Giant Bullous Reaction in Response to Tuberculin Test in a Patient of Pelvic Inflammatory Disease
Gopal Chawla1, Ram Niwas2, Naveen Dutt3
1 Senior Resident, Department of Pulmonary Medicine, AIIMS, Jodhpur, Rajasthan, India.
2 Assistant Professor, Department of Pulmonary Medicine, AIIMS, Jodhpur, Rajasthan, India.
3 Associate Professor, Department of Pulmonary Medicine, AIIMS, Jodhpur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Ram Niwas, Assistant Professor, Department of Pulmonary Medicine, AIIMS, Jodhpur, Rajasthan, India.
E-mail: rniwasaiims@gmail.com
Tuberculin test is an example of delayed hypersensitivity type reaction. Most of the patients develop mild reaction in form of erythema and induration by 24 hours, which reaches epitome at 48 to 72 hours. Hereby the case of a middle aged female who presented with vaginal brownish discharge along with lower abdominal pain and primary infertility has been reported . Transvaginal ultrasonography showed right adnexal mass suggestive of hydrosalpinx. Intradermal tuberculin test was performed which atypically lead to formation of giant bulla of size 30×32 mm by 12 hours. We report this exaggerated response to a standard 5TU tuberculin test, which was later diagnosed as tubercular lymphadenitis with tubercular pelvic inflammatory disease that may be the reason for primary infertility.
Atypical mantoux, Hydrosalpinx, Primary infertility
Case Report
A 46-year-old female case of primary infertility presented with lower abdominal pain and occasional pervaginal brownish discharge, while being worked up for primary infertility. Ultrasound showed right adenexal mass. The patient had no constitutional symptoms of tuberculosis and malignancy like loss of weight, loss of appetite, fever and chronic cough. There was no history of tuberculosis or contact with tuberculosis patient. The patient presented with no comorbidities and her vitals were within normal limits.
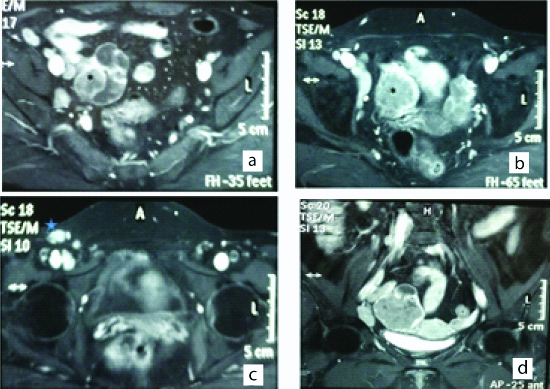
To rule out tubercular pelvic inflammatory disease, as it is one of the common causes of hydrosalpinx, intradermal tuberculin test was performed using 5 tuberculin units. It showed a strongly positive reaction with formation of bulla of size 30×32 mm in 12 hours, and induration of 45×40 mm by 24 hours [Table/Fig-1]. Normal chest radiography and negative sputum for acid fast bacilli ruled out pulmonary tuberculosis. Ultrasound upper abdomen was within normal limits while pelvic ultrasound and transvaginal ultrasound showed right bulky adnexa with hydrosalpinx which was also seen on Magnetic resonance imaging of abdomen as enlarged polylobulated mass in right hemi-pelvis and was inseparable from ipsilateral ovary. It showed isointense signals on T1W and mildly hyper-intense heterogeneous signals on T2W. Dilated tortuous intercommunicating fluid isointense structure represented hydrosalpinx. Necrotic lymph node was seen in the right iliac group location measuring 35×16 mm, along with multiple inguinal lymph nodes, largest measuring 24×14 mm [Table/Fig-2].
Standard Tuberculin test showing a strongly positive reaction with formation of a giant bulla, by 12 hours.

T1W image showing polylobulated mass (asterix) measuring 4.5×4.7×5 cm in the right pelvis; b) Tortuous intercommunicating fluid isotense structure: fallopian tube; c) Showing superficial right inguinal node (star) measuring 24×14 mm; d) Enlarged right iliac nodes.
Excision lymph node biopsy of inguinal lymph node showed caseating necrotizing granulomas along with Acid Fast Bacilli (AFB). Punch biopsy of bulla showed denuded lining epithelium with presence of ulcer comprising of marked oedema, presence of dense acute inflammatory infiltrate. There were few necrotic keratinocytes with neutrophilic infiltrate. Dermis also showed dense perivascular acute and chronic inflammation. Bulla, after biopsy, transformed into scab and area around bulla became indurated. Patient was started with anti-tubercular treatment and underwent right oophrosalpingectomy. The patient is presently continuing with continuation phase of anti-tubercular regimen. The patient experienced no complications and is on regular follow-up.
Discussion
Tuberculin Test is one of the investigations which is more than 100-year-old and is still widely used as an important test for supporting the diagnosis of tuberculosis [1]. A standardised 5TU (tuberculin units) of Purified Protein Derivative (PPD) is injected intradermally into volar surface of left forearm and delayed hypersensitivity reaction is noted by measuring the induration after 48-72 hours. An induration of 10 mm and more is regarded as a positive test response in immuno-competent individuals, whereas a response of 5 mm may be considered as positive in immuno-suppressed individuals like those with HIV infection or those on immuno-suppressive drug therapy. An erythema and induration is a normal response, while reactions such as blisters, granulomas and local necrosis after a PPD test, is very rare, and considered atypical [2].
The index case had a tubercular lymphadenitis with tubercular hydrosalphinx. Patient developed a massive bulla following intra-dermal tuberculin test in just 12 hours, which is not very typical for the delayed hypersensitivity reaction. It is difficult to explain the cause of this bullous atypical reaction [3]. Patients with active tuberculosis usually have high mycobacterial antigen load or at times are contacts of tuberculosis patients and rarely as a hypersensitivity phenomenon. Although Mantoux test is a sensitive but non-specific test, in the diagnosis of active tuberculosis, it needs to be correlated to the patient’s clinical context, for assisting the diagnosis [4].
There are no case available in literature where tubercular pelvic inflammatory disease had been associated with such an atypical mantoux test, while few reports mention similar reaction in cervical and mediastinal lymphadenopathy [5,6].
A massive bullous reaction i.e., atypical reaction to tuberculin is seen occasionally in patients with lepromatous leprosy. A temporary immune dysregulation along with changing level of antigenic load has been postulated as the cause for such giant reaction in lepromatous leprosy though exact mechanism is not clearly understood [7].
Induration of more than 20 mm is known as strong reactors and has more chances of having active tuberculosis than those with the commonly defined 10 mm induration [8].
Conclusion
Despite utility of tuberculin tests are limited in developing countries like India it is often useful test for assessing the prevalence of tuberculosis infection in the community. At times atypical tuberculin test points towards active tuberculosis infection. Tuberculin test (Mantoux) should be administered with care and interpreted with caution. Atypical, early or exaggerated response at times point towards active disease with high mycobacterial load.
Financial or Other Competing Interests
None.
Patient permission was obtained for publication of this work.
[1]. Mantoux MC, Lavoieintradermique en tubercalinothérapiePresse Med 1912 2013:146-48. [Google Scholar]
[2]. Blossom AP, Cleary JD, Atypical tuberculosis skin test reactionAnn Pharmacother 2003 2013:45110.1345/aph.1A29812639180 [Google Scholar] [CrossRef] [PubMed]
[3]. Nayak S, Acharjya B, Mantoux test and its interpretationIndian Dermatol Online J 2012 3(1):02-06.10.4103/2229-5178.9347923130251 [Google Scholar] [CrossRef] [PubMed]
[4]. Avasthi R, Chaudhary SC, Mohanty D, Giant Mantoux reactionIndian J Med Microbiol 2009 27(1):78-79. [Google Scholar]
[5]. Al Aboud D, Bullous reaction to a Mantoux test; a case report and review of the literatureOur Dermatology Online 2016 7(2):195-97.10.7241/ourd.20162.53 [Google Scholar] [CrossRef]
[6]. Bullous Mantoux Reaction-Newzealand Medical Journal [Internet]. [cited 2019 Jul 16]. Available from: http://www.nzma.org.nz/journal/read-the-journal/all-issues/2010-2019/2015/vol-128-no-1425-20-november-2015/6732 [Google Scholar]
[7]. Waters MF, Stanford JL, Giant reactions to tuberculin in lepromatous leprosy patientsInt J Lepr Other Mycobact Dis 1985 53(4):546-53. [Google Scholar]
[8]. El-Ansary EH, Grange JM, Qualitative differences in tuberculin reactivity in patients with tuberculosis, occupational contacts and non-contactsTubercle 1984 65(3):191-94.10.1016/0041-3879(84)90074-6 [Google Scholar] [CrossRef]