.2610726255646 [Google Scholar] [CrossRef] [PubMed]
[8]. Perloff JK, Congenital Aneurysms of the Sinuses of Valsalva. In: Perloff JK, editorThe Clinical Recognition of Congenital Heart Disease 2003 5th edPhiladelphiaSaunders WB:457-70. [Google Scholar]
[9]. Moustafa S, Mookadam F, Cooper L, Adam G, Zehr K, Stulak J, Sinus of valsalva aneurysms-47 years of a single center experience and systematic overview of published reportsAm J Cardiol 2007 99:1159-64.10.1016/j.amjcard.2006.11.04717437748 [Google Scholar] [CrossRef] [PubMed]