Subcutaneous Phaeohyphomycosis Caused by Rhytidhysteron rufulum-A Case Report and Review of Literature
Mangaiyarkarasi Thiyagarajan1, Muthu Gopal2, Gopal Rangasamy3, Udhayasankar Ranganathan4
1 Associate Professor, Department of Microbiology, Sri Manakula Vinayagar Medical College and Hospital, Puducherry, India.
2 Scientist-C, Department of Microbiology, Model Rural Health Research Unit (NIEICMR/DHR), Linked to Tirunelveli Medical College, Primary Heal, Thirunelveli, Tamil Nadu, India.
3 Professor and Head, Department of Microbiology, Sri Manakula Vinayagar Medical College and Hospital, Puducherry, India.
4 Assistant Professor, Department of Microbiology, Sri Manakula Vinayagar Medical College and Hospital, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Udhayasankar Ranganathan, Department of Microbiology, SMVMCH, Madgadipet, Puducherry, India.
E-mail: drudhaysnkr@gmail.com
Rhytidhysteron rufulum, a melanized fungus, is usually considered as a saprophyte and human infections due to this fungus are rarely reported in literature. To the best of our knowledge, since 2008, only eight cases of human infections due to R. rufulum has been reported and all cases were exclusively from India. We, hereby, present a case of subcutaneous phaeohyphomycosis due to R. rufulum in a 55-year-old male from Puducherry (India) who presented with swelling over left leg for one year. The patient also suffered from diabetes mellitus, systemic hypertension and chronic kidney disease. The fungus isolated in culture was finally identified by molecular sequencing. With advances in molecular diagnostic techniques, many organisms which were traditionally considered as non-pathogenic are increasingly being recognised as human pathogens. Accurate identification of the organism is essential for effective treatment and hence, molecular diagnostic techniques should be applied where ever appropriate.
Molecular sequencing, Puducherry, Rare fungus, Rhytidhysteron
Case Report
A 55-year-old male, farmer by occupation, presented with a swelling over left leg for the past one year. He noticed that the swelling was slowly increasing in size over time and for the past 10 days, he also noticed some discharge from it. The patient could not recollect any history of trauma. He is a known diabetic and hypertensive for more than 10 years and also has chronic kidney disease for more than two years. He denied any history of tuberculosis.
On examination, there was an irregular swelling of size 2×1.5 cm over the antero-lateral aspect of the left leg, just below the knee. The swelling was multiloculated, non-tender, smooth to firm and was not fixed to the underlying structures. A thick and purulent discharge was observed from the swelling. No abnormalities were found in the examination of organ systems. All routine investigations, including complete blood count, random blood glucose, urine analysis were found to be within normal limits except for mildly elevated renal parameters. He was also found to be non-reactive for HIV.
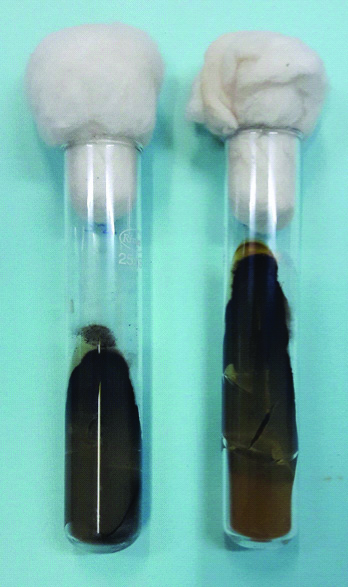
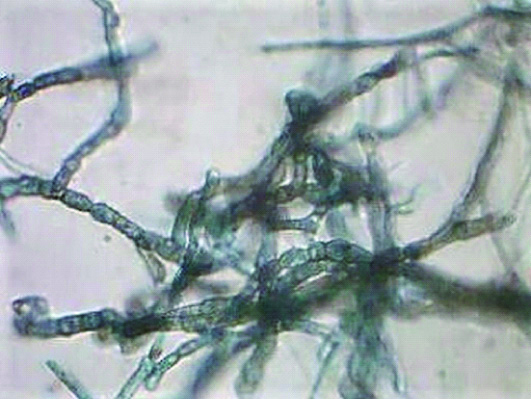
Aspirate from the swelling was received in the microbiology laboratory. The aspirate was thick, purulent and did not contain any granules. Gram stain, acid fast stain (Kinyon’s modification) and potassium hydroxide (KOH) mount were done. KOH mount showed thick, brown, septate and branching hyphae. No sclerotic bodies were seen [Table/Fig-1]. Gram stain did not show any organisms and the sample was also negative for acid fast bacilli. The sample was inoculated on multiple sets of Sabouraud’s dextrose agar with and without antibiotics and was incubated at 25°C and 37°C. Grayish black, velvety colonies [Table/Fig-2] with black reverse [Table/Fig-3] was observed after three weeks of incubation at 25°C. Teased, lactophenol cotton blue mounts of the growth showed brown coloured thick and septate hyphae but without spores [Table/Fig-4]. Repeated attempts to induce sporulation like, subculture on cornmeal agar and slide culture on potato dextrose agar were futile. Hence, the sample was sent for molecular identification to a private centre at Puducherry. The fungus was identified as Rhytidhysteron rufulum by partial sequencing of the 18S ribosomal RNA gene (Gen bank accession numbers: KP162180, KP162181). Unfortunately, further management was not possible since the patient did not return for follow-up visit.
KOH mount showing brown, septate, branching hyphae with sclerotic bodies absent (400X).

Growth on Sabouraud’s dextrose agar showing grayish black, velvety colonies on observe after 3 weeks of incubation at 25°C.
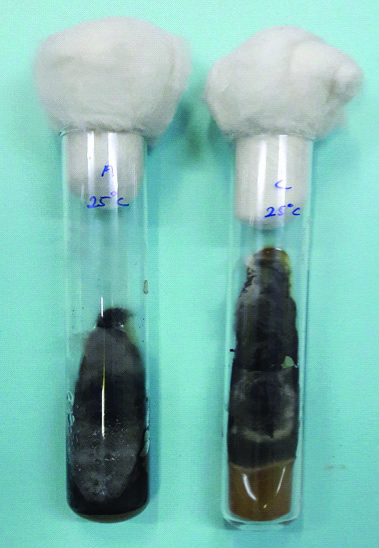
Sabouraud’s dextrose agar showing black pigment on the reverse.
Lactophenol cotton blue mount showing brown coloured, septate hyphae without spores (400X).
Discussion
Phaeohyphomycosis represents a heterogenous group of fungal infections characterised by the presence, either or a combination of dematiaceous yeast like cells, pseudohyphae or hyphae. It can be mainly classified as superficial, cutaneous, subcutaneous, systemic and corneal phaeohyphomycosis [1]. Contrary to the belief that these infections are common in immuno-compromised patients, many recent reports suggest that it can also affect immuno-competent individuals. Phaeohyphomycosis can be caused by the members of various genera like Alternaria, Bipolaris, Curvularia, Cladophialophora, Exophiala, etc., Rhytidhysteron is a phaeoid fungi which is usually considered a saprobe found in tropical and sub-tropical vegetations. The genus Rhytidhysteron, comprising the four species, R. rufulum, R. hysterinum, R. opuntiae and R. dissimile, is characterised by the production of septate ascospores and belongs to the family hysteriaceae [2]. Recently, subcutaneous infections due to this phaeoid fungus are being increasingly reported both in immuno-competent and immuno-compromised individuals. Till date, only eight cases of human infections due to Rhytidhysteron have been reported, all exclusively from India.
The case currently described is an elderly man who had co-morbidities like diabetes mellitus, systemic hypertension and chronic kidney disease. Old age, diabetes mellitus and renal disorders were observed as risk factors in the previous case reports [3-5]. Diabetes mellitus was observed as co-morbidity among two cases described by Mahajan V et al., and Tejashree A et al., [3,4]. The first case described by Chowdhary A et al., the only case recorded to have a fatal outcome, was a post-renal transplant patient [5]. All the other five cases reported were among immuno-competent individuals [6-9]. Seven of eight cases described were also found only in elderly men above 50 years of age. The case described by Mudhigeti N et al., is the only case report from southern India [9]. To the best of our knowledge, this is the second case of Southern India and the first case to be reported from the Indian union territory of Puducherry.
The disease is common among agricultural workers, where they sustain injury due to vegetative matter. Most cases reported, including the case being discussed, could not recollect any history of trauma suggesting that the disease can follow even after trivial injury.
The diagnosis of phaeohyphomycosis mainly relies on fungal culture and histopathology. But, molecular techniques like sequencing have proven to be of great value for the identification of non-sporulating fungi like Rhytidhysteron species, as seen in the previous reports where the final identification was achieved mainly by sequencing the ITS1 and ITS 4 regions [3-9]. In the index case, we identified the fungus by amplifying and partial sequencing the 18S rRNA region.
There are no clear guidelines for treatment of subcutaneous phaeohyphomycosis. All cases reported have received either itraconazole, amphotericin-B, terbinafine or a combination of them for treatment. The case described by Mahajan V et al., required intra-lesional amphotericin-B as it was not responding to itraconazole and the case reported by Tejashree A et al., was started on oral terbinafine and itraconazole [3,4]. Unfortunately, in the present case, the patient was lost to follow-up.
Conclusion
Rhytidhysteron rufulum over time, has established itself as pathogen and molecular diagnostic techniques are the key to identify this rare fungus. Since more number of cases are being reported, especially from India, further studies are necessary to study the ecology and pathogenicity of this fungus.
[1]. McGinnis M, Chromoblastomycosis and phaeohyphomycosis: New concepts, diagnosis, and mycologyJ Am Acad Dermatol 1983 8(1):01-16.10.1016/S0190-9622(83)70001-0 [Google Scholar] [CrossRef]
[2]. Murillo C, Albertazzi F, Carranza J, Lumbsch H, Tamayo G, Molecular data indicate that Rhytidhysteron rufulum (ascomycetes, Patellariales) in Costa Rica consists of four distinct lineages corroborated by morphological and chemical charactersMycol Res 2009 113(4):405-16.10.1016/j.mycres.2008.09.00318930137 [Google Scholar] [CrossRef] [PubMed]
[3]. Mahajan V, Sharma V, Prabha N, Thakur K, Sharma N, Rudramurthy S, A rare case of subcutaneous phaeohyphomycosis caused by Rhytidhysteron species: A clinico-therapeutic experienceInt J Dermatol 2014 53(12):1485-89.10.1111/ijd.1252924898242 [Google Scholar] [CrossRef] [PubMed]
[4]. Tejashree A, Suchetha C, Visakha K, Krishna Karthik M, A rare case of subcutaneous phaeohyphomycosis caused by Rhytidhysteron rufulumIndian J Microbiol Res 2017 4(4):468-70. [Google Scholar]
[5]. Chowdhary A, Guarro J, Randhawa H, Gené J, Cano J, Jain R, A rare case of chromoblastomycosis in a renal transplant recipient caused by a non-sporulating species of RhytidhysteronMed Mycol 2008 46(2):163-66.10.1080/1369378070163042018324495 [Google Scholar] [CrossRef] [PubMed]
[6]. Mishra K, Das S, Goyal S, Gupta C, Rai G, Ansari M, Subcutaneous mycoses caused by Rhytidhysteron species in an immunocompetent patientMed Mycol Case Rep 2014 5:32-34.10.1016/j.mmcr.2014.07.00225180152 [Google Scholar] [CrossRef] [PubMed]
[7]. Chander J, Singla N, Kundu R, Handa U, Chowdhary A, Phaeohyphomycosis caused by Rhytidhysteron rufulum and review of literatureMycopathologia 2016 182(3-4):403-07.10.1007/s11046-016-0064-x27628109 [Google Scholar] [CrossRef] [PubMed]
[8]. Yadav S, Agarwal R, Chander J, Chowdhary A, A rare case report of subcutaneous mycoses by Rhytidhysteron RufulumInt J Med Res Health Sci 2017 6(4):12-15. [Google Scholar]
[9]. Mudhigeti N, Patnayak R, Kalawat U, Yeddula S, Subcutaneous Rhytidhysteron infection: A case report from South India with literature reviewCureus 2018 10(4):e240610.7759/cureus.240629872587 [Google Scholar] [CrossRef] [PubMed]