Case Report
A 62-year-old male from Hanumangarh district presented to the Cardiothoracic Vascular Surgery (CTVS) OPD with the complaints of a non healing wound since two months on the anterior aspect of the chest along with pain in the surrounding area. On physical examination, he was afebrile with a pulse rate of 76 beats/min, Resp Rate 14/min, BP122/86 mmHg. The ulcer/wound was 2*3 cm in size, round in shape, with punched out edges, entire margins, associated with red granulation tissue at the base with purulent discharge. The patient was a known diabetic. Random blood sugar was 72.6 mg and Glycosylated Haemoglobin (HbA1C) was 8 mmol/L. A provisional clinical diagnosis of an infective ulcer was made and differential diagnosis of tubercular or malignant was kept in mind. A pus culture was planned first to confirm the infective etiology. Other investigations were planned later.
On further evaluation it was found that the patient had a Coronary Artery Bypass Grafting (CABG) surgery in Jaipur two months back. Around 7-10 days following the surgery he developed this lesion which did not respond to the drugs given. The information about the drugs given or any investigation done could not be elicited as patient did not have any documents. A pus swab was collected from the wound and transferred to the microbiology laboratory immediately. The swab was inoculated on Blood agar, MacConkey agar and Nutrient Agar. The plates were incubated overnight at 37°C in aerobic conditions. A gram stain was prepared from the swab which revealed numerous pus cells and gram negative bacilli. After 24 hours of incubation, the agar plates revealed purple coloured colonies which were 2-3 mm in size [Table/Fig-1] and showed β haemolysis on blood agar. The organism was Gram negative bacilli, catalase positive, oxidase positive, motile. TSI showed K/A reaction without gas with H2S. citrate was utilised, MR negative, Indole negative. We suspected the organism to be Chromobacterium violaceum. The organism was further tested by Vitek 2 compact (Biomerieux, France) for confirmation of identifiction and for testing antibiotic susceptibility. The results were interpreted as per the Clinical and Laboratory Standards Institute (CLSI) guidelines 2019 for other non-Enterobacteriaceae. The organism was found to be sensitive to ciprofloxacin (MIC 1), meropenem (MIC 4) and trimethoprim-sulphamethoxazole (MIC <20) and resistant to ampicillin (MIC >32), amoxicillin-clavulanic acid (MIC>32), ceftriaxone (MIC>64), cefepime (MIC >32), cefuroxime (MIC >64), imipenem (MIC>16), amikacin (MIC >64), gentamycin (MIC >16), piperacillin-tazobactam (MIC>128), colistin (MIC >16).
Colonies of C. violaceum on macConkey agar and nutrient agar showing violet pigmentation.

Ciprofloxacin 500 mg was started 12 hourly and patient started improving by Day 4. There was reduction in pain and the size of the wound. Cotrimoxazole was added along with ciprofloxacin on day 5. The patient was last seen two months after the incidence without any complication.
Discussion
Infective aetiology was the provisional diagnosis in this case and pus culture revealed the presence of Chromobacterium violaceum. Tubercular or malignant ulcer was the next differentials to be evaluated, had infective aetiology was ruled out. The plan was to treat the infection first and as the patient improved on Ciprofloxacin, the chances of other differentials were ruled out. The patient did not have any systemic features so, the treating physician did not ask for blood culture as the patient started improving with ciprofloxacin administration, so the second sample for confirmation was not taken.
Chromobacterium violaceum is a motile facultatively anaerobic Gram-negative bacillus, found in the water and soil of tropical areas [1-5]. Taxonomically, it is included in class-Betaproteobacteria, order-Neisseriales, family-Neisseriaceae, Genus-Chromobacterium, species-violaceum [6]. Its striking features are its ability to progress to fatal sepsis with metastatic abscesses as well as its multidrug resistance [7].
It is catalase and oxidase positive, grows easily on ordinary media like blood agar, MacConkey agar, and nutrient agar and usually produces a characteristic antioxidant non diffusible pigment called violacein that gives the bacterial colonies purple color on agar [1,2,7,8].
The organism was first identified in 1881. The pathogenic potential was established in 1905, by Wooley, who isolated the organism from a fatal infection in buffalo [3]. The first case of human infection was reported from Malaysia in 1927 [2,6].
It is a rare human pathogen. Humans acquire infection through exposure of wound or traumatic skin lesion to contaminated soil or water. Humans can also acquire infection through urinary tract or by some medical equipment in the hospital [1,6].
Its clinical spectrum varies from a localised skin lesion, urinary tract infection, gastrointestinal infection, osteomyelitis, conjunctivitis, diarrhea, meningitis, brain abscess, endocarditis, pneumonia to severe sepsis. If not treated, the disease rapidly progresses to septic shock with multi organ failure [3,8]. C. violaceum is usually resistant to penicillin, narrow-spectrum cephalosporin, amoxicillin-clavulanic acid, and polymyxin B but sensitive to fluoroquinolones, carbapenems, cotrimoxazole, chloramphenicol, cefepime, aminoglycosides, amikacin, imipenem, piperacillin-tazobactam, gentamycin, tetracycline, and trimethoprim-sulfamethoxazole [2,5,9].
The organism is usually isolated from skin lesions and blood. It can be easily identified on the basis of biochemical tests. However, a high index of suspicion is required for diagnosis [7].
So far, 21 cases have been reported from India. Out of these 21 cases, 13 were paediatric cases and 8 adult, with 2 of them being elderly >60 years, 2 neonates and 3 infants. A review of the literature is described in [Table/Fig-2] [2-7,9-15]. To the best of our knowledge, this is the first adult case being reported from North India. Earlier published cases have reported a high mortality rate of >50% [1,5,6], however, a recent case series of 28 patients from the Northern Territory of Australia published a mortality rate of 7.1% [1]. The result of the cases reviewed show an overall mortality to be 36.3% (11.1% in adults and 53.8% in paediatrics) in India. Khadanga S et al., reported the mortality among 13 Indian cases to be around 80% [6]. The reduction in mortality rate can be explained by better diagnosis and improved antibiotic administration.
Cases of C. violaceum reported from India [2-7,9-15].
| S. No. | Year | Age/Sex | Location | Complaints | Sample | Treatment | Outcome | Reference No. |
|---|
| 1 | 1979 | 4 y/M | Vishakhapatnam, Andhra Pradesh | Fever, septicaemia, meningitis, ulcers | Blood, Skin lesion | Gentamycin, Kanamycin, | Died | [9] |
| 2 | 1987 | NB | Manipal, Karnataka | Fever, meningitis | CSF | Gentamycin, Cotrimoxazole | Died | [9] |
| 3 | 2000 | 2 y/F | Manipal, Karnataka | Diarrhoea | Stool | Gentamycin, Ampicillin | Recovered | [9] |
| 4 | 2002 | 2 m/F | Manipal, Karnataka | Pustules, ear discharge | Blood, liver pus, Sinus discharge | Gentamycin, Ceftazidime, amoxicillin-clavulanic acid | Died | [9] |
| 5 | 2002 | 8 d/ | Mangalore, Karnataka | Fever, ear discharge, multiple abscess | Blood, Skin, | Gentamycin, Cefotaxime, Ceftriaxone | Died | [9] |
| 6 | 2003 | 24y/M | Beliaghata, Kolkata | Wound abscess on right leg | Pus | Ciprofloxacin | Recovered | [12] |
| 7 | 2004 | 6.5 y/M | Chandigarh | High fever, rapid breathing, pustule over right upper back | Blood, Pus | Ciprofloxacin, Amikacin | Recovered | [9] |
| 8 | 2006 | NA/F | Orissa | Puerperal sepsis | NA | Amikacin, Gatifloxacin | Recovered | [13] |
| 9 | 2009 | 6 m/M | Calicut, Kerala | Fever, breathing difficulty, multiple skin lesions, cough, loose stools | Blood, bone marrow aspirate | Piperacillin, Ciprofloxacin | Recovered | [10] |
| 10 | 2011 | 35y/M | Manipal | High grade fever, perineal pain, burning micturition, prostatitis | Urine | Ciprofloxacin | Recovered | [14] |
| 11 | 2012 | 40y/M | Vellore | High grade fever, pain and swelling in right knee | Blood, synovial fluid | Piperacillin-tazobactam, Meropenem | Died | [3] |
| 12 | 2012 | 42y/M | Tamil Nadu | Wound in scalp | Pus | Gentamycin | Recovered | [2] |
| 13 | 2014 | 19y/M | Bhubaneshwar, Odisha | Fever with chills, pain lower abdomen | Urine | Ciprofloxacin | Recovered | [9] |
| 14 | 2015 | 53/F | Mangalore, Karnataka | Fever, abdominal pain, vomiting, abscess left leg | Blood, Pus | Ciprofloxacin, Imipenem | Recovered | [4] |
| 15 | 2015 | 11 y/F | Mumbai, Maharashtra | Fever, pain on right foot | Blood, skin scrappings | Piperacillin-tazobactam, Gentamycin, Ciprofloxacin | Recovered | [5] |
| 16 | 2016 | 2.5 y/M | Kozhikode, Kerala | Fever, swelling over scalp | Blood | Ampicillin, Cloxacillin | Died | [7] |
| 17 | 2016 | 12 y/F | Kozhikode, Kerala | Dysuria, fever with chills | Urine | Ciprofloxacin | Recovered | [7] |
| 18 | 2016 | 11 m/M | Kozhikode, Kerala | High fever, loose stools, cellulitis on right cheek, lymphadenopathy | Blood | Cefotaxime, Ampicillin, Vancomycin | Died | [7] |
| 19 | 2017 | 4.5 y/F | Thootukudi | Fever, respiratory distress, abdominal pain | Blood | NA | Died | [11] |
| 20 | 2017 | 2 y/M | Bhopal, Madhya Pradesh | Fever, ulcer on right chest | Blood | Meropenem | Recovered | [15] |
| 21 | 2017, | 62y/M | Balasore, Odisha | Ulcer on left foot | Pus | Ciprofloxacin | Recovered | [6] |
| 22 | 2019 | 62y/M | Sriganganagar, Rajasthan | Wound on chest | Pus | Ciprofloxacin | Recovered | Present case |
There was rapid progression of the disease in the paediatric population. The fatality was noted to be more in patients presenting with septicaemia, meningitis or multiple abscesses. This observation was similar in other studies [5,9]. However, it was observed that whenever the antibiotics were changed on time, the progression of the disease was halted and the chances of recovery of the patient were improved.
Limited literature is available on the antimicrobial susceptibility of the organism. Ciprofloxacin is the most effective antibiotic in vitro, in almost all the cases reported [7,8,10,11]. The organism may also be sensitive to aminoglycosides, carbapenems and piperacillin-tazobactam. Most strains are resistant to penicillins and cephalosporins [2,5,7,9].
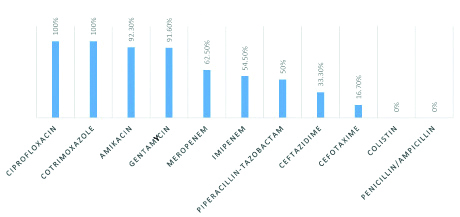
The antibiotic susceptibility pattern of the isolates obtained so far in India has been described in [Table/Fig-3]. The isolates demonstrate 100% susceptibility to ciprofloxacin and cotrimoxazole, followed by aminoglycosides, carbapenems, piperacillin-tazobactam. The isolates have demonstrated complete resistance to colistin and penicillin/ampicillin. The isolate in the present case was sensitive to ciprofloxacin, cotrimoxazole, meropenem and resistant to aminoglycosides, imipenem, penicillin, cephalosporins and piperacillin-tazobactam.
Antibiotic susceptibility pattern of C. violaceum isolates from India.
Conclusion
C. violaceum is a rare human pathogen, but increasing incidence suggests that a high clinical suspicion, prompt diagnosis and active intervention are imperative to effectively manage this otherwise fatal organism, especially in cases with signs of sepsis. Ciprofloxacin is the most effective antibiotic available so far, hence as soon as the isolation of the organism is suspected; the management should be changed accordingly to control the progression of this emerging life threatening infection.
[1]. Meher-Homji Z, Mangalore RP, Johnson PDR, Chua KYL, Chromobacterium violaceum infection in chronic granulomatous disease: A case report and review of the literatureJMM Case Rep 2017 4:01-05.10.1099/jmmcr.0.00508428348801 [Google Scholar] [CrossRef] [PubMed]
[2]. Kumar MR, Chromobacterium violaceum: A rare bacterium isolated from a wound over the scalpInt J Appl Basic Med Res 2012 2:70-72.10.4103/2229-516X.9681423776815 [Google Scholar] [CrossRef] [PubMed]
[3]. Karthik R, Pancharatnam P, Balaji V, Fatal Chromobacterium violaceum septicaemia in a South Indian adultJ Infect Dev Ctries 2012 6:751-55.10.3855/jidc.186623103899 [Google Scholar] [CrossRef] [PubMed]
[4]. Madi DR, Vidyalakshmi K, Ramapuram J, Shetty AK, Successful treatment of Chromobacterium violaceum sepsis in a south Indian adultAm J Trop Med Hyg 2015 93:1066-67.10.4269/ajtmh.15-022626304923 [Google Scholar] [CrossRef] [PubMed]
[5]. Saboo AR, Vijaykumar R, Save SU, Bavdekar SB, A rare nonfatal presentation of disseminated Chromobacterium violaceum sepsisJ Microbiol Immunol Infect 2015 48:574-77.10.1016/j.jmii.2012.11.002 [Google Scholar] [CrossRef]
[6]. Khadanga S, Karuna T, Dugar D, Satapathy SP, Chromobacterium violaceum induced sepsis and multiorgan dysfunction, resembling melioidosis in an elderly diabetic patient: A case report with review of literatureJ Lab Physicians 2017 9:325-28.10.4103/JLP.JLP_21_1728966500 [Google Scholar] [CrossRef] [PubMed]
[7]. Kaniyarakkal V, Orvankundil S, Lalitha SK, Thazhethekandi R, Thottathil J, Chromobacterium violaceum septicaemia and urinary tract infection: Case reports from a tertiary care hospital in south IndiaCase Rep Infect Dis 2016 22:01-04.10.1155/2016/679574327747113 [Google Scholar] [CrossRef] [PubMed]
[8]. Swain B, Otta S, Sahu KK, Panda K, Rout S, Urinary tract infection by Chromobacterium violaceumJ Clin Diagn Res 2014 8:DD01-DD02.10.7860/JCDR/2014/9230.470325302195 [Google Scholar] [CrossRef] [PubMed]
[9]. Ray P, Sharma J, Marak RS, Singhi S, Taneja N, Garg RK, Sharma M, Chromobacterium violaceum septicaemia from north IndiaIndian J Med Res 2004 120:523-26. [Google Scholar]
[10]. Vijayan AP, Anand MR, Remesh P, Chromobacterium violaceum sepsis in an infantIndian Paediatr 2009 46:721-22. [Google Scholar]
[11]. Subitha B, Jeyamurugan T, Gomatheswari SN, Hariprasad G, Rare cause of sepsis - Chromobacterium violaceum a case reportInt J Curr Microbiol App Sci 2017 6:1772-75.10.20546/ijcmas.2017.605.192 [Google Scholar] [CrossRef]
[12]. Dutta S, Dutta SK, Multidrug resistant Chromobacterium violaceum: An unusual bacterium causing long standing wound abscessIndian J Med Microbiol 2003 21:217-18. [Google Scholar]
[13]. Mahapatra A, Roy D, Poddar N, Panda R, Sarangi G, Mallick B, Chayani N, Chromobacterium violaceum: A case report of an unusual bacterium causing puerperal sepsisIndian J Pathol Microbiol 2006 49:450-52. [Google Scholar]
[14]. Shobha KL, Bairy I, Prostatitis by Chromobacterium violaceum- A case reportInt J Med Public Health 2011 1:54-55.10.5530/ijmedph.4.2011.12 [Google Scholar] [CrossRef]
[15]. Ahmed M, Aapte AA, Shukla V, Sarkar D, Shankar H, Chromobacterium violaceum bacteremia in a 2 years old male childPaediatric Oncall Journal 2017 14:43-44.10.7199/ped.oncall.2017.17 [Google Scholar] [CrossRef]