Case Report
A 31-year-old female with a history of blurring of vision in her left eye since August 2014. The patient was apparently well before August 2014. Her symptoms started suddenly, prompting her to seek an ophthalmic consultation. She was diagnosed with CRVO with severe macular oedema. She underwent one intravitreal injection, which gave slight relief. She consulted Sreedhareeyam Hospital in October 2014 and was advised on Inpatient (IP) management. She was neither diabetic nor hypertensive, and she does not present with dyslipidemia. Her personal history was normal. Her immediate family members do not report similar complaints.
Distant Visual Acuity (DVA) was 6/6 in her right eye (OD) and 6/36 in her left eye (OS). Anterior segment examination was normal in both eyes.
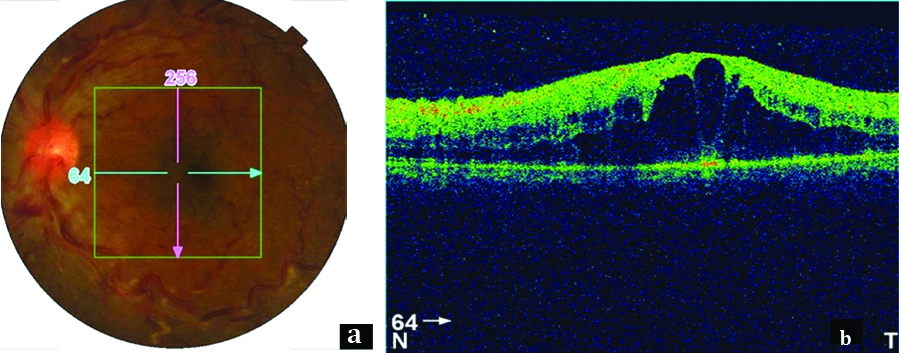
Posterior segment exam OS showed haemorrhages, cotton-wool spots, tortuous blood vessels, and a dull foveal reflex indicating macular oedema [Table/Fig-1a]. OCT OS along the naso-temporal plane showed an elevation at the macular region with a hyporeflective area within the elevation [Table/Fig-1b].
a) Fundus photograph OS showing haemorrhages, tortuous blood vessels, cotton-wool spots, and dull foveal reflex; b) OCT scan OS showing marked elevation at the macular region with a hyporeflective area within the elevation.
The patient was provisionally diagnosed with CRVO and macular oedema based on history and investigations. The disease Timira (blurring of vision), a DrshtigataRoga (disease of vision) according to Ayurveda, was explored based on the symptom of blurred vision. She underwent 2 courses of inpatient treatment. The first course was for 25 days (October 4th, 2014 to October 28th, 2014), and the second course was for 14 days (January 15th, 2015 to January 28th, 2015).
Oral medicines included Guducyadi Kashaya, Sudarsanam Tablet, Amrtottaram Kashaya, Guduci Sattva, and Triphala Guggulu, Punarnavadi Kashaya, Dasamula Katutrayam Kashaya, and a Kashaya prepared from Kantakari, Tulasi, and Vasa [Table/Fig-2] were administered over the course of the treatments.
| Medicine | Preparation | Dosage | Duration |
|---|
| Guducyadi Kashaya (decoction of Tinosporacordifolia Miers., etc.,) [1] | 1 part of the ingredients are boiled in 4 parts of water and reduced to 1/4. | 15 mL with 45 mL boiled and cooled water | 04/10/2014-28/10/2014 |
| Sudarsanam Tablet (tablet prepared from the powder of Berberisaristata DC., etc.,) | The powder is prepared by mixing 1 part of each ingredient. This is then made into a tablet. | 1 tablet twice a day after food | 04/10/2014-28/10/2014 |
| BhunimbadiKashaya (decoction of Andrographispaniculata (Burm f.) Wall. [2] | 1 part of the ingredients are boiled in 4 parts of water and reduced to 1/4. | 15 mL with 45 mL boiled and cooled water | 04/10/2014-28/10/2014 |
| Amrtottaram Kashaya (decoction of Zingiberofficinale Rosc., etc.,) [3] | 2 parts of ZingiberofficinaleRosc., 6 parts of TinosporacordifoliaMiers., and 4 parts of TerminaliachebulaRetz. are added to 4 parts of water and reduced to 1/4. | 60 mL twice a day before food | 04/10/2014-28/10/2014 |
| 10 mL with 30 mL boiled and cooled water at 6 am and 6 pm (with PunarnavadiKashaya) | 15/01/2015-29/01/2015 |
| GuduciSattva (starch extract of Tinosporacordifolia Miers.) | Starch extract is prepared by soaking stems in water overnight and draining them. | 1 tablespoon at bedtime | 04/10/2014-28/10/2014 |
| Triphala Guggulu (tablets prepared from Commiphoramukul Linn., etc.,) [4] | 48 g of all ingredients taken separately are powdered and added to 240 g of purified extract of CommiphoramukulLin. This is made into a paste and rolled into pills. | 3 g twice a day after food | 04/10/2014-28/10/2014 |
| Punarnavadi Kashaya (decoction prepared from Boerrhaaviadiffusa Linn., etc., [5] | 1 part of the ingredients are boiled in 4 parts of water and reduced to 1/4. | 10 mL with 30 mL boiled and cooled water at 6 am and 6 pm (with AmrtottaramKashaya) | 15/01/2015-29/01/2015 |
| DasamulaKatutrayaKashaya (decoction of Aeglemarmelos Corr., etc.,) | 1 part of the ingredients are boiled in 4 parts of water and reduced to 1/4. | 15 ml with 45 mL boiled and cooled water at 6 am and 6 pm | 15/01/2015-29/01/2015 |
| Decoction prepared from Solanumxanthocarpum Lam., Ocimum sanctum Linn., and Adathodavasica Nees. | 1 part of the ingredients are boiled in 4 parts of water and reduced to 1/4. | 15 mL with 45 mL boiled and cooled water at 6 am and 6 pm | 15/01/2015-29/01/2015 |
External treatments comprised of Kriyakalpa (local ocular therapy), Panchakarma (purification), and therapies for the head. Virechana (therapeutic purgation), Pratimarsa Nasya (nasal medication), Tala (paste on a cotton gauze over the head), Talapoticchil (medicine on a plantain leaf over the head), Anjana (collyrium), Purampada (paste over the eyelids), Lepa (paste) over the forehead, and Pindi (poultice over the eyes) were administered during the first course of treatment. Pratimarsa Nasya, Tala, Talapoticchil, Sirolepa (paste over the head), Takradhara (irrigation of buttermilk over the head), Seka (irrigation), Anjana, and NetraPicu (cotton gauze with medicine over the closed eyes) were administered during the second course of treatment [Table/Fig-3].
| Treatment | Medicine | Method of administration | Duration |
|---|
| Seka | Kasyapam Kashaya* (decoction prepared from Terminaliachebula Retz., etc.,) | 50 mL of the decoction was poured over the closed eyes in a thin streak. | 15/01/2015 to 23/01/2015
|
| Anjana | Darsana Drops* (sterile drops prepared from Vitexnegundo Linn., etc.,) | 1 drop of the medicine was instilled from a height of 2 Angula () in both eyes. The patient was asked to gently rotate the eyes while keeping them closed. | 05/10/2014 to 06/10/2014
|
| Nalikeranjana (drops prepared from Berberisaristata D.C., etc.,) |
| Candanadi Anjana (drops prepared from Santalumalbum Linn., etc.,) | 15/01/2015 to 22/01/2015
|
| Netramrtam* (sterile drops prepared from NaCl, etc.,) |
| Tala | Kaccuradi Curna (powder prepared from) and Nimbamrtadi Eranda Taila (castor oil processed with Azadirachtaindica A. Juss, etc.,) | A paste prepared from 60 g of the powder and 300 mL of decoction was put on cotton gauze and placed over the bregma. | 06/10/2014, 20/10/2014 to 27/10/2014
|
15/01/2015 to 16/01/2015
|
| Netra Picu | Vinayakanjana* (semisolid prepared from Cynodondactylon Linn., etc.,) | A piece of cotton was dipped in 15 mL of the medicine and applied to the closed eyes. | 22/01/2015 to 29/01/2015
|
| Pratimarsa Nasya | Anutaila (oil prepared from HolostemmaadakodienSchult., etc.,) | 2 drops of oil were instilled into each nostril. | 6/10/2014, 20/10/2014, 22/10/2014 to 27/10/2014
|
16/01/2015 to 21/01/2015
|
| Purampada | MukkadiPurampada (paste prepared from TerminaliachebulaRetz., etc.,) | A paste prepared from 9 tablets of the medicine was applied over the eyelid, obviating the lashes. | 07/10/2014
|
| Talapoticchil | AdathodavasicaNees., Glychrrhyzaglabra Linn., CyperusrotundusLinn., Asparagus racemosusLinn., and EmblicaofficinalisGaertn mixed with VasaguducyadiKashaya(decoction of AdathodavasicaNees., etc.,) | A paste prepared by mixing 60 g of the powder and 300 mL of the decoction was applied on a plantain leaf, which was kept face down over the head, obviating a small circular hole in the center. | 07/10/2014 to 11/10/2014, 15/10/2014 to 17/10/2014
|
| Emblicaofficinalis Gaertn, Adathodavasica Nees., Glychrrhyzaglabra Linn., Boerrhaaviadiffusa Linn., and TerminaliachebulaRetz. mixed with Vasa Triphaladi Kashaya (decoction of Adathodavasica Nees., etc.,) | 16/01/2015 to 22/01/2015
|
| Lepa | Emblicaofficinalis Gaertn and Takra (buttermilk) | A paste prepared with 60 g of the drug and 300 mL of buttermilk was applied over the forehead. | 07/10/2014 to 11/10/2014, 15/10/2014 to 27/10/2014
|
| Sirolepa | Glychrrhyzaglabra Linn., Symplocosracemosus Roxb., Adathodavasica Nees., and Cyperusrotundus Linn. | 60 g of the powdered ingredients are made into a paste with water and applied to the forehead. | 27/01/2015 to 29/01/2015
|
| Takradhara | Vasaguducyadi Kashaya (decoction of Adathodavasica Nees., etc.,) and Emblicaofficinalis Gaertn. (for preparing the buttermilk) and decoction of EmblicaofficinalisGaertn. | 2 L of buttermilk was prepared from the 300 mL of the decoction and 60 g of the powder and was poured in a thin stream over the head. Afterwards, 1.5 L of the decoction of EmblicaofficinalisGaertn. was poured over the head. | 23/01/2015
|
| Pindi | Biophytumsensitivum | 10 g of the drug was made into a paste with SukhoshnaJala (lukewarm water) and placed on 2 pieces of Cora cloth. 2 pieces of cotton were kept over these and the cloth was folded inwards and kept over the closed eyes. | 08/10/2014 to 13/10/2014, 15/10/2014 to 27/10/2014
|
| Virechana | Avipattikara Yoga (powder prepared from Zingiberofficinale Rosc., etc.,) | 6 g of the powder was given with warm water in the morning. | 19/10/2014, 21/10/2014, 23/10/2014, 25/10/2014, 27/10/2014
|
*Patented medicines of Sreedhareeyam Ayurvedic Eye Hospital and Research Center
All medicines prescribed were procured at Sreedhareeyam’s own medicinal gardens and were manufactured at Sreedhareeyam Ayurvedic Medicines, Pvt. Ltd., the hospital’s GMP-certified manufacturing unit.
DVA assessed on 28th October 2014 (25th day of the first course) was 6/6 OD and 6/18 OS. The same reading was reported on January 28th, 2015 (14th day of the second course).
The patient was administered Guducyadi Kashaya (15 mL with 45 mL boiled and cooled water before food), Saptamrta Lauha (1 tablet twice a day after food) [6], Pathya Punarnava Curna* (1 tablespoon of powder twice a day before food), Candraprabha Vati (1 tablet twice a day after food) [7], Triphala Guggulu (1 tablet twice a day after food), and Netramrtam* (1 drop in both eyes twice a day) at discharge and was advised regular follow-ups.
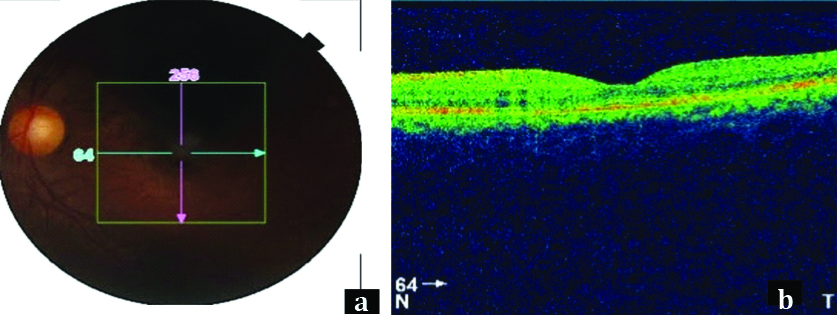
The patient reported for two subsequent follow-ups. At the first follow-up, which was on August 25th, 2016, DVA was 6/6 in both eyes (OU). The same VA was reported at the second follow-up, on January 1st, 2018. Posterior segment examination OS showed resolution of haemorrhages and cotton-wool spots, reduction in tortuosity of blood vessels, and a newly-established foveal reflex [Table/Fig-4a]. OCT showed absorption of the subretinal fluid [Table/Fig-4b].
a) Fundus photograph OS showing reduction of tortuous blood vessels, resolution of haemorrhages and cotton-wool spots, and established foveal reflex; b) OCT scan OS showing absorbed subretinal fluid, resulting in a normal appearance of the macula.
A timeline of events of the complete course of treatment is provided [Table/Fig-5].
Timeline of complete course of treatment.
| Time | Event |
|---|
| 08/2014 | Experiences a sudden onset of blurring of vision Seeks ophthalmic consultation and is diagnosed with central retinal vein occlusion and severe macular oedema Undergoes one intravitreal injection, which gives slight relief
|
| 03/10/2014 | Consults at Sreedhareeyam Hospital and is advised IP management DVA: 6/6 OD and 6/36 OS Fundus examination OS: cotton-wool spots, tortuous blood vessels, and a dull foveal reflex OCT scanning OS: elevation at the macula with a hyporeflective area within the elevation
|
| First course of treatment (04/10/2014 - 28/10/2014) |
| 04/10/2014 | Oral medicines (GuducyadiKashaya, SudarsanamTablet, BhunimbadiKashaya, AmrtottaramKashaya, GuduciSattva, and TriphalaGuggulu) are started
|
| 05/10/2014 | Anjana with DarsanaDrops* and Nalikeranjana is started
|
| 06/10/2014 | Anjana is stopped Tala with KaccuradiChurna and NimbamrtadiErandaTaila is done PratimarsaNasya with Anutailais done
|
| 07/10/2014 | Talapoticchil with Vasa, Yashtimadhu, Musta,Satavari, and Amalaki mixed with VasaguducyadiKashaya is started Lepa with Amalaki and Takrais started Purampada with MukkadiPurampadais done
|
| 08/10/2014 | Pindi with Biophytumsensitivum is started
|
| 11/10/2014 | Talapoticchil and Lepaare stopped
|
| 13/10/2014 | Pindi is stopped
|
| 15/10/2014 | Lepa, Talapoticchil, and Pindi are restarted
|
| 17/10/2014 | Talapoticchil is stopped
|
| 19/10/2014 | Virechana with Avipattikara Yoga is done
|
| 20/10/2014 | Tala and PratimarsaNasya are restarted
|
| 21/10/2014 | Virechana is done
|
| 23/05/2014 |
| 25/05/2014 |
| 27/10/2014 | Virechana, Pratimarsa Nasya, Tala, Lepa, and Pindi are stopped
|
| 28/10/2019 | Oral medicines are stopped Patient is discharged. DVA: 6/6 OD and 6/18 OS
|
| Second course of treatment (15/01/2015 - 29/01/2015) |
| 15/01/2015 | Oral medicines (Amrtottaram Kashaya, Punarnavadi Kashaya, Dasamula Katutraya Kashaya, and a decoction of Kantakari, Tulasi, and Vasa) are started Seka with Kasyapam Kashaya* is started Anjana with Candanadi Anjana and Netramrtam* is started Tala with Kaccuradi ChurnaandNimbamrtadi ErandaTaila is started
|
| 16/01/2015 | Tala is stopped Pratimarsa Nasya with Anutaila is started Talapoticchil with Amalaki, Vasa, Yashtimadhu, Punarnava, and Haritaki mixed with VasaTriphaladi Kashayais started
|
| 21/01/2015 | PratimarsaNasyais stopped
|
| 22/01/2015 | Anjanais stopped Talapoticchilis stopped NetraPicu with Vinayakanjana* is started
|
| 23/01/2015 | Seka is stopped Takradhara with VasaguducyadiKashaya and Amalaki is done
|
| 27/01/2015 | Sirolepa with Yashtimadhu, Lodhra, Vasa, and Mustais started
|
| 29/01/2015 | Sirolepa is stopped NetraPicuis stopped Oral medicines are stopped DVA: 6/6 OD and 6/18 OS
|
| 25/08/2016 | DVA: 6/6 OU
|
| 01/01/2018 | DVA: 6/6 OU Fundus examination OS: reduction in cotton-wool spots and tortuous blood vessels, and re-establishment of the foveal reflex OCT scanning OS: absorption of subretinal fluid
|
*Patented medicines of Sreedhareeyam Ayurvedic Eye Hospital and Research Center
Discussion
Vascular occlusions of the retina involve both central and branch arteries and veins. CRVO, enlisted as number 362.35 in the International Classification of Diseases, is the second most common retinal vascular pathology after diabetic retinopathy [8]. It is divided into ischaemic and non-ischaemic varieties. Its aetiology includes pressure on the vein by an atherosclerotic retinal artery, hypertension, diabetes mellitus, raised IOP, and local causes such as orbital tumours. The most common cause of defective or loss of vision in CRVO is macular oedema [9].
Its pathogenesis is believed to follow Virchow’s triad of thrombosis, which involves stasis, vascular damage, and hyper-coagulation [10]. Occlusion is believed to be caused by a thrombus at or posterior to the lamina cribrosa. Another view is that arteriosclerosis of the central retinal artery causing turbulent venous flow and endothelial damage also plays a role. Another theory states that thrombosis is an end-stage phenomenon induced by a variety of primary factors such as inflammatory optic nerve or orbital problems, structural anomalies in the lamina cribrosa, and haemodynamic changes. [11] Haematological factors such as elevated erythrocyte sedimentation rate and increased haematocrit, homocysteine, fibrinogen, and blood viscosity levels may be associated with retinal venous occlusion, but their exact role in the pathogenesis of CRVO and whether they themselves can initiate venous occlusion remains obscure.
Timira, a condition that encompasses a range of symptoms starting from Avyakta Rupa (indistinct vision) to Andhya (blindness), occurs when the pathological Doshas (humours) lodge into the Abhyantara Patalas (interior layers) of the eye. It warrants immediate and comprehensive management as Timiracan progress to Kaca (diminished vision) and finally to Linganasa (complete blindness) if left untreated [12].
Involvement of RaktaDhatu (blood) was explored as CRVO involves the blood vessels of the retina. Acakshushya Ahara and Vihara (diet and lifestyle that are detrimental to eye health) caused Pitta (bile) and Kapha (phlegm) Doshas (humors) to increase. This factor, along with the Asraya-AsrayiBhava (homologous relationship) between Pitta and Rakta, caused Rakta to pathologically increase and lodge in the eye.
In this patient, Mandagni (impaired gastric fire) and the resultant increase of the Doshas (humors) resulted in compromised delivery of vital nutrients to the eye due to Sanga (obstruction) and Vimarga Gamana (diversion of flow to improper places) of the Raktavaha Srotas (channels transporting blood).
Oedema and tortuous blood vessels were a direct result of Sanga and Vimarga Gamana, in which the retinal blood vessels became pathologically affected and leak serum into the retina. Cotton-wool spots are caused by Sanga in the fact that the inadequate supply of nutrients caused by obstruction results in hypoxia, which leads to infarction of the tissue.
The first line of management was to enhance the Jatharagni (gastric fire) by AmaPacana (digestion of toxic products) using internal medicines. This helped to clear up the obstruction in the Srotas and allow nutrition to reach both the retina and the eye as a whole. The external treatments corrected the vascular pathology in the retina and absorbed the excess subretinal fluid from the macula. Lepa (application of paste) to the forehead and Tala (application of semisolid paste) to the head facilitated vasodilation, which allowed faster absorption of toxins and resolution of oedema. An identical mode of action at the ocular level was observed with Pindi and Purampada. Takradhara facilitated absorption of the subretinal fluid and cooling down of the body.
Virechana expelled Pitta and Kapha out of the body, thus enabling absorbtion of the subretinal fluid and correction of vascular pathology. It also prevented the Doshas from moving upwards to the head. Nasya prevented excess Kapha from accumulating in the head, with Anutaila being an excellent oil for bestowing strength to the sense organs [13]. Anjana allowed penetration of minute particles that had the affinity to pass through the barriers of the eye and hence reach the target tissues.
Darsana Eye Drops is made from Nirgundi (Vitexnegundo Linn.,), SaindhavaLavana (rock salt), and Tankana (borax), and is indicated in Timira. KasyapamKvatha, prepared from Triphala (TerminaliachebulaRetz., TerminaliabellericaLinn, EmblicaofficinalisGaertn.), Vasa (AdathodavasicaNees.), Bhrngaraja (EcliptaalbaLinn.), and Candana (SantalumalbumLinn.), is useful in all eye diseases. Vinayakanjana, prepared from Durva (CynodondactylonLinn.), goat’s milk, and goat’s ghee, provides strength to the eyes and is a healing medicine. PathyaPunarnavaChurna (a powder prepared from TerminaliachebulaRetz. and BoerrhaaviadiffusaLinn.) prevents collection of fluid and permits smooth flow of nutrients to the target tissues.
The discharge medicines helped maintain Agni, prevent formation of oedema, and promote vision. In the end, the VA improved to 6/6 and was maintained through the follow-ups. This shows that the Ayurvedic protocol not only targets the disease, but also aims to bring the body back to normal activity.
Conclusion
The Ayurvedic treatment protocol for the present study patient resulted in improved DVA and retinal images both at discharge and after 2 follow-ups because of early and timely management. This case can be a stepping stone for future research in that the results may be validated by conducting large-scale sample trials.
*Patented medicines of Sreedhareeyam Ayurvedic Eye Hospital and Research Center
*Patented medicines of Sreedhareeyam Ayurvedic Eye Hospital and Research Center
[1]. Murthy KR Srikantha, AshtangaHrdaya of Vagbhata: Text, English Translation, Notes, Appendices, and Index, Vol. 1: Sutrasthana & SariraSthana 1994 VaranasiKrishnadas Academy:202 [Google Scholar]
[2]. Lochan K, Textbook of Bhaishajya Ratnavali of Govinda Dasji Bhishagratna, Chaukhambha Sanskrit Series Office 2008 Varanasi, Reprint:132 [Google Scholar]
[3]. Nishteswar K, Vidyanath R, Sahasrayogam: A Popular Book on Keraliya Tradition of Ayurvedic Treatment, Chowkhamba Sanskrit Series Office 2014 Varanasi, Reprint:4 [Google Scholar]
[4]. Murthy KR, Srikantha, SarngadharaSamhita: Text, English Translation, Notes, Appendices, and Index, ChaukhambhaOrientalia 2004 4th EditionVaranasi:109 [Google Scholar]
[5]. Murthy KR, Srikantha, SarngadharaSamhita: Text, English Translation, Notes, Appendices, and Index, ChaukhambhaOrientalia 2004 4th EditionVaranasi:70 [Google Scholar]
[6]. Sharma PV, Cakradatta: Sanskrit Text with English Translation, ChaukhambhaOrientalia 2000 Varanasi:251 [Google Scholar]
[7]. Murthy KR, Srikantha, SarngadharaSamhita: Text, English Translation, Notes, Appendices, and Index, ChaukhambhaOrientalia 2004 4th EditionVaranasi:105 [Google Scholar]
[8]. Hayreh SS, Zimmerman MB, Podhajasky P, Incidence of various types of retinal vein occlusion and their recurrence and demographic characteristicsAm J O Ophthalmol 1994 11721:429-41.10.1016/S0002-9394(14)70001-7 [Google Scholar] [CrossRef]
[9]. Yanoff M, Duker J, Ophthalmology: 3rd Edition 2009 Philadelphia, PennsylvaniaMosby, an Imprint of Elsevier, Inc.:599 [Google Scholar]
[10]. Pichi F, Linn JI, Tripathy K, Shah VA, Central Retinal Vein Occlusion, American Academy of Ophthalmologyhttps://eyewiki.aao.org/Central_Retinal_Vein_Occlusion [Google Scholar]
[11]. Yanoff M, Duker J, Ophthalmology: 3rd Edition 2009 Philadelphia, PennsylvaniaMosby, an Imprint of Elsevier, Inc.:597 [Google Scholar]
[12]. Murthy KR, Srikantha, AshtangaHrdaya of Vagbhata: Text, English Translation, Notes, Appendices, and Index, Vol. 3: UttaraSthana 1994 VaranasiKrishnadas Academy:113 [Google Scholar]
[13]. Sharma RK, Dash B, CarakaSamhita: Text with English Translation and Critical Exposition based on CakrapaniDatta’s Ayurveda Dipika, Vol 1: Sutra Sthana:121 [Google Scholar]