Low back ache is a condition that affects all age groups. In fact, according to the 2010 Global Burden of Disease Study, low back pain is among the top 10 causes of the highest number of Disability-Adjusted Life Year (DALY) [1]. The lifetime prevalence of non-specific low back ache in developed countries is estimated to be in the range of 60-70%, with the largest number of cases occurring between 35 and 55 years of age [2]. Unfortunately, in developing countries, it is difficult to get a close estimate of prevalence of low back pain especially as it is not considered a major cause of disability leading to scarcity of data. In a meta-analysis on available literature regarding epidemiology of low back pain, Bindra S et al., found the prevalence ranging from as low as 6.2% to high as 92% depending upon the population under study [3].
One of the primary goals in the management of chronic low back ache is the temporary alleviation of pain. This enable the patient to engage in a physiotherapy and rehabilitation program aimed at improving strength to provide eventual long-term relief [4].
Even though the surgery is always a compelling option, selecting patients who are suitable candidates for surgery can be challenging and even in well-selected patients surgical outcomes may vary [5].
Amongst the multiple newer modalities of treatments available for managing chronic spinal pain, image guided interventions like perineural and facet joint steroid injection are fast emerging as a viable and minimally invasive alternative. Therefore, the present study was conducted with an aim to assess the efficacy of pain relief provided by CT guided perineural and CT guided facet joint steroid injections respectively in patients with chronic spinal pain.
Materials and Methods
This was a prospective study carried out over a period of 12 months from 01 January 2016 to 31 December 2016. This study conforms to widely accepted ethical principles guiding human based research. The institutional ethical committee approval for the study was taken (CHCC/IAC/2016/23). Patients with low back ache attending the neurosurgery centre were initially assessed by the neurosurgery team. Amongst these patients with neurological deficits who were surgical candidates were taken up for surgery. Non-surgical candidates were initially put on a conservative treatment regime including exercise, physiotherapy and lifestyle/posture modification.
All non-surgical candidates who failed to respond to conservative treatment even after a month of compliance were referred to the Interventional Radiology Department of command hospital for image guided interventions. Selected patients were examined to determine whether the backache was mechanical or neurological. Physical examination and review of MRI of the spine was done to localise the offending facet joint(s) and nerve root(s). As per institutional protocol, the patients were instructed to report back at 3 days, 30 days and 90 days for review. Patients who underwent these image guided interventions and reported back for review as per institutional protocol were considered for the study. Exclusion criteria included contraindication to local anaesthesia (allergy), steroids (diabetes or infection) and patients with tingling or numbness in the legs (as the perineural local anaesthesia may increase these symptoms). Also, patients who had not reported back for review and those with neurological deficits in the form of weakness or numbness in the lower limbs were excluded from the study.
Technique
Patients were placed in a prone position on the Computed Tomography (CT) gantry and a lateral scanogram was obtained.
For perineural injections, the scans were performed in the plane of the IV disc as determined by the scanogram. Facet joint injections were usually performed in the axial plane; however if evaluation of the axial scans suggested that an obliquity in the longitudinal plane would be helpful, scans were repeated in those angles.
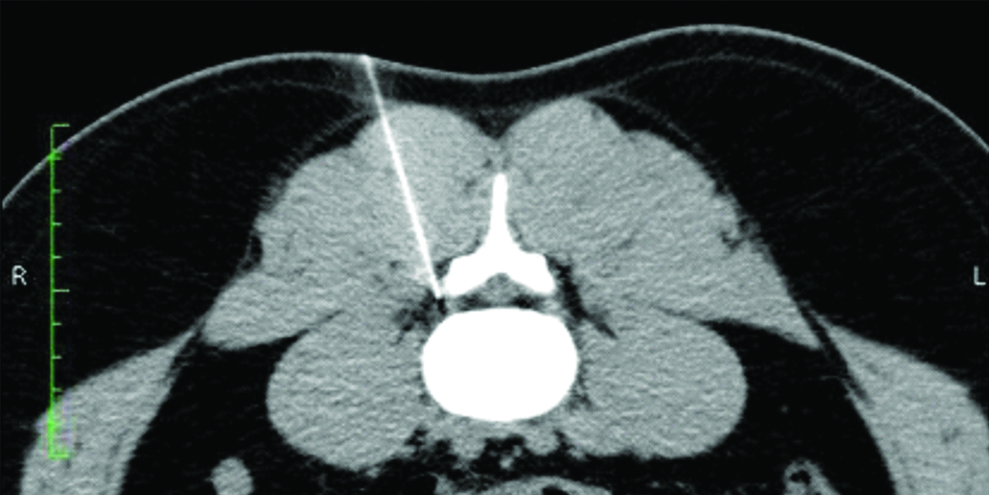
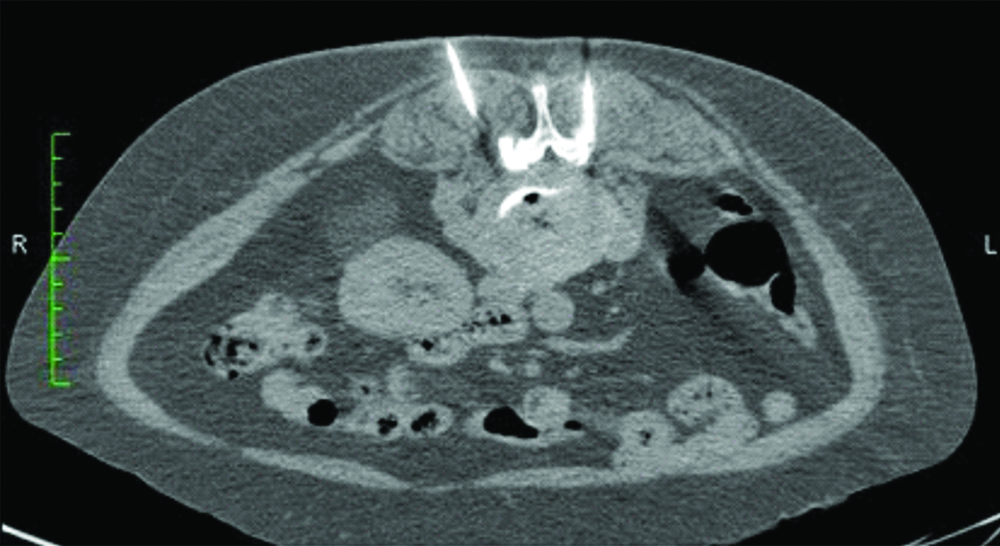
The local skin was cleaned and draped using standard surgical scrubbing techniques. A 3 to 5 mL of lignocaine 2% was used to anaesthetise the skin and underlying tissues using a 21G 1.5 inch needle and the needle left in place. If bilateral injections were planned, the local anaesthetic to the access site was given and needles left in place bilaterally. A check scan was then done to determine the correctness of the needle position and direction. Using these 1.5 inch needles as guide posts (to make any correction as calculated by the check scan), 23 G lumbar puncture needles were advanced till the neural foramen [Table/Fig-1]. A similar technique was used to reach till the facet joint space in cases of facetal arthropathy causing mechanical back pain [Table/Fig-2]. Position of the lumbar puncture needle was now confirmed using CT scan. Once the needle was confirmed to be in the satisfactory position, a mixture of 0.4 mL of 2% lignocaine, 0.6 mL of 0.25% bupivacaine and 80 mg of depomedrol was injected at this point. In case two injection sites were to be addressed, the depomedrol was divided so that the total dose did not exceed 80 mg.
Perineural steroid injection at L4-5 level in 30-year-old male patient with right sided sciatica.
Facet joint steroid injection in 65-year-old female with poorly localised chronic low back ache. The left needle is at the facet joint. The right sided needle was repositioned to target the facet joint.
Post Procedure
The patient was asked to wait in the CT scan centre for some 15-20 minutes. Most patients started experiencing pain relief within this time. Patients who received perineural injections were warned that their leg may feel numb for a few hours. All the patients were reviewed at 3 days, 30 days and 90 days.
Patient Assessment
For analysis each injection on each side and at each instance was calculated separately for pain relief. Patients were asked to grade pain on a VAS [6] for pain before the procedure as well as on subsequent reviews at 3 days, 30 days and 90 days. This pain score was used to calculate percentage of pain relief since previous follow-up and classified accordingly as follows:
<20% (none/minimal)
20-80% (moderate)
>80% (very good)
Statistical Analysis
The VAS date was tabulated and the serial change was noted. No statistical tools were used as the study merely analysed the subjective change according to VAS before and after the procedure as reported by individual patients. The date tabulation was done on MS Excel.
Results
A total of 75 patients reported for CT-guided perineural steroid injection for low back ache over the period 01 Jan 2016 to 31 Dec 2016. Of these 8 patients were excluded from the study due to exclusion criteria which were numbness in the lower limb and poorly controlled diabetes. Four patients did not report back and were lost to follow-up. The study group therefore included 63 patients who presented with sciatica that could be localised to a particular dermatome. Of these, 46 patients had pain at a single level while 4 patients had pain that could be localised to two levels. Out of 46 patients with single level involvement, 13 patients had bilateral sciatica.
Ten patients were taken up for CT-guided facet joint injection. Due to poor side localisation in mechanical low back ache due to facetal arthopathy, all these patients received bilateral injections. None of these patients was given injection again.
Since each injection on each side and at each instance was calculated separately, a total of 67 perineural injections and 20 facetal injections were administered [Table/Fig-3].
Number of Patients administered perineural/facet joint injection.
| Number of patients | Single level | Two level | Bilateral | Total injection sites |
|---|
| Perineural injection | 63 | 46 | 4 | 13 | 67 |
| Facet joint injection | 10 | 10 | Nil | 10 | 20 |
Pain relief after Perineural injection and after Facet joint injection on follow-up on day 3, 30 and 3 months is shown in [Table/Fig-4,5], respectively. All the patients had recurrence of symptoms and gave a history of none to minimal relief at 90 days post injection.
Pain relief after perineural injection.
| Number of days post-injection | None/Minimal (<20%) | Moderate (20-80%) | Very good (>80%) |
|---|
| 3 days | 13.4% (n=9) | 55.2% (n=37) | 31.5% (n=21) |
| 30 days | 20.9% (n=14) | 50.7% (n=34) | 28.3% (n=19) |
| 90 days | 65.8% (n=44) | 23.9% (n=16) | 10.4% (n=7) |
Pain relief after Facet joint injection.
| Number of days post-injection | None/Minimal (<20%) | Moderate (20-80%) | Very good (>80%) |
|---|
| 3 days | 40.0% (n=8) | 60.0% (n=12) | - |
| 30 days | 80.0% (n=16) | 20.0% (n=4) | - |
| 90 days | 100% (n=20) | - | - |
Discussion
Local steroid spinal injections performed either with or without fluoroscopy, are increasingly being used for the management of chronic low back pain [7]. An image-guided technique increases the precision of spinal injection procedures in delivering the medication in a targeted fashion, as close as possible to the area of pathology. This will not only maximises the therapeutic effect but also minimise the systemic side effects of corticosteroids [8].
Perineural injection given selectively around the affected exiting nerve is the most specific and targeted form of injection to achieve localised analgesia, however the only caveat with this technique is that its accuracy depends upon whether the involved nerve root is specifically determined by history or physical exam [9]. Facet joint injection is less selective, and may be used when a specific nerve root cannot be identified as the cause of the pain or in certain clinical settings which include strong clinical suspicion of the facet syndrome, focal tenderness over the facet joints, low back pain with normal radiological findings, post-laminectomy syndrome with no evidence of arachnoiditis or recurrent disc disease, and persistent low back pain after spinal fusion [10].
CT guided perineural and facet joint injections are generally deemed safe and are well tolerated by most patients. Complications have been reported relatively infrequently and are usually minor, most common of these comprise cases of facial flushing and vasovagal reactions occurring immediately after treatment and resolving rapidly with minimal supportive care. More serious complications like dural puncture with concomitant misadministration of the medication into the thecal space can occur, however these incidents are quite rare. Spinal cord infarction and paraplegia are extremely rare in association with lumbo-sacral perineural injection and are usually caused by inadvertent injection into a branch of the spinal artery [11].
Regarding complications arising from perineural injections in literature, Manchikanti L et al., [12] reported on 43,000 intermittent fluoroscopically guided facet joint nerve block injections performed during 7500 visits, and observed the following complications: Intravascular injection (11.4%), local bleeding (76.3%), oozing (19.6%), and local hematoma with profuse bleeding (1.2%) with less than 1% experiencing other notable complications. However, none of the patients in present study group suffered from complications related to the steroid injection.
To study the efficacy of lumbo-sacral spinal injections, Benny B and Azari P, carried out a meta-analysis reviewing the “best evidence-based literature” [13]. They included eight of ten randomised control studies and nine prospective trials and documented that image guided (CT or fluoroscopic guidance) lumbo-sacral transforaminal epidural spinal injection showed positive short- and long-term outcomes.
Roberts ST et al., also utilised multiple databases (Medline, Embase, Cochrane) to assess the efficacy of different types of spinal injections such as transforaminal epidural spinal injection, foraminal epidural spinal injection, selective nerve root block, nerve root injection, selective nerve root injection, periradicular infiltration, and periradicular injection for treating radicular pain [14]. They found that transforaminal epidural spinal injection was superior to placebo for treating radicular symptoms, and that injections could avoid surgery. They also discovered that transforaminal epidural spinal injections were superior to interlaminar epidural spinal injections and caudal epidural spinal injections for managing radiculopathy.
Schaufele MK et al., did a retrospective evaluation of pain resolution in the short-term and surgical requirements in the long-term for 20 patients undergoing fluoroscopically guided transforaminal epidural steroid injections vs. 20 patients undergoing fluoroscopically guided interlaminar epidural steroid injections [15]. Their study found that undergoing transforaminal injection experienced better resolution of pain, required fewer subsequent injections, and fewer subsequent operations.
The consensus-based guidelines for the pharmacological management of neuropathic pain given by Special Interest Group of the Canadian Pain Society say there is limited evidence regarding various selective transforaminal nerve root blocks. However, these procedures were found to provide up to eight to twelve weeks of relief from lumbar radicular pain. Thus, the task force recommended that these interventions be used with caution depending on the circumstances [16].
As far as studies regarding efficacy of facet joint injections, Civelek E et al., studied the effectiveness of lumbar facet joint injections vis-a-vis radio-frequency denervation in patients suffering from chronic low back pain and noticed that over short term, lumbar facet joint injection was more effective than radio-frequency [17]. Radiofrequency ablation has shown more satisfying results on an intermediate follow-up. They recommended that the first choice should be the facet joint injection and radio-frequency procedure should be used if the pain reccurs after a period of time. Other studies like the one by Datta S et al., noted that there was a level III (limited) evidence for intra-articular injections which was further reinforced by Falco FJ et al., [18,19].
In the present study also we observed that out of 67 perineural injections at least 31.5% reported very good pain relief as early as 3 days post-injection, while 28.3% continued to have very good pain relief even at the end of 30 days. However, at the end of 90 days, the number of patients with good pain relief fell to 10.4%. This is in consonance with findings in earlier reported studies.
Meanwhile, another 55.2% reported moderate pain relief at 3 days and about 50.7% and 23.9% continued to have moderate relief at 30 days and 90 days post injection respectively.
On the other hand only 13.1% of those given perineural injection had no or minimal pain relief at 3 days post-injection, however this figure subsequently increased to 21.1% at 30 days post injection and further to 65.8% at 90 days post injection. Thus even though perineural steroid injections provided short term relief in a significant number of patients, long term benefit was observed in a smaller percentage of patients. This observation can be compared to that of Benny B and Azari P, who found promising results in both short- and long-term outcomes with image guided transforaminal epidural spinal injection injections [13].
Out of 10 patients (20 injection sites) given bilateral facet joint injections, 60% gave history of moderate relief at 3 days post-injection and this figure came down to 20% at 30th day follow-up. At 90 days post injections, almost all patients had none or minimal relief as compared to pre-injection state. This conforms to previously published studies that found weak evidence for lumbar facet joint injection. In fact, two publications [20,21] that performed critical analysis of all available literature, found these injections were not clearly shown to be effective.
Our study confirms the efficacy of perineural injections in providing symptomatic relief to patients with chronic spinal pain. In our study, the efficacy of facet joint injections however was not as good as perineural injections.
Limitation
The skewed ratio of patients undergoing perineural injections compared to facet joint injections is one of the major limitation of present study which precludes any confident statistical analysis comparing their respective efficacies.
Conclusion
Lumbo-sacral perineural steroid injections provided excellent short term relief in patients with sciatica. Those not responding to conservative treatment and who are not ideal candidates for surgery, enabling the patient to engage in physiotherapy and rehabilitation programs leading to improved strength and provide eventual long-term relief. On the other hand, facet joint injections were not found to be efficacious in providing adequate pain relief in present study group. CT-guided perineural steroid injections can be incorporated into any existing interventional radiology practice. However, use of image guidance and adherence to proper technique along with appropriate patient selection is important to maintain a favorable risk/benefit ratio.