A Rare Case of Ileal Inflammatory Fibroid Polyp with Small Bowel Obstruction
Asfar Ahamed1, Venkatesh Munikrishnan2, Sudeepta Kumar Swain3, Ajay Chanakya Vallabhaneni4
1 Junior Consultant, Department of Colorectal Surgery, Apollo Main Hospital, Chennai, Tamil Nadu, India.
2 Colorectal Surgeon, Department of Colorectal Surgery, Apollo Main Hospital, Chennai, Tamil Nadu, India.
3 Surgical Gastroenterologist, Department of Surgical Gastro, Apollo Main Hospital, Chennai, Tamil Nadu, India.
4 Surgical Oncologist, Department of Colorectal, Apollo Main Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Asfar Ahamed, Junior Consultant, Department of Colorectal Surgery, Apollo Main Hospital, Chennai, Tamil Nadu, India.
E-mail: asfar.ahamed@gmail.com
Inflammatory fibroid polyp is rare idiopathic benign tumour of gastrointestinal tract. The most common site is stomach (gastric antrum) followed by ileum. Ileal inflammatory fibroid polyp usually present with intussusception which has been published in various worldwide literatures. We report a case of 46-year-old lady presented with three days history of abdominal pain, vomiting and low grade fever. Clinically, she was diagnosed with acute small obstruction. Computed Tomography imaging demonstrated Ileo-ileal intussuception with polyp in the location of terminal ileum. Diagnostic laparoscopy was suggestive of Ileo-ileal intussuception due to a polyp 20 cm from ileo-caecal junction. Intussuception was spontaneously reduced and wedge resection was performed on the diseased segment.
Computed tomography, Ileal polyp, Intussuception
Case Report
A 46-year-old female, known case of hypertension, presented to emergency department with history of abdominal pain since 3 days. It was associated with vomiting which was bilious in nature and she also had low grade fever for a day. Her medical, drug and family history were non-contributory. Twelve years back she has undergone total abdominal hysterectomy for uterine myoma.
She was moderately built with all vitals within normal limits. On examination, she had tenderness in the left lumbar region. There was no organomegaly or free fluid. Laboratory analysis revealed 12,000 leukocytes with raised neutrophils. C reactive protein was 13.7 mg/L (Normal <5 mg/L).
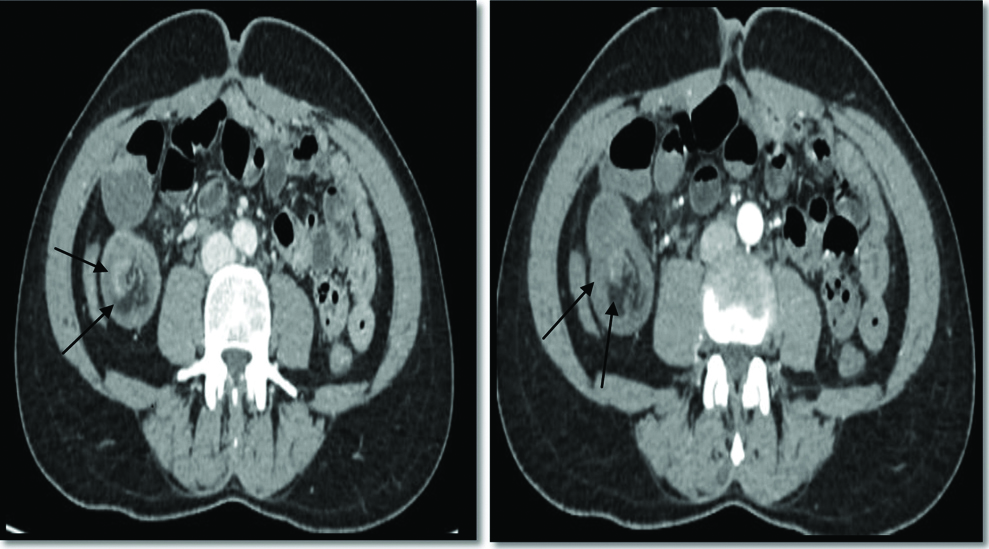
Patient underwent Ultrasonography which showed ileo-ileal intussusceptions with a well-defined mural bowel hypoechoic solid mass as lead point. Computerised Tomography scan, whole abdomen with contrast, suggested ileo-ileal intussuception involving the last loop of ileum for a length of 10 cm. At head of intussusception, a smooth surfaced polyp measuring 5×3 cm was seen. It revealed poor contrast enhancement [Table/Fig-1].
Computerised tomography scan whole abdomen showing smooth surfaced ileal polyp with intussusception.
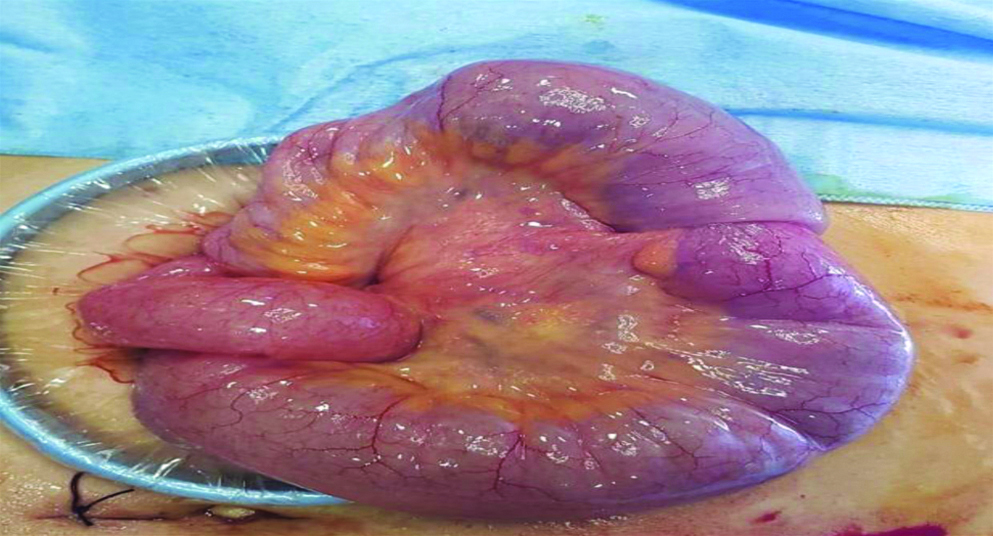
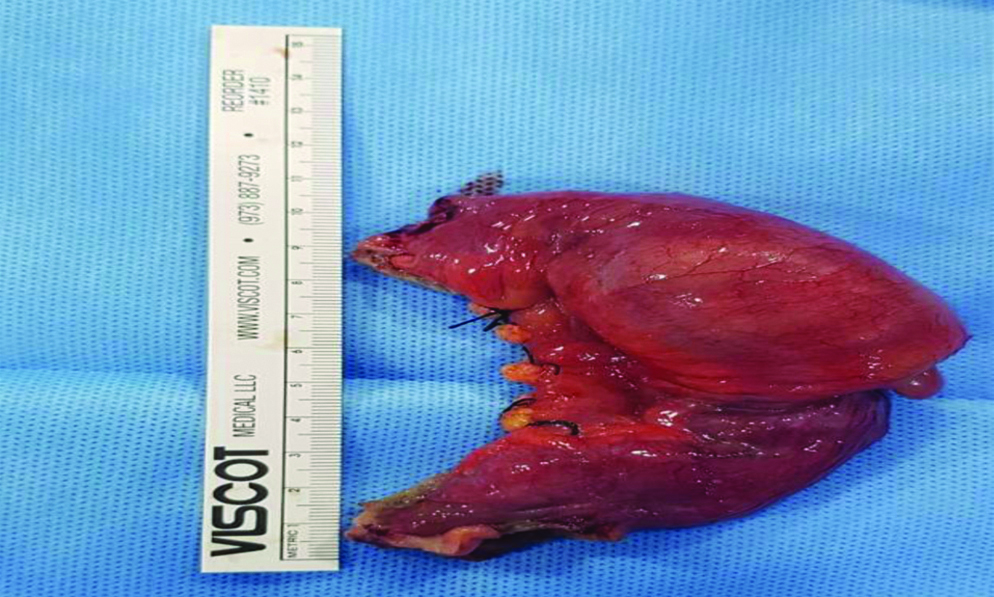
After taking written consent from the patient, she underwent diagnostic laparoscopy. Pneumo-peritoneum was created via Veress needle technique at Umbilical region. Small bowel walk through was performed which was suggestive of ileo-ileal intussusception with polyp 20 cm from ileo-caecal junction. Lower midline incision was performed to extract the diseased segment. Wedge excision of ileo-ileal intussusception with polyp was performed [Table/Fig-2,3] with ileo-ileal anastomosis.
Intraoperative picture of ileal polyp with intussuception.
Intraoperative picture of resected ileal specimen.
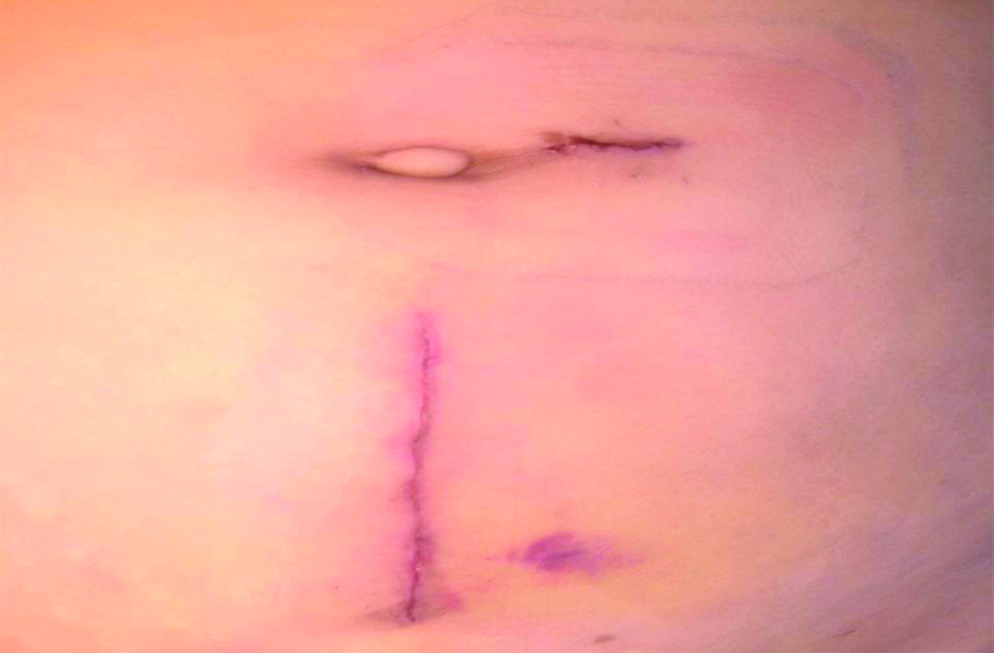
Her post-operative period was uneventful. Patient was started on clear liquid 30 mL/hour on post-operative day one. Next day she opened bowels. Since she was tolerating clear liquid, she was continued with full liquid diet. Patient was discharged on post-operative day 4, with advice for soft solid diet. She came for a check-up after a week. She was doing well. Her abdominal wound was healthy [Table/Fig-4].
Post-operative surgical healthy wound.
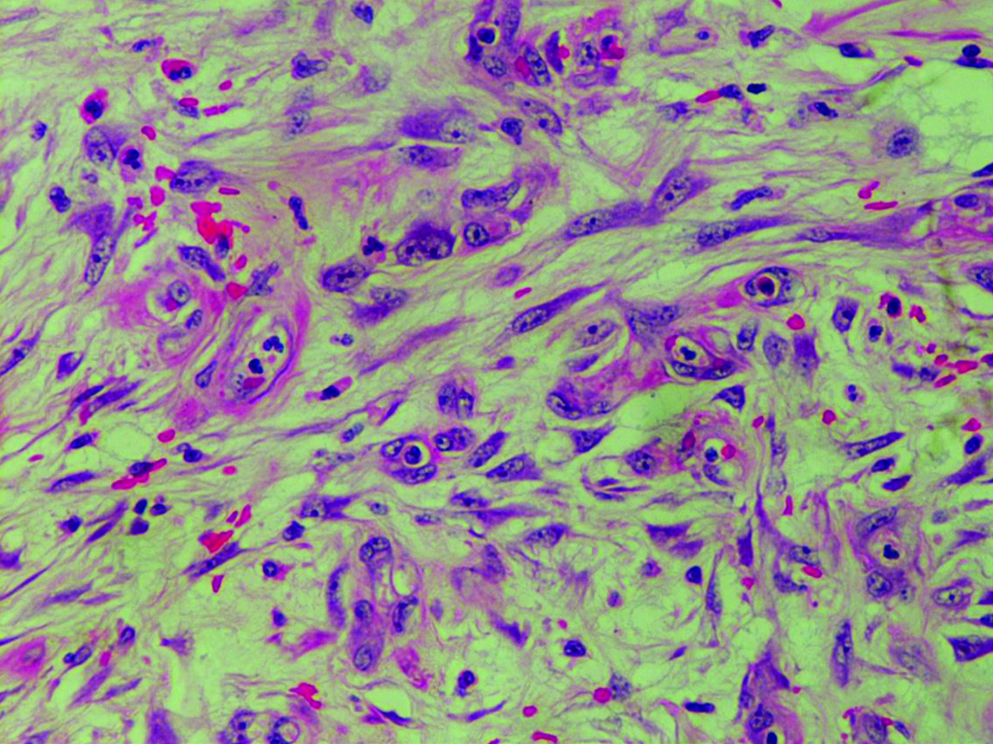
Histopathological examination reported as proliferating capillary vessel in a myxoid stroma with whorls of spindle shaped cell around blood vessel consistent with inflammatory fibroid polyp [Table/Fig-5].
Tumour composed of proliferative oval to spindle cell with capillary sized blood vessels and presence of eosinophils and scattered plasma cells. Presence of a tendency of whorling of spindle shaped cell around blood vessels (H&E x400).
Discussion
Inflammatory Fibroid Polyps (IFP) is rare benign lesions of the gastrointestinal tract with ileum as a rarest location [1]. The term IFP was described by Vanek in 1949 as an eosinophilic submucosal granuloma [2].
The most common site of inflammatory fibroid polyp in gastro-intestinal tract is gastric antrum. Nevertheless, the ileum is the most common site where the intussuception occurs [3]. Colon, gall bladder, oesophagus, duodenum and appendix have also been described as rare sites [4]. Most common age of presentation is fourth to seventh decade of life [4]. In the present case report, the patient belonged to 4th decade.
Macroscopically, the inflammatory fibroid polyp may be polypoidal or sessile and the average size is around 4 cm. However a giant IFP up to 20 cm in diameter have also been reported [5]. Retro-peritoneal IFP measuring up to 20 cm [6] and colon IFP measuring up to 14 cm have also been reported [7].
Schildhaus HU et al., reported 25 cases of small bowel inflammatory fibroid polyp, largest of which was 7 cm and none were found in jejunum [8]. Rehman S et al., presented a case report of a 46-year-old British man with 15 cm polyp in the distal jejunum [1]. The index patient presented with 5 cm polyp with ileo-ileal intussuception in the last loop of ileum.
Microscopically, IFP are characterised by eosinophilic inflammatory response with vascular and fibroblast proliferation [9]. GIST and IFP share same pathological features. Immunohistochemistry differentiates IFP from GIST. Both are positive for CD34 and Vimentin, CD 117 is specific for GIST [10].
Aetiology of IFP is unknown. Trigger including foreign body, chronic pyloric infection, parasite have been suggested, but remain unsupported. In view of marked eosinophilic infiltration in most cases, localised variant of gastroenteritis is another proposed aetiology [3]. Poorly controlled inflammatory response to chemical, traumatic, metabolic mucosal injury has also been hypothesised [1].
IFP are usually asymptomatic. Clinical presentation depends on anatomic location. Gastric IFP may present with pyloric obstruction or anaemia with chronic bleeding. Intussuception is the most common finding when it arises from small bowel [10].
Contrast enhanced CT scan of whole abdomen and enteroscopy are diagnostic modalities to diagnose inflammatory fibroid polyp of small intestine [11,12]. Sensitivity of contrast studies such as small bowel series and barium enema are relatively poor and ultrasonography lacks specificity [13]. Del-pozo G et al., reported a crescent in doughnut sign which helped in diagnosing intussusception via USG [14]. In concordance to this study, the ultrasonography reported well-defined hypoechoic mural band, solid mass lesion arising from the ilieal loop in the right iliac fossa. This lesion acts as a lead point resulting in the entrapment of ileum within ileum manifested as ileo-ileal intussuception. In accordance to other studies, CT scan is most useful which reveals mass with central dense area and a halo with low attenuation, suggestive of intussusceptions [11]. The standard treatment is resection and anastomosis of small bowel [15].
Conclusion
Inflammatory fibroid polyp in ileum is a rare benign entity and they present with acute small bowel obstruction. Wedge resection of the diseased segment with ileo-ileal primary anastomosis should be the standard care of management.
[1]. Rehman S, Gamie Z, Wilson T, Coup A, Kaur G, Inflammatory fibroid polyp (Vanek’s tumour), an unusual large polyp of the jejunum: a case reportCases J 2009 2:715210.1186/1757-1626-2-715219829925 [Google Scholar] [CrossRef] [PubMed]
[2]. Vanek J, Gastric Submucosal granuloma with eosinophilic infiltrationAm J Pathol 1949 25(3):397-411. [Google Scholar]
[3]. Nonose R, Valenciano JS, da Silva CM, de Souza CA, Martinez CA, Ileal intussusception caused by Vanek’s tumour: a Case ReportCase Rep. Gastroenterol 2011 5(1):110-16.10.1159/00032693021503167 [Google Scholar] [CrossRef] [PubMed]
[4]. Wysocki A, Taylor G, Windsor J, Inflammatory fibroid polyps of the duodenum: a review of the literatureDigestive Surgery 2007 24(3):162-68.10.1159/00010209917476106 [Google Scholar] [CrossRef] [PubMed]
[5]. Ozolek J, Sasatomi E, Swalsky P, Rao U, Krasinskas A, Finkelstein S, Inflammatory fibroid polyps of the gastrointestinal tractApplied Immunohistochemistry & Molecular Morphology 2004 12(1):59-66.10.1097/00129039-200403000-00011 [Google Scholar] [CrossRef]
[6]. Van Roggen J, Hogendoorn P, Soft tissue tumours of the retroperitoneumSarcoma 2019 4(1-2):17-26.10.1155/S1357714X0000004918521430 [Google Scholar] [CrossRef] [PubMed]
[7]. Kan H, Suzuki H, Shinji S, Naito Z, Furukawa K, Tajiri T, Case of an inflammatory fibroid polyp of the cecumJ Nippon Med Sch 2008 75:181-86.10.1272/jnms.75.18118648178 [Google Scholar] [CrossRef] [PubMed]
[8]. Schildhaus HU, Cavlar T, Binot E, Buttner R, Wardelmann E, Merkelbach-Bruse S, Inflammatory fibroid polyps harbour mutations in the Platelet-derived growth factor receptor alpha (PDGFRA) geneJ Pathol 2008 216:176-82.10.1002/path.239318686281 [Google Scholar] [CrossRef] [PubMed]
[9]. Kim YI, Kim WH, Inflammatory fibroid polyps of gastrointestinal tract. Evolution of histologic patternsAm J Clin Pathol 1988 89:721-27.10.1093/ajcp/89.6.7213369362 [Google Scholar] [CrossRef] [PubMed]
[10]. Gonul II, Erdem O, Ataoglu O, Inflammatory fibroid polyp of the ileum causing intussusception: a case reportTurk J Gastroenterol 2004 15:59-62. [Google Scholar]
[11]. Warshauer DM, Lee JK, Adult intussusception detected at CT or MR imaging: clinical-imaging correlationRadiology 1999 212:853-60.10.1148/radiology.212.3.r99au4385310478257 [Google Scholar] [CrossRef] [PubMed]
[12]. Harned RK, Buck JL, Shekitka KM, Inflammatory fibroid polyps of the gastrointestinal tract: radiologic evaluationRadiology 1992 182:863-66.10.1148/radiology.182.3.15359091535909 [Google Scholar] [CrossRef] [PubMed]
[13]. Desai N, Wayne MG, Taub PJ, Levitt MA, Spiegel R, Kim U, Intussusception in adultsMt Sinai J Med 1999 66:336-40. [Google Scholar]
[14]. del-Pozo G, Albillos J, Tejedor D, Intussusception: US findings with pathologic correlation-the crescent-in-doughnut signRadiology 1996 199(3):688-92.10.1148/radiology.199.3.86379888637988 [Google Scholar] [CrossRef] [PubMed]
[15]. Yalamarthi S, Smith RC, Adult intussusception: case reports and review of literaturePostgrad Med J 2005 81(953):174-77.10.1136/pgmj.2004.02274915749793 [Google Scholar] [CrossRef] [PubMed]