Anaesthetic Management of a Patient with Myasthenia Gravis for Laparascopic Cholecystectomy: A Case Report
Jaya Choudhary1, Aaditya Prabhudesai2, Anshika Agarwal3
1 Consultant, Department of Anaesthesiology and Pain Medicine, Medica Superspecialty Hospital, Kolkata, West Bengal, India.
2 Postgraduate Trainee, Department of Aanesthesiology and Pain Medicine, Medica Superspecialty Hospital, Kolkata, West Bengal, India.
3 Postgraduate Trainee, Department of Anaesthesiology and Pain Medicine, Medica Superspecialty Hospital, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jaya Choudhary, Medica Superspecialty Hospital, 127, Mukundapur, E M Bypass, Kolkata-700099, West Bengal, India.
E-mail: jayachoudhry11@gmail.com
Myasthenia gravis is an autoimmune disease, which presents as fatigue and muscle weakness due to destruction of nicotinic receptors. Perioperative management of such patients is challenging due to altered pharmacology of drugs especially muscle relaxants and opioids as well as high incidence of postoperative respiratory complications. Here, authors report a new anaesthetic technique for avoiding muscle relaxants and opioids in a myasthenia gravis patient using a combination of total intravenous anaesthesia with bilateral subcostal Transverses Abdominis Plane (TAP) block.
Dexmedetomidine, Muscle relaxants, Subcostal transversus abdominis plane block
Case Report
A 42-year-old female patient, suffering from acute cholecystitis was planned for laparoscopic cholecystectomy. She was diagnosed to have myasthenia gravis ten years back when she presented with progressive fatigue and weakness involving upper limbs. She was graded as Osserman’s Class IIA and was on medical management since then [1]. At the time of surgery, her symptoms were well-controlled with 60 mg pyridostigmine (thrice daily) and 10 mg prednisolone (once daily). There was no history suggestive of involvement of respiratory or bulbar muscles. She also gave a history of hypothyroidism, which was well controlled with 100 μg thyroxin. Her preoperative haematological, biochemical parameters and pulmonary function test were normal. After explaining the risks involved; a written informed consent was obtained from the patient.
She received 60 mg pyridostigmine, 10 mg prednisolone, 100 μg thyroxin and 150 mg ranitidine in the morning of surgery. In the operating room after applying all standard ASA monitors, intravenous dexmedetomidine was administered in a dose of 1 μg/kg over 10 minutes followed by maintenance infusion at 0.7 μg/kg/minute. Patient was induced with fentanyl 100 μg, and propofol 100 mg. Proseal LMA Size 3 was inserted without muscle relaxant. Propofol infusion was started to achieve a BIS of 40-45 intraoperatively. A BIS value of 40-45 was maintained intraoperatively to facilitate the surgery and avoid coughing and bucking.
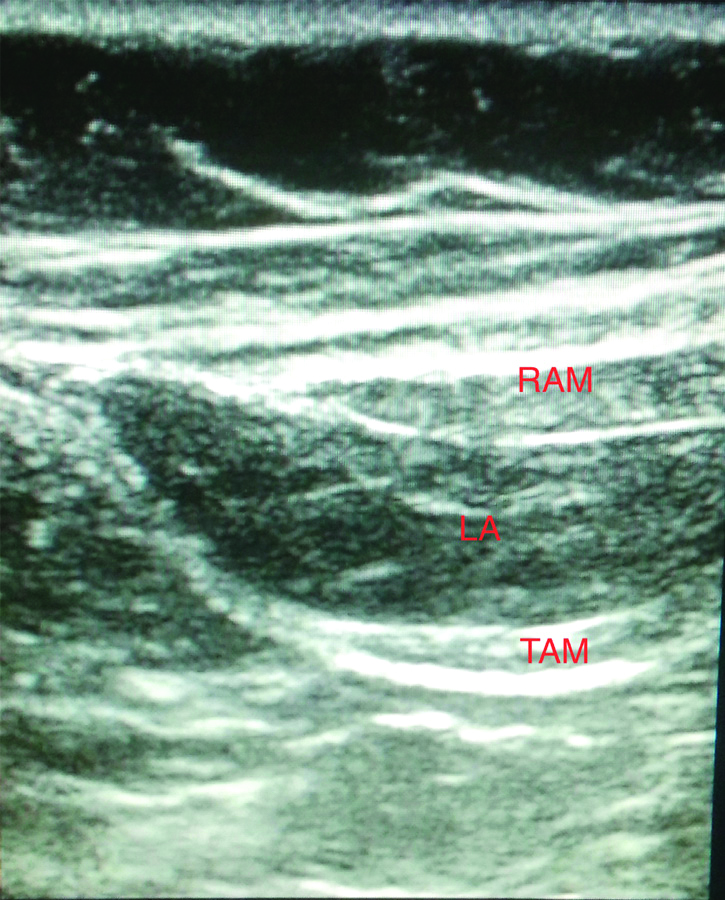
After induction, under aseptic precautions, the ultrasound probe was placed along the costal margin for bilateral subcostal TAP block [2]. The neurofascial plane between the rectus abdominis and the transversus abdominis muscle was identified and traced laterally to visualise the plane between the internal oblique and the transversus abdominis muscles. A 22 G, 10 cm needle was inserted from the xiphisternum and advanced in this neurofascial plane to inject 20 mL 0.25% bupivacaine with 4 mg dexamethasone bilaterally [Table/Fig-1]. Surgical incision was allowed fifteen minutes later to allow adequate spread of local anaesthetic. Pneumoperitoneum was created slowly and intra-abdominal pressure was kept <12 mmHg. Patient received additional 50 μg fentanyl, 1 gm paracetamol and 75 mg diclofenac during the procedure as a part of multimodal analgesia.
Spread of local anaesthetic in the neurofascial between RAM and TAM after subcostal TAP block.
RAM: Rectus abdominis muscle; TAM: Transversus abdominis muscle; LA: Local anaesthetic
Patient remained spontaneously breathing during the procedure and tolerated the Synchronised Intermittent Mandatory Ventilation+Pressure Support (SIMV+PS) mode of ventilation, well. Whereas dexmedetomidine infusion was stopped prior to the closure of abdominal port incisions, propofol infusion was stopped after abdominal port closure. LMA was removed after 15 minutes when she was obeying verbal commands. Postoperatively, she was haemodynamically stable and her postoperative pain was well controlled with a combination of paracetamol and diclofenac. Rest of her perioperative course remained uneventful.
Discussion
Laparoscopic cholecystectomy is one of the commonest surgeries performed. Neuromuscular Blockers (NMB) facilitate controlled ventilation and provide improved surgical conditions for laparoscopic surgeries. However, myasthenic patients demonstrate increased sensitivity and unpredictable response to muscle relaxants even with minimal disease or in remission phase [3]. The commonly used intermediate acting NMB; rocuronium, vecuronium and cisatracurium have shown similar sensitivity in myasthenia patients [4]. Despite dose reduction, the use of non-depolarizing NMB may predispose these patients to prolonged postoperative ventilation and associated respiratory complications. Such complications are highly undesirable after minimally invasive procedures like laparoscopic cholecystectomy. Sugammadex has shown rapid recovery of the neuromuscular function after administration of rocuronium in myasthenics [5,6]. However, sugammadex is still not available in many parts of the world including India.
Various non-muscle relaxant techniques such as total intravenous anaesthesia, inhalationals and epidural anaesthesia have been used to avoid neuromuscular blockers and associated post-operative complications [4]. Propofol in combination with short acting opioids is highly effective in avoiding intraoperative use of muscle relaxants. Amongst the opioids; remifentanil has been considered ideal adjuvant in myasthenics due to its potent analgesic effect and short duration of action. Dexmedetomidine is a highly selective alpha-2 agonist with excellent sedative and analgesic properties. Post-operative respiratory depression is a major concern in myasthenics. Dexmedetomidine stands out from other agents due to its property to preserve of patient’s respiration even at very high doses [7]. Also, due to the rapid offset of remifentanil; intraoperative infusion of dexmedetomidine has shown to provide more stable postoperative haemodynamics and better postoperative analgesia as compared to remifentanil [8]. Dabbous AS reported successful use of dexmedetomidine with isoflurane and propofol in two myasthenic patients undergoing trans-sternal thymectomy [9]. However, inhalational including isoflurane are known to have neuromuscular blocking effect [4]. As laparoscopic cholecystectomy is less invasive than thymectomy, we could avoid inhalationals altogether using propofol with dexmedetomidine.
Georgiou L et al., reported successful management of laparoscopic cholecystectomy in a myasthenia patient using a combination of thoracic epidural and general anaesthesia [10]. However, subcostal block is less invasive as compared to epidural anesthesia and provides excellent pain relief after laparascopic cholecystectomy when used as a component of multimodal analgesia [2]. Dexmedetomidine and TAP block both are known to reduce the perioperative requirement of opioids and associated postoperative respiratory depression, which proved extremely beneficial in the present patient [3,11]. The novelty of our anaesthetic management lies in the fact that a combination of total intravenous anaesthesia and TAP block has never been reported as a technique to avoid muscle relaxants and opioids in myasthenia gravis patients.
Conclusion
Myasthenia gravis patients remain a challenge to the anaesthesiologists and require detailed assessment and planning for their successful management. Dexmedetomidine maybe considered as a safe and effective alternative to remifentanil in combination with propofol for providing satisfactory surgical conditions in myasthenic patients undergoing laparoscopic cholecystectomy. Addition of bilateral subcostal TAP block in such patients prove beneficial by providing excellent pain relief and reducing the requirement of opioids in the perioperative period.
[1]. Osserman KE, Peter K, Cohen E, Genkins G, Mendelow H, Studies in myasthenia gravis: a review of two hundred eighty-two cases at the Mount Sinai Hospital, New York CityAMA Archives of Internal Medicine 1958 102(1):72-81.10.1001/archinte.1958.0026019007400813558746 [Google Scholar] [CrossRef] [PubMed]
[2]. Tolchard S, Davies R, Martindale S, Efficacy of the subcostal transversus abdominis plane block in laparascopic cholecystectomy: Comparison with conventional port-site infiltrationJ Anaesthesiol Clin Pharmacol 2012 28(3):339-43.10.4103/0970-9185.9833122869941 [Google Scholar] [CrossRef] [PubMed]
[3]. Lumb AB, Calder I, “Cured” myasthenia gravis and neuromuscular blockadeAnaesthesia 1989 63:497-500. [Google Scholar]
[4]. Blichfeldt-Lauridsen L, Hansen BD, Anaesthesia and myasthenia gravisActa Anaesthesiol Scand 2012 56:17-22.10.1111/j.1399-6576.2011.02558.x22091897 [Google Scholar] [CrossRef] [PubMed]
[5]. Ulke ZS, Yavru A, Camci E, Ozkan B, Toker A, Senturk M, Rocuronium and sugammadex in patients with myasthenia gravis undergoing thymectomyActa Anaesthesiol Scand 2013 57(6):745-48.10.1111/aas.1212323678983 [Google Scholar] [CrossRef] [PubMed]
[6]. de Boer HD, van Egmond J, Driessen JJ, Booij LH, A new approach to anaesthesia management in myasthenia gravis: reversal of neuromuscular blockade by sugammadexRev Esp Anestesiol Reanim 2010 57(3):181-84.10.1016/S0034-9356(10)70194-8 [Google Scholar] [CrossRef]
[7]. Ramsay MAE, Luterman DL, Dexmedetomidine as a total intravenous anaesthetic agentAnaesthesiology 2004 101:787-90.10.1097/00000542-200409000-0002815329604 [Google Scholar] [CrossRef] [PubMed]
[8]. Rajan S, Hutcherson MT, Sessler DI, Kurz A, Yang D, Ghobrial M, The effects of dexmedetomidine and ramifentanil on hemodynamic stability and analgesic requirement after craniotomyJ Neurosurg Anaesthesiol 2016 28(4):282-90.10.1097/ANA.000000000000022126325514 [Google Scholar] [CrossRef] [PubMed]
[9]. Dabbous AS, Anaesthesia with dexmedetomidine in two myasthenic patients undergoing trans- sternal thymectomyBr J Anaesth 2012 :10910.1093/bja/el_9146 [Google Scholar] [CrossRef]
[10]. Georgiou L, Bousoula M, Spetsaki M, Combined thoracic epidural and general anaesthesia with laryngeal mask airway for laparoscopic cholecystectomy in a patient with myasthenia gravisAnaesthesia 2001 55(8):821-22.10.1046/j.1365-2044.2000.01629-24.x10947722 [Google Scholar] [CrossRef] [PubMed]
[11]. Carollo DC, Nossaman BD, Ramadhyani U, Dexmedetomidine: A review of clinical applicationsCurrent opinion in Anaesthesiology 2008 21(4):457-61.10.1097/ACO.0b013e328305e3ef18660652 [Google Scholar] [CrossRef] [PubMed]