Unilateral Grave’s Disease: A Rare Variant
Arun Pande1, Ajay Aggarwal2, Roopak Wadhwa3
1 Consultant, Department of Endocrinology, Sahara Hospital, Lucknow, Uttar Pradesh, India.
2 Senior Consultant, Department of Endocrinology, Fortis Hospital, New Delhi, India.
3 Consultant, Department of Endocrinology, Fortis Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Ajay Aggarwal, Senior Consultant, Department of Endocrinology, Fortis Hospital, Shalimar Bagh, New Delhi-110088, India.
E-mail: endocrinologist39@yahoo.co.in
Grave’s Disease (GD), an autoimmune disorder, usually presents as diffuse goitre with involvement of both lobes of the thyroid gland. It is characterised by hyperthyroidism, ophthalmopathy and rarely dermopathy. Involvement of eyes can be unilateral or bilateral, but unilateral involvement of a lobe in a bilobar thyroid gland is very rare. Only 13 cases of unilateral GD have been reported so far. This entity may be missed quite often for thyroid hemiagenesis or hyperfunctioning thyroid nodule. Here, authors present a case of unilateral thyroid lobe involvement in a patient of GD.
Goitre, Methimazole, Thyroid
Case Report
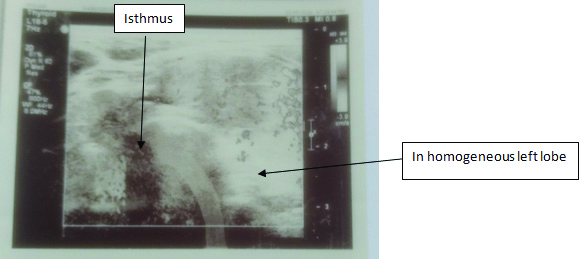
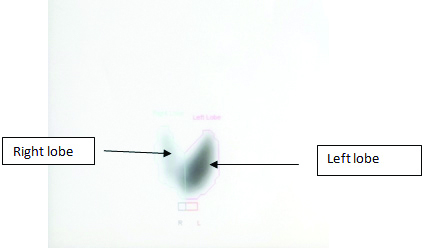
A 35-year-old female presented with symptoms and signs suggestive of thyrotoxicosis which included fatigue, heat intolerance, palpitation, weight loss and tremors for the past 2 to 3 weeks. The palpation of thyroid gland revealed non-tender, diffuse enlargement of left thyroid lobe with no definite nodules. Right lobe was normally palpable with no apparent increase in size. There were no eye signs and skin lesions. There was no family history of thyroid diseases. Her thyroid function tests revealed high T3 (6.56 nmol/L), high T4 (252.2 nmol/L), and an undetectable TSH (<0.01 mIU/L). Serum thyroid receptor antibodies (TRAbs, 2.4 IU/L, normal <1 U/L) and Anti-Thyroperoxidase Antibodies (Anti-TPO) (132 IU/mL, normal <35 IU/mL) were positive. The ultrasound neck showed non-nodular, enlarged, and heterogeneous left lobe, whereas right lobe of thyroid gland appeared homogeneous [Table/Fig-1]. The Tc99m thyroid scan showed enlarged left lobe of thyroid gland with uniform uptake. There was no uptake in the normal-sized right lobe [Table/Fig-2]. These findings supported the diagnosis of unilateral GD involving left thyroid lobe. The patient was started on methimazole (10 mg twice daily) and propranolol (10 mg twice daily). At four-week follow-up, she reported significant clinical improvement. Her thyroid function tests showed normal T3 (1.81 nmol/L), normal T4 (109.7 nmol/L), low TSH (0.217 mIU/L). The patient went into remission after 10 months of anti-thyroid therapy.
Ultrasound of thyroid gland with Unilateral GD.
A 99m Tc thyroid scan of patient with unilateral GD involving left lobe.
Discussion
Grave’s Disease (GD) is characterised by hyperthyroidism, ophthalmopathy and rarely dermopathy. The pathogenesis of GD involves stimulation of both lobes of thyroid gland by TRAbs, leading to thyrotoxicosis. Grave’s ophthalmopathy occurs in 25-50% patients. The involvement of eyes can be unilateral or bilateral [1,2]. Thyroid scan reveals bilateral diffuse uptake of radioisotopes. However, involvement of unilateral lobe in a bilobar thyroid gland is rare. Few cases of unilateral goitre in patients with GD due to hemi-agenesis of either lobe of thyroid gland have been published in the literature [3-6]. Only 13 cases of GD with unilateral involvement of bilobar thyroid gland have been reported so far [Table/Fig-3] [7-17]. Right thyroid lobe was involved in 11 cases [7-12,14-16] whereas only two patients had left lobe involvement [13,17].
Summary of all cases of unilateral Grave’s disease published in literature [7-17].
| Case | Age (Y) | Sex | Lobe involved | TRAb/Anti-TPO Ab | Scintigraphy (Tc/RAIU uptake) | USG/Doppler thyroid gland | Treatment | Reference No. |
|---|
| 1. | 55 | F | Right | -/+ | Diffuse uptake right lobe | Enlarged rt lobe, low echogenecity | Surg/MMZ | [7] |
| 2. | 61 | F | Right | -/+ | Diffuse uptake right lobe | Non-nodular, homogeneous | Surg/MMZ | [7] |
| 3. | 31 | F | Right | +/+ | Enlarged right lobe, uptake homogeneous | Non-nodular rt lobe, echogenicity homogeneous | MMZ | [8] |
| 4. | 33 | F | Right | +/+ | Increased uptake right lobe | Rt lobe enlarged inhomogeneous echogenecity | MMZ | [9] |
| 5. | 39 | M | Right | +/+ | Increased uptake right lobe | Non-nodular non-homogeneous pattern | MMZ | [10] |
| 6. | 23 | M | Right | +/- | Diffuse uptake right lobe | Heterogeneous echogenecity rt lobe | PTU | [11] |
| 7. | 49 | F | Right | -/- | Homogeneous uptake right lobe | Heterogeneous parenchyma | Anti thyroid drugs | [11] |
| 8. | 63 | M | Right | NA/+ | Enlarged right lobe, uptake homogeneous | Rt lobe enlarged, coarse texture, no nodules | N.A. | [12] |
| 9. | 48 | F | Left | +/+ | Lt lobe uniform increased activity | Non-nodular heterogeneous lt lobe | RAI ablation | [13] |
| 10. | 40 | M | Right | NA/+ | Diffuse uptake right lobe | Rt lobe, Non-nodular, enlarged heterogeneous | Anti-thyroid therapy | [14] |
| 11. | 18 | F | Right | +/+ | Increased uptake right lobe | Enlarged rt lobe heterogeneous | MMZ | [15] |
| 12. | 42 | F | Right | +/+ | Uniform unilateral uptake | Hypervascular, non-homogeneous, enlarged rt lobe | MMZ | [16] |
| 13. | 44 | F | Left | +/+ | Diffuse uptake left lobe | Hypervascular, heterogeneous, non-nodular lobe | MMZ | [17] |
Surg: Surgery; MMZ: Methimazole; PTU: Propylthiouracil; RAI: Radioiodine; NA: Not available
Unilateral GD, not due to thyroid hemi-agenesis, is very rare. In 1993, Sakata S et al., reported two cases of right sided unilateral GD for the first time [7]. TRAbs were negative initially but were tested positive later on. These patients underwent right hemi-thyroidectomy and later on developed thyrotoxicosis due to left lobe hyperfunction and required methimazole.
In all case reports [8-17], the patients were diagnosed to have unilateral GD on the basis of clinical presentation, physical examination, positive thyroid antibodies and imaging. The ultrasound showed enlarged involved lobe with heterogenous echogenicity, whereas doppler study showed hypervascularity of the involved lobe. Scintigraphy (99Tc/RAIU) revealed uniform uptake of radioisotope in the involved thyroid lobe. The diagnosis of unilateral GD was further confirmed by the presence of TRAbs and Anti-TPO antibodies.
Scott M et al., evaluated Automated Electrochemiluminescence Immunoassay (ECLIA) in clinical routine and compared it with established TRAb assays among 508 GD, 381 other patients with established thyroid disorders and 446 normal controls [18]. The highest sensitivity (99%) and specificity (99%) was seen at a cut-off level of 1.75 IU/L. Here, the calculated positive predictive value was 95% and negative predictive value was 100%. Applying the ROC plot-derived cut-off of 1.75 IU/l, sensitivity for newly diagnosed GD patients. TRAb positivity within the group of newly diagnosed GD patients was 97%, which was in accordance to the sum of different non-automated porcine TSH receptor-based assays with a sensitivity of 94%. The TRAb level (2.4 IU/L) in the present patient was suggestive of unilateral GD.
Left lobe is not commonly involved in patients, two out of thirteen cases were reported in the literature [Table/Fig-3]. The present patient is the third case with left lobe involvement. The exact cause of unilateral lobe involvement in GD is not known. Bolognasi M and Rossi R, proposed that it may be due to larger size of right lobe and because this lobe is more frequently affected by nodular and non-nodular conditions [10]. As both thyroid lobes are exposed to TRAbs, usually both lobes are involved in GD. Several other explanations have been put forth like it may be due to chance or may be due to pre-existing structural or functional changes due to congenital (separate lymphatic drainage) or acquired factors (previous viral inflammation in the silent lobe) [7]. The presence of chronic thyroiditis or silent thyroiditis in uninvolved lobe may be a possibility, but these lesions involve both lobes usually. Muller Gartner HW et al., proposed existence of functional heterogeneity in GD tissue which causes resistance to stimulating immunoglobulins [19]. Sodium/Iodine Symporter (NIS), located on basolateral membrane of thyroid follicle, mediate iodine transport [20]. In GD, there is abundant NIS immuno-reactivity suggestive of diffuse uptake of iodide. Local suppression of NIS gene expression and function may be responsible for the development of impaired radioisotope uptake by thyroid tissue is another possible explanation [12].
The authors propose that unilateral to bilateral involvement of the thyroid gland may be natural history of GD. The time duration from unilateral to bilateral progression may be very small. Hence, very few cases of GD with unilateral involvement are diagnosed. Due to some anatomical difference among the thyroid lobes or may be due to infection, the unilateral to bilateral progression may be slow in some cases and hence unilateral GD can be picked up.
The differential diagnosis of unilateral GD includes hyperfunctioning thyroid nodule involving one lobe and hemi-agenesis of thyroid lobe, both of which can be easily diagnosed on ultrasound. Another possibility includes unilateral Subacute Thyroiditis (SAT). The differentiating feature between unilateral SAT and unilateral GD include presence of clinical features like fever, pain in thyroid area and elevated acute phase reactants [21].
Conclusion
Unilateral GD of the thyroid gland is very rare, and its aetiology remains unclear. The presence of TRAbs, unilateral diffuse radioisotope uptake and non-nodular inhomogeneous echogenicity on ultrasound points to its diagnosis. Therefore, a diagnosis of unilateral GD should be kept in mind when thyroid scan shows unilateral uptake of radioisotope in a thyrotoxic patient. The treatment should be targeted at both lobes. If required, total thyroidectomy rather than hemithyroidectomy should be the surgical treatment.
Surg: Surgery; MMZ: Methimazole; PTU: Propylthiouracil; RAI: Radioiodine; NA: Not available
[1]. Weetman AP, Grave’s diseaseN Eng J Med 2000 343:1236-48.10.1056/NEJM20001026343170711071676 [Google Scholar] [CrossRef] [PubMed]
[2]. Cooper DS, HyperthyroidismLancet 2003 362:459-68.10.1016/S0140-6736(03)14073-1 [Google Scholar] [CrossRef]
[3]. Mortimer PS, Tomlinson IW, Rosenthal FD, Hemiaplasia of the thyroid with thyrotoxicosisJ Clin Endocrinol Metab 1981 52:152-55.10.1210/jcem-52-1-1527451642 [Google Scholar] [CrossRef] [PubMed]
[4]. Harada T, Nishikawa Y, Suzuki T, Ito K, 3 cases of Basedow’s disease with atresia of unilateral lobe of the thyroid glandHoruman To Rinsho 1969 17:774-76. [Google Scholar]
[5]. Ozaki O, Ito K, Mimura T, Sugino K, Kitamura Y, Iwabuchi H, Hemiaplasia of the thyroid associated with Grave’s disease: report of 3 cases and review of the literatureSurg Today 1994 24:164-69.10.1007/BF024734028054799 [Google Scholar] [CrossRef] [PubMed]
[6]. Shechner C, Kraiem Z, Zuckermann E, Dickstein G, Toxic Grave’s disease with thyroid hemiagenesis: diagnosis using thyroid-stimulating immunoglobulin measurementsThyroid 1992 2:133-35.10.1089/thy.1992.2.1331356055 [Google Scholar] [CrossRef] [PubMed]
[7]. Sakata S, Fuwa Y, Goto S, Fukui M, Yuasa H, Takuno H, Two cases of Grave’s disease with presentation of unilateral diffuse uptake of radioisotopesJ Endocrinol Invest 1993 16:903-07.10.1007/BF033489548144868 [Google Scholar] [CrossRef] [PubMed]
[8]. Dimai HP, Ramschak-Schwarzer S, Lax SS, Lipp RW, Leb G, Hyperthyroidism of Grave’s disease: Evidence for only unilateral involvement of the thyroid gland in a 31-year-old female patientJ Endocrinol Invest 1999 22:215-19.10.1007/BF0334354510219891 [Google Scholar] [CrossRef] [PubMed]
[9]. Gratz S, Barth P, Arnold R, Behr TM, Grave’s disease with unilateral radioisotope uptakeNuclearmedizin 2004 43:N66-68. [Google Scholar]
[10]. Bolognasi M, Rossi R, Unilateral Grave’s diseaseThyroid 2006 16:493-95.10.1089/thy.2006.16.49316756472 [Google Scholar] [CrossRef] [PubMed]
[11]. Kisakol G, Cakir M, Gungor K, Gonen MS, Two cases of Grave’s disease presenting with unilateral involvement of the thyroid glandTurk Jem 2007 11:64-66. [Google Scholar]
[12]. Al Juhanni N, Wagieh Sh, Al Ghanmdi H, Grave’s disease affecting one thyroid lobe (Unilateral Grave’s Disease): Case reportEgyptian J Nucl Med 2010 2:62-65.10.21608/egyjnm.2010.5501 [Google Scholar] [CrossRef]
[13]. Chen LC, Green JB, First reported case of unilateral Grave’s disease in the left lobe of a bilobar thyroid glandThyroid 2011 21:683-86.10.1089/thy.2010.034321563918 [Google Scholar] [CrossRef] [PubMed]
[14]. Gonulalan G, Cakir M, Grave’s disease with unilateral involvement. A rare entityTurk Jem 2011 15:128-29. [Google Scholar]
[15]. Eklioglu BS, Atabek ME, Akyurek N, Tastekin G, Unilateral Grave’s disease in an adolescent: Case reportESPE Abstracts 2015 84:P-3-1219 [Google Scholar]
[16]. AY SA, Baskoy K, Urhan M, Deniz F, Yonem A, A rare variant of hyperthyroidism: Unilateral Grave’s diseaseEndocrine Abstracts 2016 41:EP386 [Google Scholar]
[17]. Stamatouli AM, Lupsa BC, Unilateral Graves Disease in a Patient with Evans Syndrome Responded to RituximabEndocrine Abstracts 2016 :SUN-302 [Google Scholar]
[18]. Schott M, Hermsen D, Broecker-Preuss M, Casati M, Mas JC, Eckstein A, Clinical value of the first automated TSH receptor autoantibody assay for the diagnosis of Graves’ disease (GD): an international multicentre trialClin Endocrinol (Oxf) 2009 71:566-73.10.1111/j.1365-2265.2008.03512.x [Google Scholar] [CrossRef]
[19]. Muller-Gartner HW, Schneider C, Schroder S, Autoimmune-resistance in Grave’s disease tissue indication of a structural and functional heterogenicityActa Endocrinol (Copenh.) 1986 113:233-41.10.1530/acta.0.11302333535326 [Google Scholar] [CrossRef] [PubMed]
[20]. De La Vieja A, Dohan O, Levy O, Carrasco N, Molecular analysis of the sodium/iodine symporter: impact on thyroid and extrathyroid physiologyPhysiol Rev 2000 80:1083-105.10.1152/physrev.2000.80.3.108310893432 [Google Scholar] [CrossRef] [PubMed]
[21]. Sari O, Erhas B, Erbas T, Subacute thyroiditis in a single lobeClin Nucl Med 2001 26:400-01.10.1097/00003072-200105000-0000511317018 [Google Scholar] [CrossRef] [PubMed]