Hyperglycaemia is associated with poor outcomes and increased mortality in critically ill patients [1]. Hyperglycaemia influence the patients’ outcomes due to its suppressive effects on immune function, that increases the risk of infection, endothelial damage, mitochondrial damage in hepatocytes and tissue ischemia due to acidosis and inflammation [2]. Despite decades of research, the effect of IIT on ICU mortality rates and hypoglycaemia remains debatable [3]. Clinical trials on use of IIT have reported improved glycaemic control, and decreased mortality, organ dysfunction, and length of stay in the ICU in medical and surgical critically ill patients. On the contrary, some published data suggest that IIT neither benefits nor harms patients during cardiac surgical procedures or those recovering from cardiac arrest [4]. While intervention trials report improvement in patient’s outcomes, other studies reports that IIT is associated with increased risk of hypoglycaemia [5,6]. Regardless of the conflicting conclusions, American Diabetes Association (ADA) recommends intensive insulin therapy as the standard of care for critically ill patients [7].
Owing to the inconsistent results, the present study was designed to determine the effect of tight blood glucose via CIT and IIT on mortality rates in critically ill ICU patients.
Materials and Methods
The prospective observational study was conducted at Yenepoya Medical College and Hospital, Karnataka, India. The study was approved by the Institutional Ethical Committee (YEC-1/080). After obtaining informed written consent, 325 clinically diagnosed diabetic patients admitted in ICU from January 2018 to December 2018 were enrolled for the study. Sample size was calculated using G-power software with a level of significance, α=5%, and power of study, 1-β=80%.
Random Blood Sugar (RBS) and HbA1c levels during admission in ICU were measured. Age, gender, duration of DM, co-morbidities, SOFA score, APACHE II score, hypoglycaemia status, drug history, Acute Kidney Injury (AKI) and mortality were recorded for all study participants [8,9].
Capillary blood sugar was measured after every one hour using glucometer (Glucocard-Arkray Healthcare Pvt. Ltd., GT-1070). On ICU admission, patients were randomly assigned to Intensive Insulin Therapy or the Conventional approach by blinded envelopes. In the conventional group, continuous insulin infusion with 50 IU Actrapid HM (Novo Nordisk from Denmark) in 50 mL of 0.9% Sodium chloride (Perfusor-FM pump) was started when blood glucose levels rose above 215 mg/dL and was adjusted to maintain blood glucose levels between 180-200 mg/dL. For IIT, insulin dose was adjusted according to whole blood glucose levels, measured at 1- to 4-h intervals using glucometers. If the patient was hypoglycaemic, insulin administration was halted and DW 50% in the volume of (100-BS) × 0.4 mL was infused to the patient and sampling was performed every 30 min until he/she was euglycaemic. When patients were haemodynamically stable, feeding was started. Parenteral supplements were given to meet estimated caloric needs, when sufficient amount of calories could not be given enterally.
Statistical Analysis
Data obtained were presented as mean±standard deviation and percentage, and analysed using Statistical Package for the Social Sciences (SPSS) version 16. The primary study outcome was mortality. Independent student t-test was used for comparing mean changes between two parameters and ANOVA for comparison of changes between the groups in quantitative variables. Chi-square test was used for analysing qualitative variables between groups. A two-sided p-value <0.05 was considered as statistically significant.
Results
Age, gender, history of diabetes, co-morbidities, APACHE II score, SOFA score, hypoglycaemic episodes, mortality and the demographic characteristics of study participants are presented in [Table/Fig-1]. In 221 (68.2%) patients, a history of oral glucose control agents was noted. The patient population was predominantly men 210 (64.6%), 190 (57%) were older than 60 years. Most admissions in ICU were of Cardiac cause 146 (45.2%) and Stroke 98 (30.3%). The data sets for APACHE and SOFA were 98.72% and 99.52% respectively. APACHE II score for survivor and non-survivor was 18.2 and 28.2 respectively. SOFA score for survivor and non-survivor was 8.8 and 15.2, respectively. ICU mortality was 110 (33.8%) [Table/Fig-1].
Demographic characteristics of study population.
| Characteristics | n (%) | Survivors | Non-survivors |
|---|
| Number of patients | 325 | 215 | 110 |
| Males | 210 (64.6%) | 135 | 75 |
| Females | 115 (35.4%) | 75 | 35 |
| Mean age (years) | 64 (60-69) | 65 (58-68) | 65 (62-70) |
| APACHE score | 18.8 | 18.2 | 28.2 |
| SOFA score | 8.2 | 8.8 | 15.2 |
| Mean blood glucose (mg/dL) | 162.43 | 135.54 | 184.67 |
| HbA1C | 8%-9% | 6.5%-7.5% | 9.5%-10.5% |
APACHE: Acute physiologic assessment and chronic health evaluation score; HbA1c: Glycated haemoglobin; SOFA: Sequential organ failure assessment score
The most common reasons for ICU admission were cardiac causes, stroke, CKD, sepsis and Chronic obstructive pulmonary disorder COPD [Table/Fig-2].
Mortality outcomes of patients during ICU stay.
| Insulin treatment | n (%) | Intensive insulin therapy | Conventional insulin therapy | p-value |
|---|
| Death during ICU care | 110 (33.8%) | 30 | 80 | 0.005 |
| Death due to cardiac cause | 35 (10%) | 5 | 30 | 0.005 |
| Death due to stroke | 5 (1.5%) | 0 | 5 | 0.02 |
| Death due to CKD | 15 (4.6%) | 5 | 10 | 0.04 |
| Death due to DKA | 30 (9.2%) | 10 | 20 | 0.005 |
| Death due to sepsis | 15 (4.6%) | 10 | 5 | 0.03 |
| Death due to COPD | 10 (3%) | 0 | 10 | 0.02 |
Independent student t-test; *p <0.05 statistically significant, CKD: Chronic kidney disease; COPD: Chronic obstructive pulmonary disorder; DKA: Diabetic ketoacidosis
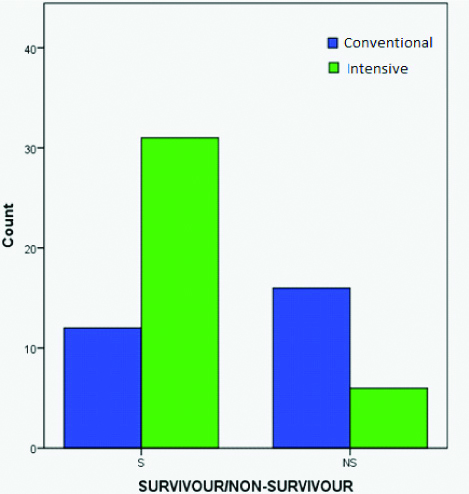
Mortality rate was significantly lower (p-value=0.005) in the Intensive Insulin Therapy group than in the conventional group [Table/Fig-3]. Hypoglycaemia occurred in 7 (2.2%) patients treated conventionally and 30(9.4%) patients treated with Intensive insulin therapy (p-value <0.0001). Risk of hypoglycaemia increased with lower mean blood glucose (3.1% at 140 mg/dL, 4.6% at 110-150 mg/dL, and 11.7% at <110 mg/day); p-value <0.0001. In 70% of the patients with hypoglycaemia, blood glucose was normalised (by stopping the insulin infusion and/or administering extra glucose) within 1 h and in all but two patients within 4 hour. In our study cause of death in non-survivors with previous history of diabetes was more of cardiac reasons in both Intensive and conventional group.
Glycaemic control of patients and Mortality outcome.
Discussion
Hyperglycaemia is commonly seen in critically ill patients, both with and without DM. Hyperglycaemia and concurrent insulin administration is associated with increased risk of death. Reduction of blood glucose levels with infusion of soluble insulin reduces mortality; but such a strategy is effective in certain selected groups of critically ill patients [10].
In the present study, mortality in the Intensive Insulin Therapy group was significantly lower than in the conventional group. Vanden Berghe G et al., in his study on 2,748 patients found that an intensive glycaemic control was important to bring down mortality and morbidity rates both in medical and surgical ICU patients [11]. Another study reported that IIT during intensive care prevent morbidity but does not reduce the risk of death in medical ICU population [12]. Reed CC et al., study reported that outcomes before and after using intensive glucose monitoring improves in mortality rate [13].
In contrast to present findings, NICE-SUGAR study reported that intensive glucose control increased mortality among adults in the ICU [14]. In another study groups on 537 patients with sepsis, no significant difference was observed in death rate in conventional blood sugar management versus IIT [15]. Oksanen T et al., reported that strict glucose control do not reduce mortality, and rather increases the incidence of hypoglycaemia in a group of patients treated to maintain blood glucose <108 mg/dL for 48 hours following cardiac arrest, in comparison with a group treated to maintain glucose <144 mg/dL [16].
An Action to Control Cardiovascular Risk in Diabetes (ACCORD) study showed that intensive blood glucose control may actually not be beneficial to the outcome of cardiac patients, and suggested that the results obtained were due to hypoglycaemia or weight gain or due to drug interactions [17]. Another study reported that intra-operative hyperglycaemia is an independent risk factor for complications in patients undergoing cardiac surgery [18]. On the contrary, preliminary results from Collier B et al., study showed no significant difference in mortality and increase in the risk of hypoglycaemia [19]. Literature suggests that hyperglycaemia independently affects length of hospital stay, infectious morbidity and mortality rate in trauma population [20,21]. These results, combined with data from the most recently concluded randomised trials, suggest that broad implementation of intensive insulin therapy may be needed and that additional randomised trials in diverse groups of critically ill patients are necessary.
Limitation
The study constituted of only medical ICU patients. Further studies on larger cohort comprising of mixed patient population such as cardiac, surgical and trauma are required to establish the results.
Conclusion
In conclusion, the results of present study support adoption of intensive insulin therapy in critical ill patients in ICU. In this study we observed that IIT in intensively ill patients was associated with a reduction in mortality in the hospital. Blood glucose maintained at <110 mg/day was more effective than at 110-150 mg/dL though it is associated with the high risk of development of hypoglycaemia.
APACHE: Acute physiologic assessment and chronic health evaluation score; HbA1c: Glycated haemoglobin; SOFA: Sequential organ failure assessment score
Independent student t-test; *p <0.05 statistically significant, CKD: Chronic kidney disease; COPD: Chronic obstructive pulmonary disorder; DKA: Diabetic ketoacidosis