Cryptococcus Infection and Lymphocytopenia: An Ill Defined Entity
Venkat Janardhan Rama Reddy1, S Brunda2, Amit Kulkarni3, BG Chenna Keshava4
1 Postgraduate Student, Department of General Medicine, Sagar Hospital, Bengaluru, Karnataka, India.
2 Postgraduate Student, Department of General Medicine, Sagar Hospital, Bengaluru, Karnataka, India.
3 Consultant Neurologist, Sagar Hospital, Bengaluru, Karnataka, India.
4 Consultant Neurologist, Sagar Hospital, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. BG Chenna Keshava, 1323, 7th Main 2nd Stage, WCR Mahalaxmipuram, Bengaluru-560086, Karnataka, India.
E-mail: ckeshava7@gmail.com
Cryptococcus neoformans infections are rare. Meningitis by Cryptococcus is well known as an opportunistic infection. It is most commonly seen in immuno-suppressed patients, especially in retrovirus infections and chemotherapy patients. Herein we describe a healthy adult male patient, with no known co-morbidities, who had Cryptococcus meningitis with associated very low CD4 count. We could not ascertain a reason for the low CD 4 count and hence was labelled as Idiopathic CD4 lymphocytopenia. Patient was successfully treated with amphotericin and discharged home.
CD4, Fungus, Idiopathic, Meningitis
Case Report
A 57-year-old male with no known co-morbidities, complained of on and off neck pain and fever for two weeks, worsening headache with vomiting since three days. The vomiting was projectile in nature and on the previous day he had vomited nearly 15 times. He was initially treated at a local hospital but with no improvement. His symptoms persisted and headache worsened, so he came to emergency room with family. He denied history of seizures, chest pain, fall, sleep disturbance, loose motions.
On physical examination, he was well-built and nourished appropriate for age. He was conscious, oriented and obeyed simple commands. His vitals were HR-72/min, BP-140/90 mm Hg, temperature-afebrile, GRBS -115 mg/dL. After the initial sampling in ER for CBC, RFT, Chest X-Ray, LFT, urine and ECG, patient was admitted to ICU (intensive care unit) for monitoring and care, with an admitting diagnosis of Neuroinfection (Bacterial vs Viral). His initial MRI and MR venogram was essentially normal. He was started on Acyclovir and Cephalosporins, with other supportive management.
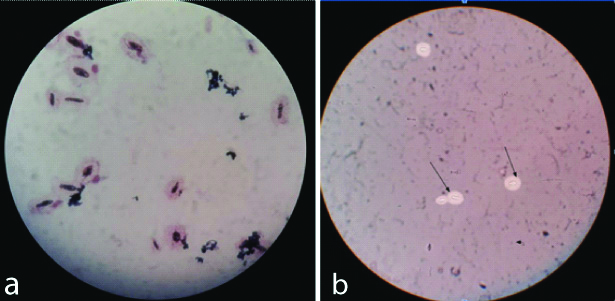
A lumbar puncture, done on Day 1, revealed a total cell count of 25 with lymphocyte (85%) predominance [Table/Fig-1]. Gram stain detected encapsulated yeast and India Ink confirmed presence of Cryptococcus neoformans [Table/Fig-2]. Patient was started on Liposomal Amphotericin at 3 mg/kg. A second set of investigations was sent to rule out an immunocompromised state which included HIV I & II, HbsAg, HCV & CD4/CD8 counts. His immune workup turned out to be negative and the CD4/CD8 was very low [Table/Fig-3] with a very total CD count of 89 cells/mcl.
Investigations done on subsequent days.
| Investigations | Day 1 | Day 3 | Day 15 | Day 30 | Day 45 |
|---|
| Haemoglobin (gm/dL) | 16.2 | | | | |
| PCV | 44 | | | | |
| TLC (cells/mm3) | 5800 | | | | |
| Platelet count(cells/mm3 | 202000 | | | | |
| Serum Creatinine(mg/dL) | 0.94 | | | | |
| BUN (mg/dL) | 22 | | | | |
| Sodium (mEq/l) | 133 | 133 | | | |
| Potassium (mEq/l) | 3.80 | 4.14 | | | |
| Chloride (mEq/l) | 102 | 106 | | | |
| CSF | Colourless, slight turbidity | | Colourless, clear | Colourless, clear | Colourless, clear |
| Cells | 25 (L85%, N15%) | | 146 (L 57%, N43%) | 60 (L65%, N 20%, E-15%) | 46 (L90%, N 8%,E-2%) |
| Protein (mg/dL) | 42.9 | | 57.5 | 97.8 | 60.7 |
| Glucose (mg/dL) | 61 | | 90 | 45 | 45 |
| Gram stain | Few pus cells, Yeast cells encapsulated yeast | | Few pus cells, Yeast cells encapsulated yeast | Few pus cells, No organism. | Mononuclear cells. |
| India ink | Cryptococcus | | Cryptococcus | Cryptococcus | Negative |
| Cryptococcal antigen | Positive | | Positive | Positive | Negative |
| Fungal C/S | Cryptococcu neoforman | | Cryptococcu neoforman | No growth | No growth |
a) Haematoxylin and Eosin; b) India Ink Stain (arrow mark indicate organism).
CD4/CD8 Absolute counts (Flow Cytometry).
| Test | Test result | Reference range |
|---|
| CD3 counts | 539 | |
| CD3 lymphocytes % | 71.29% | 60.5-76.9% |
| CD4 counts | 89.00 cells/mcl | Male-441-1295 female-1372 cells/mcl |
| CD4 lymphocytes % | 11.7% | 29.3-44.9% |
| CD8 counts | 299.00 | Male-326-763 cells/mclFemale-223-1103 cells/mcl |
| CD8 lymphocytes % | 39.59% | 25.2-42.8% |
| CD4/8 ratio | 0.30 | Male-0.74-2.58 Female-0.82-3.21 |
| TLC | 10283.00 | 4000-11000 Cells/cu.mm |
| Absolute lymphocyte count | 756.00 Cells/cu.mm | 1000-4000 Cells/cu.mm |
| Lymphocytes % | 7.35% | 20-45% |
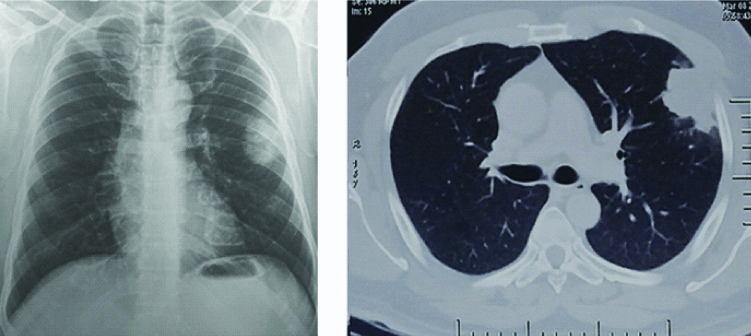
Over the next few days patient was symptomatically better and was shifted to ward, on Day 5 of hospitalisation. His initial chest radiograph showed a left uppersone coin lesion. A CT+PET CT showed a 3.6×3.5×3.6 cm metabolically active lobulated soft tissue density mass anterior segment of left upper lobe plus multiple metabolically active lymph nodes in the cervical, axillary, and bilateral iliac lymph nodes [Table/Fig-4]. Histopathology of the lesion was negative for malignancy and showed cryptococcus in the tissue. Other markers for malignancy (including lymphoma) were negative.
Chest X-ray (left image) with a solitary nodular lesion in left midzone and CT Chest (right image).
Patient continued to improve and was discharged on day 15 of hospitalisation with advice to continue Amphotericin for 6 weeks plus Flucytosine and regular follow-up on OPD basis. His follow-up lumbar punctures on Day 15, Day 30 and Day 45 showed gradual improvement, with complete disappearance of the organism on Day 45. His follow-up CD4 count 5 months later was 240 cells/mcl.
Discussion
Idiopathic CD4+T Cell Lymphocytopenia (ICL) is a rare and heterogeneous clinical syndrome. It is defined by persistent CD4+ T cell lymphopenia (<300 cells/microL) in the absence of infection with Human immunodeficiency virus (HIV)-1 or any other cause of immunodeficiency. Patients present with opportunistic infections, malignancies or auto-immune disorders. CD4+T cell counts should be below 300 cells/microL or less than 20 percent of total lymphocytes on more than one occasion, usually two or three months apart [1,2].
ICL is a rare condition, distributed worldwide, with no apparent gender predilection and distributed across all ages though in the beginning it was seen in adults. Initially, described in the year 1992, at the beginning of the HIV epidemic, following the recognition that people with suspected Acquired immune deficiency syndrome (AIDS). Though no causative agent has been identified, ICL is more prevalent among intravenous drug users and haemophiliacs [2,3]. Though there are multiple mechanisms proposed to explain the enhanced loss of CD4 that include increased activation, increased degradation or increased apoptosis, none are validated. ICL has anecdotal association with Immunoglobulin G4 (IgG4) multi-organ disease, systemic lupus erythematosus and certain other autoimmune conditions [4].
The majority of patients are symptomatic. In a retrospective review of 258 cases of ICL, most patients (88 percent) had one or more infections, malignancies were reported in 18.1 percent, and auto-immune disorders were reported in 14.2 percent [5]. The severity and type of infection depend on the level of immuno-suppression. Patients become infected with common pathogens, such as Human papillomavirus (HPV) and varicella-zoster virus, as well as opportunistic organisms, especially cryptococcus and mycobacteria. Cryptococcal meningitis was the most common presenting opportunistic infection. Other opportunistic infections, include pneumocystis jirovecii (carinii) pneumonia, aspergillosis of larynx, toxoplasmosis, histoplasmosis, hepatitis C, Epstein-Barr virus (EBV), Cytomegalovirus (CMV); especially retinitis. Malignancies associated with ICL are lymphomas of various types (NHL, Leptomeningeal, cerebral), Kaposi sarcoma and vulvar carcinoma. Auto-immune conditions particularly those involving skin and mucous membranes, have been associated with ICL. Reported ones are Idiopathic thrombocytopenic purpura, auto-immune haemolytic anaemia, sjögren’s syndrome, systemic lupus erythematosus, antiphospholipid antibody syndrome, polyarteritis/vasculitis, psoriasis, erosive lichen planus of the scalp, autoimmune vitiligo, behçet-like syndrome, vasculitis, thyroiditis and sclerosing cholangitis [5,6].
Consensus diagnostic criteria have not been formulated. ICL is a diagnosis of exclusion. There should be no other immunologic abnormalities and no infections attributable to the low CD4+ counts. There is no standard treatment or recommendation when it comes to monitoring for ICL. The standard antimicrobial prophylaxis below a CD4 of 200 cells/mcl is same as HIV. The long term prognosis is variable as it depends on the duration and severity of infection. In most of the published cases, the CD4 reduces and stabilises at a lower level [7].
The index patient had no co-morbidity, retrovirus infection work-up was negative and cryptococcus infection was confirmed by India ink and PCR. His ANA profile screening was negative and with no other obvious cause for cryptococcus infection and a low CD4 count, it was diagnosed as Idiopathic CD4 Lymphocytopenia (ICL).
Conclusion
All cases of uncommon infections or opportunistic infections in the absence of any obvious cause, a CD4 count work-up would be worthwhile in understanding this particular disease entity.
[1]. Unexplained CD4+ T-lymphocyte depletion in persons without evident HIV infection-United StatesMMWR Morb Mortal Wkly Rep 1992 41:541 [Google Scholar]
[2]. Spira T, Jones B, Nicholson J, Lal R, Rowe T, Mawle A, Idiopathic CD4+ T-Lymphocytopenia- An analysis of five patients with unexplained opportunistic infectionsNew England Journal of Medicine 1993 328(6):386-92.10.1056/NEJM1993021132806038093635 [Google Scholar] [CrossRef] [PubMed]
[3]. Gholamin M, Bazi A, Abbaszadegan M, Idiopathic lymphocytopeniaCurrent Opinion in Hematology 2015 22(1):46-52.10.1097/MOH.000000000000010225463685 [Google Scholar] [CrossRef] [PubMed]
[4]. Sonios DI, Falloon J, Bennett JE, Shaw PA, Chaitt D, Baseler MW, Idiopathic CD4+ lymphocytopenia: natural history and prognostic factorsBlood 2008 112(2):287-94.10.1182/blood-2007-12-12787818456875 [Google Scholar] [CrossRef] [PubMed]
[5]. Ahmad D, Esmadi M, Steinmann W, Idiopathic CD4 Lymphocytopenia: Spectrum of opportunistic infections, malignancies, and autoimmune diseasesAvicenna Journal of Medicine 2013 3(2):3710.4103/2231-0770.11412123930241 [Google Scholar] [CrossRef] [PubMed]
[6]. Régent A, Autran B, Carcelain G, Cheynier R, Terrier B, Charmeteau-De Muylder B, Idiopathic CD4 LymphocytopeniaMedicine 2014 93(2):61-72.10.1097/MD.000000000000001724646462 [Google Scholar] [CrossRef] [PubMed]
[7]. Duncan R, von Reyn C, Alliegro G, Toossis , Sugar A, Levitz S, Idiopathic CD4+ T-Lymphocytopenia-Four Patients with Opportunistic Infections and No Evidence of HIV InfectionNew England Journal of Medicine 1993 328(6):393-98.10.1056/NEJM1993021132806048093636 [Google Scholar] [CrossRef] [PubMed]