Imaging of Breast Hamartoma on Mammography, Ultrasound and MRI
Pratiksha Yadav1
1 Professor, Department of Radiology, Dr. D.Y. Patil Medical College, Hospital and Research Centre, DPU, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pratiksha Yadav, Department of Radiology, Dr. D. Y. Patil Medical College, Sant Tukaram Nagar, Pimpri, Pune, Maharashtra, India.
E-mail: yadavpratiksha@hotmail.com
Hamartoma or fibroadenolipomas are rare benign tumours. These tumours present as painless, mobile masses or it can be asymptomatic and detected incidentally on screening mammogram. This article intends to review the characteristic findings of breast hamartoma on mammography, tomosynthesis, ultrasound and Magnetic Resonance Imaging (MRI) techniques. Multiparametric MRI is a sensitive non invasive modality for diagnosis of these masses. There is a need to evaluate the characteristic imaging features of hamartoma in order to make an accurate diagnosis. Most of the patients with breast hamartomas are young patients so we can avoid the radiation based imaging techniques. MRI can be used in the uncertain cases of hamartoma on mammography and ultrasound. Advanced MRI techniques e.g., Diffusion Weighted Imaging (DWI) with mean ADC calculation and MR Sepctroscopy (MRS) are useful non-invasive techniques which can be used for effective diagnosis and can avoid biopsy in these patients. Pathologically, a distinctive appearance lacks in these masses as these consists of lactiferous tissue, fat and fibrous tissue. Clinical finding of breast lump or breast asymmetry and imaging features are helpful in the diagnosis.
Adenolipoma, Benign, Diffusion weighted imaging, Fibroadenolipoma, Lipofibroadenoma
Introduction
Breast hamartomas are the benign neoplasm with incidence of 0.1-0.7% in all benign breast masses [1]. Increased social awareness and use of various imaging techniques to evaluate breast lump with mammography, ultrasound and MRI, it is expected to report more cases of hamartomas. It is also known as fibroadenolipomas, lipofibroadenomas or adenolipomas depending upon the amount of fat, glandular tissue and fibrous elements in the mass which is surrounded by the pseudocapsule [2]. Arrigoni MG et al., first used the term hamartoma in 1971 [3]. These are painless, mobile masses which are typically present in the middle age women during 4th or 5th decade of life [1,4]. It may not be palpable and is sometimes detected incidentally during screening work up. These tumours grow and develop a larger masses in many cases and sometimes present with enlargement of the breast [5].
Most of the articles correlating to breast hamartoma found in the literature are presented as case reports and rarely as case series [5-8]. This review article discusses the characteristic findings of breast hamartoma on mammography, ultrasound and MRI. It gives the information about the diffusion weighted MRI and MR Spectroscopy findings in these lesions.
Although, it was stated in the text book that the hamartomas are rare tumour but those radiologists who use both mammography and ultrasound for screening; frequently encounter these tumours. Aetiopathology of breast hamartoma is not clear but they are thought to result from dysgenesis than a true tumorous process [4]. These masses consists of mammary glands, lactiferous tissue, connective tissue and fat, which are surrounded by pseudocapsule. Fechner RE et al., described the lobular distribution and presence of fat is the distinguishing features as compared to fibroadenomas [9].
Hamartoma may cause enlargement of the breast. It has all the constituents of normal breast tissue so histologically, it may not have recognised but on radiological investigations it showed typical features. Clinical, radiological and pathological correlation is always important for the correct diagnosis. MRI is an excellent modality to demonstrate the content of the hamartoma.
Malignant transformation of hamartomas is very rare but it can occur in the mass which contains the epithelial tissue. A review of the literature described 15 cases of carcinoma associated with Hamartoma [1,6]. It is important to recognise the suspicious findings on mammography, Ultrasound and MRI that may be present in the hamartoma.
Hamartoma can give variable appearance on mammography and ultrasonography as it contains variable amount of fat and fibrous tissues [7,8]. On conventional T1WI and T2WI these lesions reveal heterogeneous signal intensities due to the fatty and fibroglandular tissue and thin hypointense capsule [10]. Advanced MRI provide additional information which can help in the diagnosis. On DWI these lesions does not show restriction and mean ADC values similar to normal breast parenchyma [10,11].
Imaging Techniques
Mammography was done on Mammomat Inspiration Siemens Healthineers. Standard Medial Oblique (MLO) and Craniocaudal (CC) views of both the breasts were taken. In dense breast tomosynthesis were also done. Ultrasound Breast was done on Hitachi Aloka Areittas S 60 colour doppler ultrasound machine using high frequency linear transducer. MRI was done on 1.5 T Seimen’s Avanto and 3T Seimen’s Vida machine using dedicated breast coil. Patient was positioned prone. Field of view (FOV) 300-360 mm were used and slice thickness 3 mm was selected. T1WI, T2WI and STIR in axial plane, STIR, T2WI coronal, T2WI and STIR in sagittal plane images were acquired. DWI were obtained using diffusion weighted echo-planer imaging, sensitising diffusion gradients with b value of 0,400 and 800 s/mm2. Mean ADC measurements were obtained using circular Region Of Interest (ROI) placed in the lesion. All the measurements were performed three times and the average were used in the final calculation. Dynamic contrast enhanced MRI was performed. Pre contrast fat-suppressed T1WI axial images were obtained before injection intravenous contrast media. MultiHance (GdDTPA-BMA) 0.1 mmol/kg body weight was injected as a bolus, with a flow rate of 2.0 mL/s, followed by a flush of 20 mL of saline. Post processing and kinetic curve analysis were done using mean curve technique; ROI was placed in the most enhanced area within the mass. MRS was done using single voxel technique after localising the chemical signal centred in the area of interest.
Imaging Features
Mammography
On mammography these lesions are ovoid in shape and show heterogeneous parenchymal density with hypodense fat containing areas [Table/Fig-1a,b]. Thin pseudocapsule can be seen surrounding the mass. They can show internal fat densities and radiolucent halos on mammogram. It can present as mixed density masses on mammography with fat and soft tissue densities and benign calcification.
Digital mammogram MLO view (a) and CC view (b) of hamartoma -A mixed density mass involving the upper outer quadrant of left breast. It is of equal density as the rest of the parenchyma showed fat densities within the mass (arrow). This mass showed partially obscured margins on 2-D mammogram however it showed fairly well defined margins on tomosynthesis in CC view (c). It is seen compressing the adjacent parenchyma (arrow).
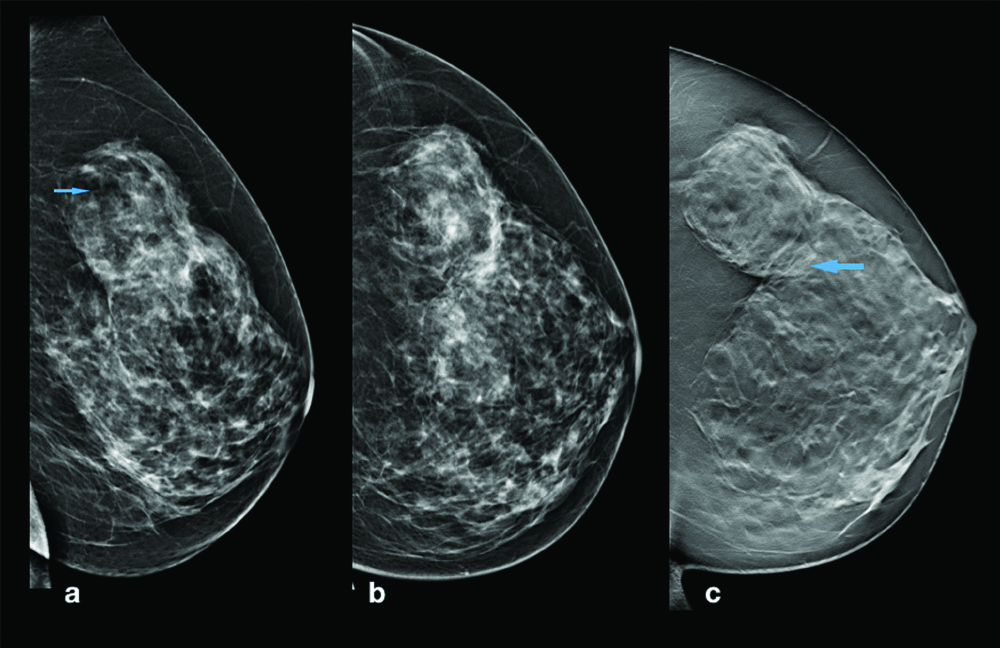
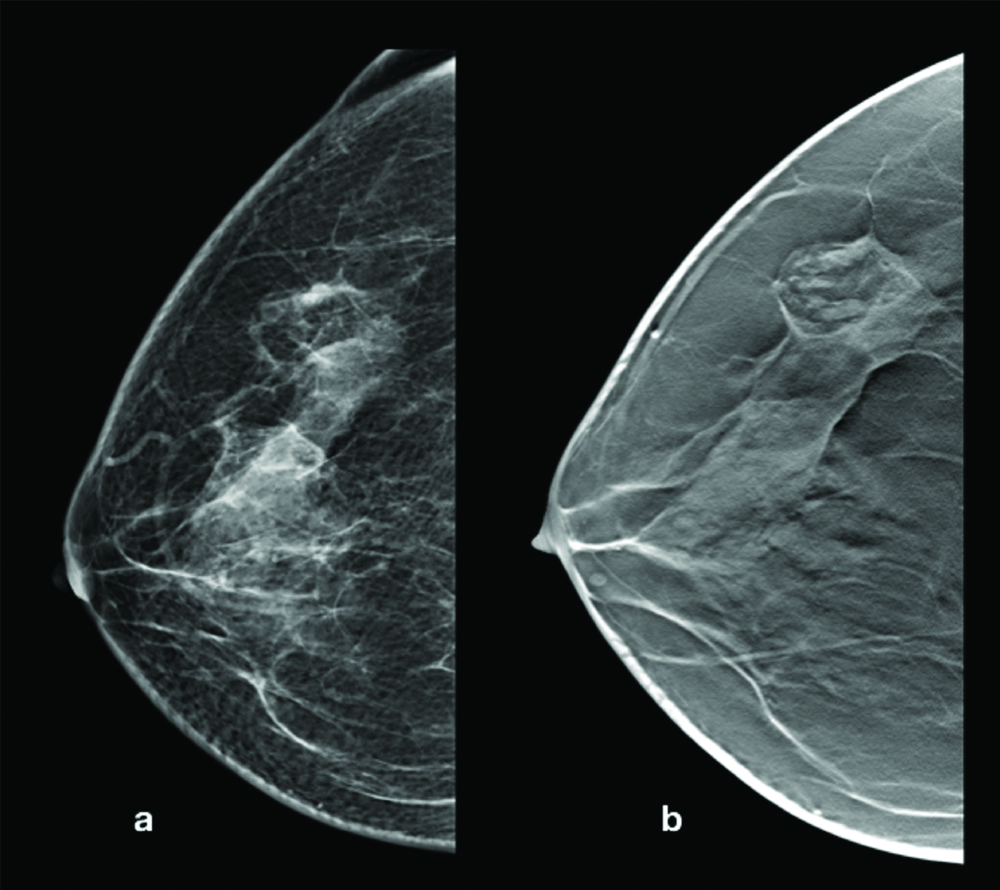
Three Dimensional (3D) Tomosynthesis show better visualisation of the lesion and the pseudocapsule [Table/Fig-1c]. Hamartomas show mixed density depending on the fibrous and fatty content of the tumour [Table/Fig-2]. On mammography these lesions show mild compression of the adjacent parenchyma with displacement of the tissue if large in size; however does not cause architectural distortion [Table/Fig-3]. Microcalcification was not observed in these cases. Mammography is a good modality to diagnose the hamartomas, however it is radiation based technique and in the younger population with dense breast the mass cannot be well visualised. Tomosynthesis are the better imaging modality to visualise the margins and imaging features of the breast masses.
Hamartoma incidentally detected in right breast in a case of left sided breast carcinoma- Mammogrm CC view of the patient showing a suspicious density (a). On tomosynthesis in CC view it is seen as well defined mass with mixed densities, predominantly fat densities.
Digital mammogram MLO view (a) and CC view (b) of hamartoma -A large well defined mass seen in the right breast. It is slightly of more density than the rest of the parenchyma with few areas of fat densities. On tomosynthesis in MLO view (c). It is seen compressing the adjacent parenchyma. (arrow).
Ultrasound
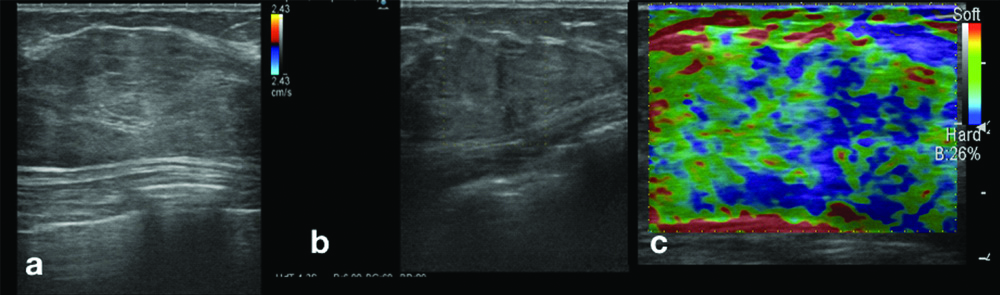
On ultrasound hamartomas are seen as fairly well defined masses surrounded with capsule. These appear as mixed echotexture which consists of hypoechoic and hyperechoic masses as compared to adjacent parenchyma [Table/Fig-4a]. The lesions are compressible with transducer’s pressure. These are always avascular on colour doppler studies as it contain fat and fibrous tissues [Table/Fig-4b]. On elastography, hamartomas showed firm consistency [Table/Fig-4c]. Its compressibilty depends upon the amount of the adipose tissue it contains. Compressibility of the mass is also a feature of the benign breast tumour [8,12]. Breast ultrasound is an operator dependent technique and needs an experience for interpretation. Hamartoma can give variable sonographic appearance and microcalcifications may not be visualised on ultrasound.
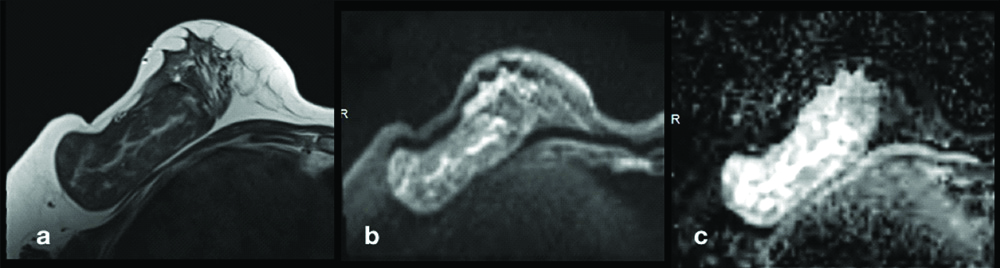
Ultrasound breast showing a hamartoma. An heterogeneous mixed echotexture mass with capsule. Ultrasound of the above patient showed a well defined large capsulated heterogeneous mass (a); On colour doppler it did not show any internal vascularity (b); On ultrasound elastography the mass showed a firm consistency (c).
Magnetic Resonance Imaging
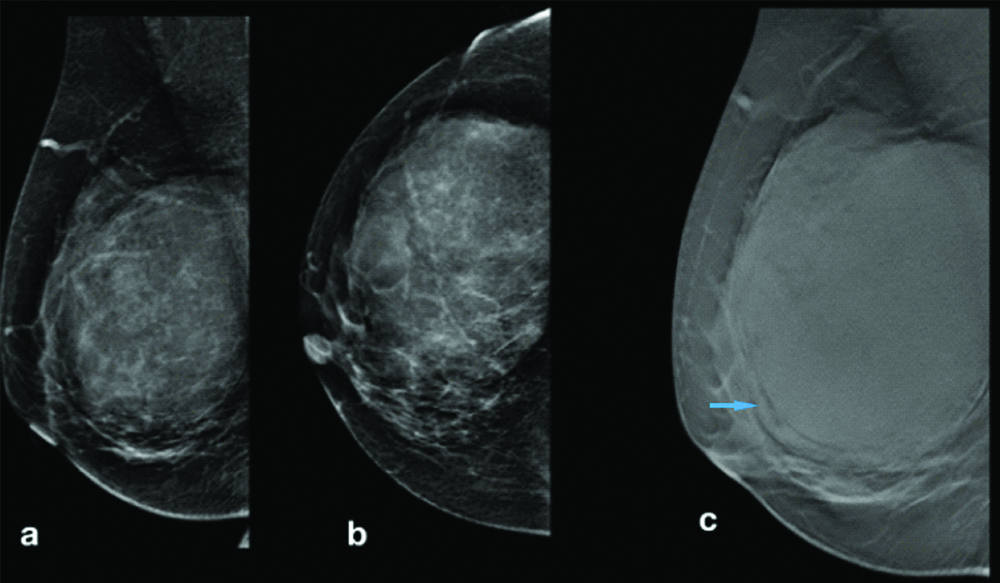
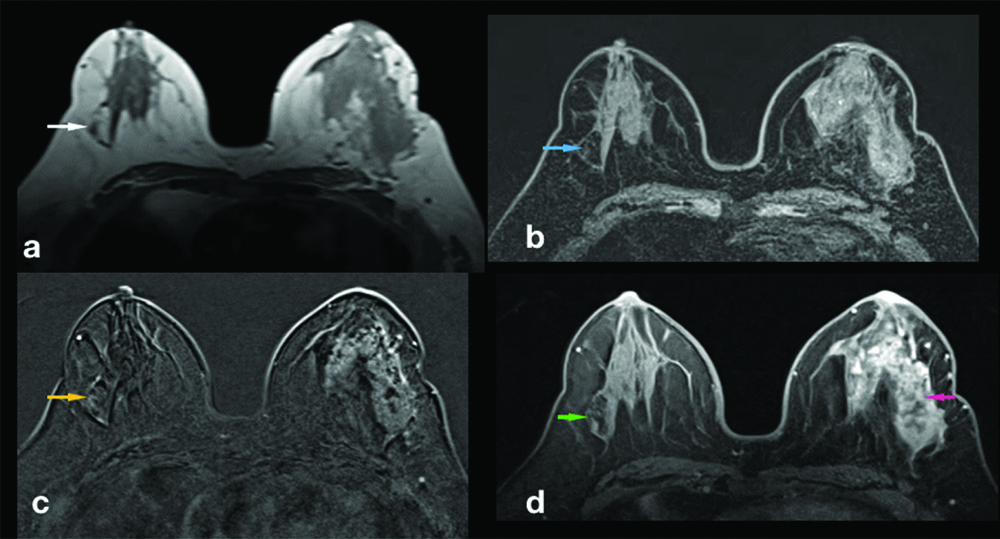
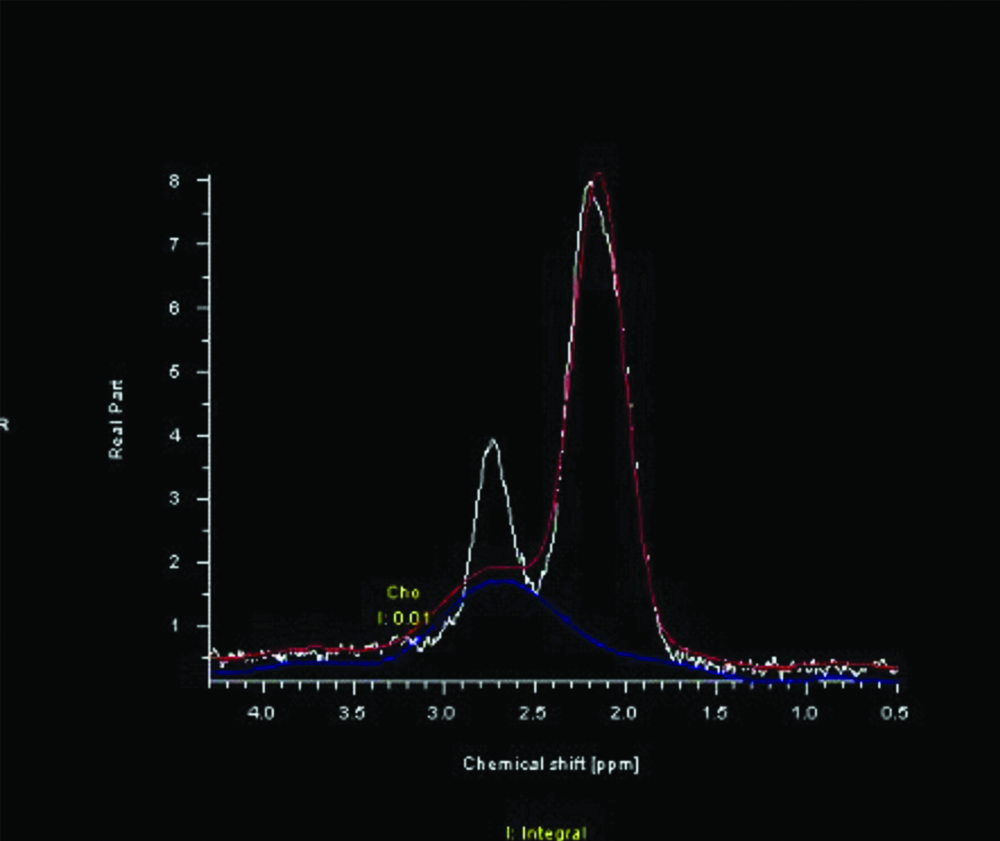
Hamartomas are better visualised on MRI. On MRI these masses are easy to diagnoses as all the contents of the masses like fat, fibrous and glandular tissue are distinguished in various sequences. Pseudocapsule are seen as hypointense rim, hamartomas show mixed signal intensity on T1WI and T2WI with fat and soft tissue signal intensities [Table/Fig-5a,b]. On dynamic post contrast MRI these lesions show gradual, progressive enhancement with type I kinetic curve. It can show similar enhancement as normal breast parenchyma [Table/Fig-5c,d]. These lesions show the signal intensity similar to the breast (breast within the breast) [Table/Fig-6a]. On DWI these lesions do not show restriction with high ADC values, mean ADC values was 1.352±0.62 X10-3 mm2/s and mean ADC values of normal breast was 1.024±0.68 X10-3 mm2/s [Table/Fig-6b,c]. MRS provides information about the biochemical structure and metabolites of tissues. MRS detects lactate and water peak with low choline in these masses [Table/Fig-7]. It is similar to the normal breast tissue.
Hamartoma incidently detected in right breast in a case of left sided breast carcinoma: (a) T2WI MRI showed a well defined oval mass in left breast (white arrow); b) it showed hypointense signal on T1WI fat sat images shown as blue arrow; (c) Dynamic post contrast T1WI FS subtracted image, hamartoma in right breast did not show enhancement (yellow arrow). (d) Dynamic post contrast T1WI FS non-subtracted image did not show post contrast enhancement in hamartoma (green arrow) and malignant lesion on left breasts showed enhancement (red arrow).
MRI imaging in Hamartoma- Axial T2WI revealed a well defined, large capsulated mass with mixed signal intensity and showed fat signal intensities in the mass (a); On Axial DWI the mass did not show restriction (b); and showed high ADC values (c).
MRS in the hamartoma showed low choline values.
Pathology
Hamartomas do not possess specific diagnostic histologic features; therefore diagnosis is difficult, especially on biopsy or FNAC [6]. When fibrous tissue in the lobules or fat and fibrous tissue in the stroma observed with or without pseudoangiomatous changes, there is possibility of Hamartoma [6]. A correlation with imaging findings and clinical findings are always helpful in the diagnosis.
Limitation
Mammography is not sensitive in the dense breast parenchyma. Ultrasound is an operator dependent technique. MRI is very expensive and long investigation is required. It need expertise of radiologist and patient co-operation. It can not be performed in the claustrophobic patients.
Conclusion
Hamartomas are oval encapsulated benign masses which does not show micro calcification on ultrasound, most hamartomas reveal hyper echoic, or mixed echotexture. On mammography they show mixed density masses which contain fat density. MRI is a very sensitive non invasive, non radiation technique for the diagnosis of the Hamartoma of breast. Hamartomas do not possess specific histopathology features and diagnosis requires clinical and radiological correlation. Functional MR techniques like DWI and MRS can be used to confirm the MRI diagnosis.
[1]. Tse GM, Law BK, Ma TK, Chan AB, Pang LM, Chu WC, Hamartoma of the breast: A clinicopathological reviewJournal of Clinical Pathology 2002 55:951-54.10.1136/jcp.55.12.95112461066 [Google Scholar] [CrossRef] [PubMed]
[2]. Fisher CJ, Hanby AM, Robinson L, Millis RR, Mammary hamartoma- Review of 35 casesHistopathology 1992 20:99-106.10.1111/j.1365-2559.1992.tb00938.x1559675 [Google Scholar] [CrossRef] [PubMed]
[3]. Arrigoni MG, Dockerty MB, Judd ES, The identification and treatment of mammary hamartomaSurg Gynecol Obstet 1971 133(4):577-82. [Google Scholar]
[4]. Guray M, Sahin AA, Benign breast diseases: Classification, diagnosis, and managementOncologist 2006 11(5):435-49.10.1634/theoncologist.11-5-43516720843 [Google Scholar] [CrossRef] [PubMed]
[5]. Bhatia M, Ravikumar R, Maurya VK, Rai R, “Breast within a breast” sign: Mammary hamartomaMed J Armed Forces India 2015 71(4):377-79.10.1016/j.mjafi.2015.06.00926663968 [Google Scholar] [CrossRef] [PubMed]
[6]. Nami C, Eun SK, Invasive ductal carcinoma in a mammary hamartoma: Case report and review of the literatureKorean J Radiol 2010 11(6):687-91.10.3348/kjr.2010.11.6.68721076596 [Google Scholar] [CrossRef] [PubMed]
[7]. Farrokh D, Hashemi J, Ansaripour E, Breast hamartoma: Mammographic findingsIran J Radiol 2011 8:258-60.10.5812/iranjradiol.449223329952 [Google Scholar] [CrossRef] [PubMed]
[8]. Chao TC, Chao HH, Chen MF, Sonographic features of breast hamartomasJUM 2007 26:447-52.10.7863/jum.2007.26.4.44717384041 [Google Scholar] [CrossRef] [PubMed]
[9]. Fechner RE, Fibroadenoma and related lesions. In: Page D L, Anderson T J, editorsDiagnostic Histopathology of the Breast 1987 EdinburghChurchill Livingstone:72-85. [Google Scholar]
[10]. Erdem G, Karakas HM, Isik B, Firat AK, Advanced MRI findings in patients with breast hamartomasDiagn Interv Radiol 2011 17(1):33-37. [Google Scholar]
[11]. Yadav P, Chauhan S, Effectivity of combined diffusion-weighted imaging and contrast-enhanced MRI in malignant and benign breast lesionsPolish Journal of Radiology 2018 83:82-93.10.5114/pjr.2018.7436330038683 [Google Scholar] [CrossRef] [PubMed]
[12]. Cole-Beuglet C, Soriano RZ, Kurtz AB, Goldberg BB, Fibroadenoma of the breast: Sonomammography correlated with pathology in 122 patientsAJR Am J Roentgenol 1983 140:369-75.10.2214/ajr.140.2.3696600356 [Google Scholar] [CrossRef] [PubMed]