Tuberculous Meningitis Presenting with Sudden Deterioration and Demise after Ceftriaxone Withdrawal: A Case Report and Review of Literature
Francis Ikechukwu Ukekwe1, Ann Ebele Aronu2, Isaiah Ogbonna Nwidenyi3, Ngozi Chinyelu Ojinnaka4
1 Senior Lecturer/Consultant Pathologist, Department of Morbid Anatomy, University of Nigeria, Enugu Campus, Enugu/University of Nigeria Teaching Hospital, Ituku-Ozalla, Enugu, Nigeria.
2 Senior Lecturer/Consultant Paediatrician, Department of Paediatrics, University of Nigeria, Enugu Campus, Enugu/University of Nigeria Teaching Hospital, Ituku-Ozalla, Enugu, Nigeria.
3 Senior Registrar, Department of Morbid Anatomy, University of Nigeria Teaching Hospital, Ituku-Ozalla, Enugu, Nigeria.
4 Professor/Consultant Paediatrician, Department of Paediatrics, University of Nigeria, Enugu Campus, Enugu/University of Nigeria Teaching Hospital, Ituku-Ozalla, Enugu, Nigeria.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Francis Ikechukwu Ukekwe, Department of Morbid Anatomy, University of Nigeria, Enugu Campus (UNEC), P. M. B. 01129, Enugu-400241, Ituku-Ozalla, Enugu State, Nigeria.
E-mail: drikukekwe@hotmail.com
Tuberculous Meningitis (TBM) is a challenging condition to diagnose due to its non-specific clinical presentation and the limited sensitivity of existing laboratory techniques. Here we report an unusual presentation of TBM in a Nigerian teenager who presented with fever, headache, neck stiffness and progressive weight loss, and who had remarkable improvement while on ceftriaxone but had sudden deterioration and demise on withdrawal of ceftriaxone. Postmortem findings of TBM underlie the need for a high index of suspicion to enable early diagnosis, proper treatment and better prognosis.
Autopsy, Diagnosis, Tuberculosis
Case Report
A 13-year-old female teenager presented at the Paediatric Neurology Unit through the Children Outpatient Clinic with a three-month history of high grade fever, associated with headache, which was throbbing in nature and located at the frontal region. There was also associated progressive weight loss for two months and neck stiffness for two weeks. There was no cough or history of household contact with sputum smear-positive tuberculosis. She had been admitted into three different peripheral hospitals and had been placed on various intravenous antibiotics, with no clinical improvement. She had no remarkable medical history and was fully immunised.
Physical examination on admission revealed a fully conscious but ill-looking teenager with a temperature of 38.2°C. Central nervous system examination revealed only signs of meningeal irritation and uvula deviation to the right. Other aspects of physical examination were normal.
Laboratory investigations showed an elevated erythrocyte sedimentation rate, CSF White Blood Cell (WBC) count of 500 cells/mm3, normal Cerebrospinal Fluid (CSF) sugar but raised protein 0.76 gm/l (0.15-0.40 gm/l). MRI showed features suggesting obstruction of the flow of CSF at the region of aqueduct of sylvius.
Patient was managed for poorly treated meningitis with ceftriaxone and she became afebrile by the 2nd day of admission. There was remarkable improvement with CSF WBC count of 3-4 cells/mm3 and antibiotic was discontinued on the 12th day. There was a relapsed of symptoms two days later and TBM was considered. An urgent CT scan was requested and samples were taken for Full Blood Count (FBC) and CSF analysis but the patient however had a protracted seizure same night, lapsed into unconsciousness and died 2 hours later.
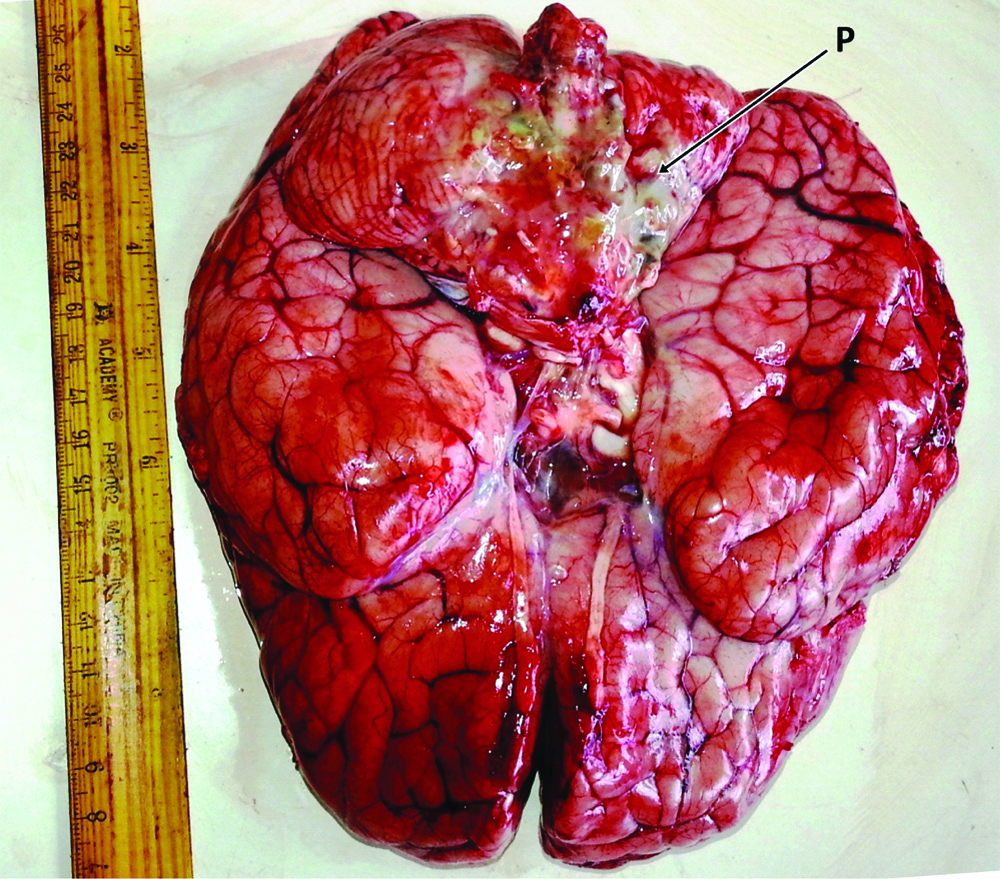
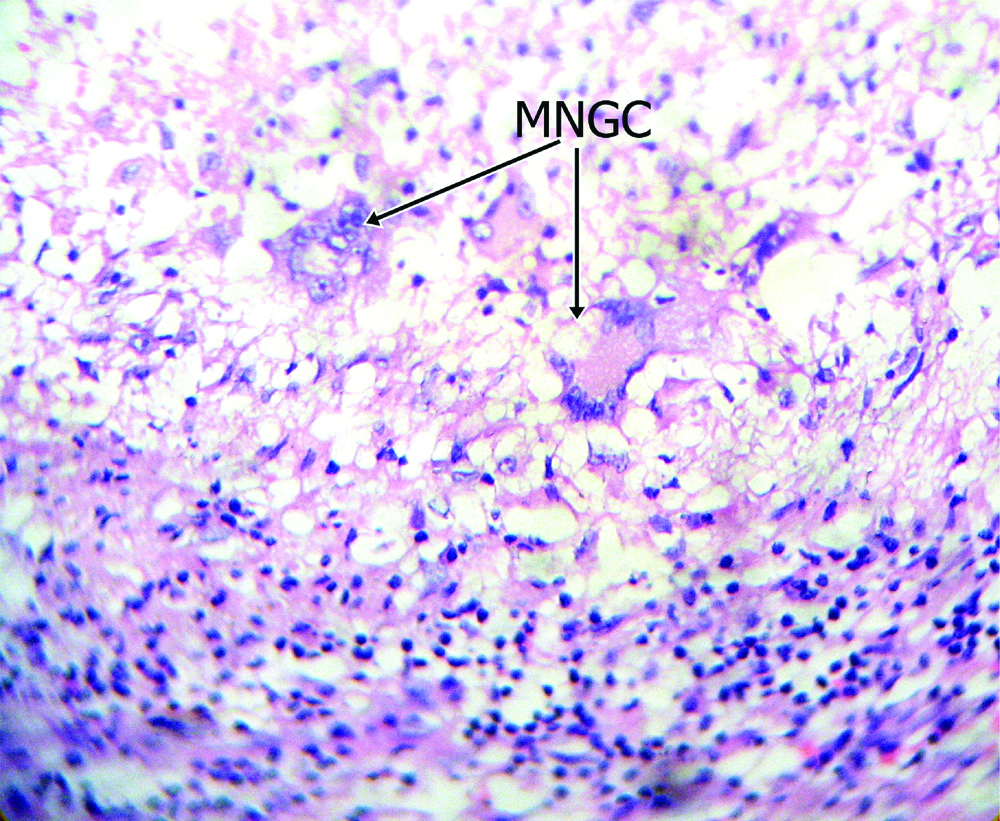
An autopsy was requested because of the unusual presentation of sudden deterioration and demise following improvement on treatment. Postmortem examination however showed remarkable thick pussy exudate at the base of a severely oedematous brain [Table/Fig-1] and on microscopic examination of brain sections, several foci of poorly formed tuberculous granulomas with Langhan’s type Multinucleate Giant Cells (MNGC), lymphoplasmacytic cells and macrophages were seen [Table/Fig-2].
Photograph of the brain at postmortem examination showing remarkable pussy exudate (P) at the base of a severely oedematous brain.
Photomicrograph of the brain section showing foci of poor tuberculous granuloma formation with Langhan’s type Multinucleate Giant Cells (MNGC) (H&E, x400).
Discussion
The scourge of Tuberculosis (TB) continues to have global dimensions as one of the world’s deadliest communicable diseases presenting as clinical affectations of different parts of the body [1]. TBM is a rare form of extrapulmonary tuberculosis [2] comprising 2-5% of all active cases of Mycobacterium tuberculosis (MTB) [3] and accounting for about 7.8% to 14% of all cases of TB in Nigeria [2-4]. It also accounts for a significant proportion of TB cases globally, causing substantial morbidity and mortality, especially in children and HIV-infected patients [5,6]. It is an infection that is caused by the hematogenous dissemination of tuberculosis bacilli from its primary focus [7] and a challenging condition to diagnose due to its non-specific clinical presentation and the limited sensitivity of existing laboratory techniques [5].
TBM is also the most severe form of Mycobacterium tuberculosis infection, causing death or disability in more than half of those affected [8]. It is a highly devastating form of tuberculosis, which, even in the setting of appropriate anti-tuberculous therapy, leads to unacceptable levels of morbidity and mortality [5,9]. Patients with TBM usually develop typical symptoms and signs of meningitis such as headache, fever, and stiff neck which may be absent in the early stages but can present from several days to several months [10]. This is similar to the index patient who presented with a three-month history of high grade fever, associated frontal throbbing headache, neck stiffness and progressively weight loss. She also had no associated history of cough or household contact with sputum smear-positive tuberculosis. Though she had received various intravenous antibiotics while on admission at a peripheral hospital with no clinical improvement, findings from an initial CNS examination, laboratory investigations and Magnetic Resonance Imaging (MRI) suggested poorly treated meningitis with obstruction of the flow of CSF at the region of aqueduct of sylvius. Though neuro imaging of the CNS can help to strengthen diagnosis and to monitor disease progression in TBM, especially in developing countries where definite diagnosis by laboratory testing is limited, it is however not definitive in confirming TBM [9,11]. She however, made remarkable improvements while receiving appropriate dose of ceftriaxone. This necessitated the decision to discontinue the antibiotics treatment which resulted in her unusual sudden deterioration and demise. The non-specificity of these clinical presentations and the limited sensitivity of existing laboratory techniques and the unavailability of promising molecular diagnostic techniques in most developing countries like ours, and reliance on largely insensitive microbiological methods make diagnosis and treatment of CNS tuberculosis a formidable diagnostic challenge [5,9,10]. Thus CNS tuberculosis rely largely on microbiological methods that are insensitive, despite the development of promising molecular diagnostic techniques which are unavailable in most developing countries like ours [5,9]. The autopsy findings of thick pussy exudate at the base of a severely oedematous brain [Table/Fig-1] and foci of poor tuberculous granuloma formation with Langhan’s type MNGC, lymphoplasmacytic cells and macrophages [Table/Fig-2] were diagnostic of TBM [4], a highly devastating form of tuberculosis, which, even in the setting of appropriate anti-tubercular therapy, leads to unacceptable levels of morbidity and mortality [5,9]. Early identification of TB in the paediatric population at risk of TBM especially when the patient lives in TB endemic regions of Southeast Asia, Western Pacific and Africa improves the prognosis [12-14]. The probable source of infection in the index case could be due to droplet inhalation from a coughing close contact. Since, she was living with her grandmother in poor conditions in a resource limited area of South East Nigeria but this contact could not be traced before her demise.
The incidence of multidrug-resistant strains of M. tuberculosis is rising so there is an increasing need of well-tolerated and effective antibiotics [5]. A high index of suspicion is thus required by the attending clinician to enable early diagnosis if the patient is to survive, because a missed or delayed diagnosis is commonly fatal [10,15]. The index patient died despite an initial improvement because of a missed diagnosis, thus highlighting the need for the attending clinician to always consider TBM early enough in all cases of suspected meningitis irrespective of the presenting clinical signs and symptoms.
Conclusion
This report underscores TBM as a diagnostic challenge in children that could lead to substantial morbidity and mortality if not promptly diagnosed and properly managed. High index of suspicion, early diagnosis and appropriate treatment modalities are required for a favorable prognosis.
Financial or Other Competing Interests
None.
Patient consent was obtained before publication of this work.
[1]. Ukekwe FI, Olusina DB, Banjo A, Akinde OR, Nzegwu MA, Okafor OC, Tuberculous lymphadenitis in south-eastern Nigeria: A 15 years histopathologic review (2000-2014)Ann Med Health Sci Res 2016 6(1):44-49.10.4103/2141-9248.18027327144076 [Google Scholar] [CrossRef] [PubMed]
[2]. DOTS Expansion Plan to Stop TB in the WHO European Region 2002-2006. World Health Organization. Regional Office for Europe 2002 [Google Scholar]
[3]. Fischbein N, Dillon W, Barkovich A, TuberculosisIn: Teaching atlas of brain imaging 2000 Thieme:165-68. [Google Scholar]
[4]. Komolafe MA, Sunmonu TA, Esan OA, Tuberculous meningitis presenting with unusual clinical features in Nigerians: Two case reportsCases J 2008 1(1):18010.1186/1757-1626-1-18018816394 [Google Scholar] [CrossRef] [PubMed]
[5]. Ho J, Marais BJ, Gilbert GL, Ralph AP, Diagnosing tuberculous meningitis- have we made any progress?Tropical Medicine and International Health 2013 18(6):783-93.10.1111/tmi.1209923521060 [Google Scholar] [CrossRef] [PubMed]
[6]. Marais S, Pepper DJ, Schutz C, Wilkinson RJ, Meintjes G, Presentation and outcome of tuberculous meningitis in a high HIV prevalence settingPLoS ONE 2011 6(5):e20077doi: 10.1371/journal.pone.002007710.1371/journal.pone.002007721625509 [Google Scholar] [CrossRef] [PubMed]
[7]. Elmas ON, Akıncı A, Bilir P, Tuberculous meningitis associated with diabetic ketoacidosisJ Clin Res Pediatr Endocrinol 2011 3(4):222-24.10.4274/jcrpe.37322155468 [Google Scholar] [CrossRef] [PubMed]
[8]. Török ME, Tuberculous meningitis: Advances in diagnosis and treatmentBr Med Bull 2015 113(1):117-31.10.1093/bmb/ldv00325693576 [Google Scholar] [CrossRef] [PubMed]
[9]. Marx GE, Chan ED, Tuberculous meningitis: Diagnosis and treatment overviewTuberc Res Treat 2011 2011:79876410.1155/2011/79876422567269 [Google Scholar] [CrossRef] [PubMed]
[10]. Chin JH, Tuberculous meningitis: Diagnostic and therapeutic challengesNeurol Clin Pract 2014 4(3):199-205.10.1212/CPJ.000000000000002325110618 [Google Scholar] [CrossRef] [PubMed]
[11]. Rim A, Fakher K, Badreddine K, Hanène T, Faycal Z, Ahmed G, Tuberculous meningitis in adults: MRI contribution to the diagnosis in 29 patientsInternational Journal of Infectious Diseases 2006 10(5):372-77.10.1016/j.ijid.2005.07.00916839793 [Google Scholar] [CrossRef] [PubMed]
[12]. World Health Organization. Global tuberculosis report 2013. Available at: http://www.who.int/tb/publications/global_report/en/index.html. Accessed January 10, 2014 [Google Scholar]
[13]. Guziejko K, Czupryna P, Moniuszko A, Grygorczuk S, Kondrusik M, Zajkowska J, Tuberculous meningitis-A case reportPrzegl Epidemiol 2013 67(4):629-32.:717-19. [Google Scholar]
[14]. Chow EJ, Toll E, Montague BT, Alexander-Scott N, Van Scoyoc E, Tuberculous meningitis in child born in the US to immigrants from a tuberculosis-endemic countryR I Med J (2013) 2014 98(1):22-25. [Google Scholar]
[15]. Khanna SR, Kralovic SM, Prakash R, Tuberculous meningitis in an immunocompetent host: A case reportAm J Case Rep 2016 17:977-81.10.12659/AJCR.90076228008165 [Google Scholar] [CrossRef] [PubMed]