Introduction
Myiasis is a parasitic infection, which is infested in the skin by developing larvae (maggots). There are a variety of fly species (myiasis is Greek for fly) within the arthropod order Diptera. Their infestation in oral cavity is a rare condition.
Aim
To systematically analyse the data available on the oral Myiasis, its aetiology, clinical presentation including age, gender, location of lesion, various treatment modalities and preventive measurements.
Materials and Methods
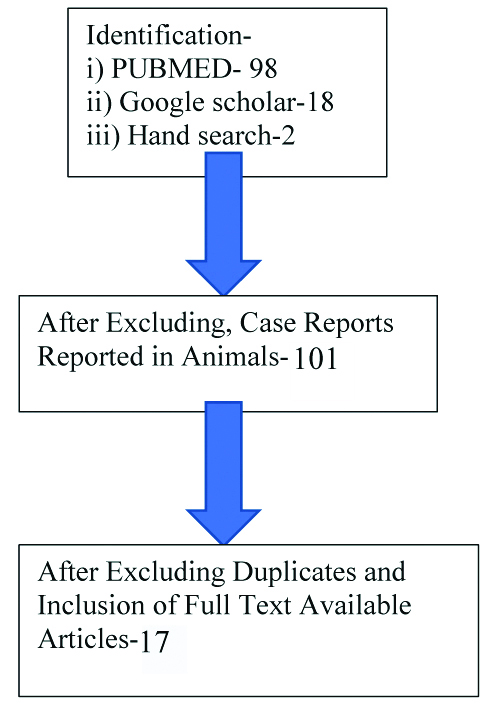
A systematic review of studies which included case reports on oral myiasis was included and a literature search was conducted using online databases (Pubmed and google scholar) along with hand-searching. Case reports and case series on oral myiasis, oral myiasis reported in humans, articles from 1980 to 2017, full text availability and text available in English language were the inclusion criteria. Review articles, oral myiasis reported in animals and text available in other language were excluded.
Results
A total of 98 articles from PubMed, 18 from Google Scholar, and 2 from hand search were identified. Out of 98 articles, 17 were shortlisted based on the inclusion criteria. Based on the analysis of collected data, gingiva of the anterior teeth and palate was the most commonly affected site with a male prediction and commonly seen between the age group of 20 to 40 years and was usually associated with patients presenting with CNS disorder.
Conclusion
Oral myiasis is relatively a rare entity of the oral cavity and only few cases have been documented till date. Hence, further documentation of cases is required to comment elaborately on the inherent susceptibility of individuals with similar condition and associated complications of the disease. And it is the role of the dentist to be aware of the condition and manage them accordingly.
Diptera, Ivermectin, Larvae, Maggots, Parasite
Introduction
Myiasis is defined as “infestation of live human and vertebrate animals with dipterous larvae that feed on the host’s dead or living tissue, liquid body substance or ingested food” by Zumpt in the year 1965 [1]. It is also defined as “any disease that results from the infestation of tissues or cavities of the body by larvae of flies” [1]. This condition was first described and termed by Hope FW in the year 1840. The term myiasis is derived from the Greek word “myi” meaning fly and “asis” meaning disease [2]. It is an infestation of skin caused by developing larvae (maggots) of variety of fly species belonging to the family Diptera [3]. The most common flies that are the basis of human infestation are Dermatobia hominis and Cordylobia anthropophaga [4]. The infestation ensues worldwide with seasonal variation, the prevalence of which is associated with the latitude and life cycle of the various species of flies. During their life cycle, human and animal tissue acts as an intermediate host. Its incidence is higher in tropics and subtropics of Africa and America [5]. It accounts for about 7.3% to 11%, usually one among the five most common dermatologic conditions [4]. The most commonly affected sites include skin, eyes, ears, stomach and intestinal tract or the genitourinary sites, other rarely affected uncommon site includes oral cavity [4]. There are many factors that predispose to myiasis which includes age, low socio-economic status, and medical comorbidities such as a history of cranio-maxillofacial trauma and malignant tumours. There are two main systems of classification i.e., anatomical and ecological. Anatomical is further divided into, Sanguinivorous or bloodsucking, cutaneous myiasis, furuncular and migratory, wound myiasis and cavitary myiasis. Ecological classification is sub-divided into specific or obligatory, semi-specific or facultative, accidental or pseudo myiasis [4].
Oral myiasis is a rare condition, which was first described by Laurence SM, in the year 1909 [6]. Since oral tissues are not permanently exposed to external environment, so the incidence is comparatively less as compared to cutaneous myiasis [5]. Oral myiasis is caused by flies larvae which belongs to either of the three families of Diptera, the Oestridae, Calliphordae and Sarcophagidae, which feed on dead and living tissues [7]. Most of them were described in developing countries and in the tropics. Oral myiasis can be of two types namely primary and secondary based on their order of occurrence i.e., infection involving palate or paranasal sinus etc., are considered to be primary and those which penetrate from the primary site and get lodged at a distant site is referred to as secondary. It is usually associated with poor oral hygiene, mouth breathing, anterior open bite, severe halitosis, alcoholism, neurological defect, patients under mechanical ventilation etc., [8]. Due to limited amount of cases reported in India and the availability of data is also limited when compared to myiasis associated with dermatological condition, this systematic review was carried out.
Overall, this review is an attempt to systematically analyse the data available on oral myiasis, its aetiology, clinical features including age, gender, location of lesion, various treatment modalities and preventive measurements.
Materials and Methods
This systematic review was carried out to identify all the available case reports and case series on oral myiasis. All the articles published from the year 1980 to 2017 were collected using the keywords “Diptera”, “Larvae”, “Maggots”, “Parasite”, “Ivermectin”. This search strategy was applied to key databases such as PubMed, and Google Scholar and the identified articles were independently reviewed by two reviewers, which was cross checked by the third reviewer. In addition, hand search of journals was completed for article retrieval. At this stage, all articles were collected and arranged chronologically. A total of 98 articles from PubMed, 18 from Google Scholar, and 2 from hand search were identified initially.
The articles were screened and selection of articles to be considered for review was based on inclusion and exclusion criteria.
Inclusion criteria:
Case reports and case series on oral myiasis;
oral myiasis reported in humans;
articles from 1980 to 2017;
full text availability; and
text available in English language.
Exclusion criteria:
Review articles;
oral myiasis reported in animals; and
text available in other language.
After close scrutiny of their abstract, excluding the duplicates and based on the inclusion and exclusion criteria, 17 articles were finally included in our study. All selected articles were reviewed in full text after gaining access.
Results
Based on the scrutiny of pre-existing records, the following articles were included in the study based on the inclusion and exclusion criteria [Table/Fig-1].
Inclusion and exclusion of the articles.
All the 17 case reports (18 cases) collected are summarised and tabulated in chronological order in [Table/Fig-2] [1,2,7,9-22].
Tabulated data of all the available case reports [1,2,7,9-22].
| S. No. | Patient age/sex | Country | Location of the lesion | Causative organism | Number of larvae present in the region | Associated disorder | Author, year and reference | Treatment |
|---|
| 1. | 42/Female | India | Anterior palate | Diptera | 10-12 | Neurological defect | Sharma J et al., 2008 [1] | Mechanical removal by administration of topical ivermectin. |
| 2. | 20/Female | Brazil | Gingiva of anterior teeth | Chochliomyiahominivorax | Multiple larvae | Hypotonic Cerebral palsy | Shinohara EH et al., 2004 [2] | Surgical debridement under local anaesthesia. |
| 3. | 34/Male | India | Anterior palate | Larvae | 55 | Neurological defect | Sharma N et al., 2014 [7] | Surgical debridement under local anaesthesia. |
| 4. | 69/Male | Israel | Gingiva of anterior teeth | Wohlfahrtia magnifica | 30 | - | Zeltser R and Lustmann J, 1988 [9] | Surgical debridement under local anaesthesia. |
| 5. | 24/Male | Brazil | Gingiva of anterior teeth | Sarcophagi | Multiple | - | Bozzo L et al., 1992 [10] | Surgical debridement under local anaesthesia. |
| 6. | 36/Female | Turkey | Gingiva of anterior teeth | Sarcophagi | Unknown | - | Günbay Ş et al., 1995 [11] | Mechanical removal under local anaesthesia. |
| 7. | 45/Male | India | Lip and floor of mouth | Musca domesticus | Multiple | Malnourished | Lata J et al., 1996 [12] | Surgical debridement under local anaesthesia. |
| 8. | 12/Male | India | In relation to 42,43,44 | Larvae of flies | - | Learning disability | Bhatt AP and Jayakrishnan AM, 2000 [13] | Mechanical removal under local anaesthesia. |
| 9. | 15/Male | China | Palatal aspect of upper right central incisor | Maggots | 100’s | Cerebral palsy | Ramli R and Rahman RA,2002 [14] | Surgical debridement under local anaesthesia. |
| 10. | 19/Male | India | Palatal region adjacent to left lateral incisor | Maggots | - | Cerebral palsy | Ramli R and Rahman RA, 2002 [14] | Mechanical removal under local anaesthesia. |
| 11. | 3/Male | Iran | Gingiva of anterior teeth | Oestrus ovis | 5 | - | Hakimi R and Yazdi I, 2002 [15] | Mechanical removal under local anaesthesia. |
| 12. | 26/Male | Turkey | Gingiva of anterior teeth | Calliphoridae | Greater than 10 | Mouth breather | Gursel M et al., 2002 [16] | Mechanical removal under local anaesthesia. |
| 13. | 66/Female | Brazil | Gingiva of anterior teeth | Chochliomyia hominivorax | 40 | - | Gomez RS et al., 2003 [17] | Surgical debridement under local anaesthesia. |
| 14. | 89/Female | Hong Kong | Gingiva of anterior teeth | Chrysomya bezziana | 7 | Pulmonary Tuberculosis | Ng KH et al., 2003 [18] | Mechanical removal under local anaesthesia. |
| 15. | 15/Male | Turkey | Aspiration fluid from oral cavity | Sarcophaga sp. | 3 | Tuberculosis Meningitis | Yazar S et al., 2002 [19] | Mechanical removal under local anaesthesia. |
| 16. | 19/Male | Israel | Gingiva of posterior mandible | Wohlfahrtia magnifica | 2 | - | Droma EB et al., 2007 [20] | Mechanical removal under local anaesthesia. |
| 17. | 40/Male | India | Anterior palate | Chrysomya benzziana | 6 | - | Aggarwal A et al., 2014 [21] | Mechanical removal under local anaesthesia followed by antibiotic therapy. |
| 18. | 40/Male | India | Ulcer in the left cheek region | Maggots | 15-20 | Mentally challenged with epilepsy | Saravanan T et al., 2015 [22] | Mechanical removal under local anaesthesia followed by ivermectin. |
The collected articles were analysed independently and their clinical features were summarised as follows,
Site: Gingiva in relation to anterior teeth and anterior part of the palate were the most commonly involved sites and the least involved sites were lip and floor of the mouth.
Gender: Among these 18 cases, 13 showed male predilection.
Age: It was more prevalent during second to fourth decade of life.
Distribution: Though worldwide in distribution, it is more predominantly seen in developing countries.
Associated disorder: Most of the patients presented with CNS disorders.
Number of larvae: The total number of larvae ranges from minimum of two larvae to maximum of hundreds of larvae.
Treatment: Surgical debridement under local anaesthesia.
Discussion
Myiasis is defined as “infestation of live human and vertebrate animals with dipterous larvae that feed on the host’s dead or living tissue, liquid body substance or ingested food” by Zumpt [1]. It usually presents with painful ulcers along with facial edge and fever. Few cases also present with a crawling sensation and smelly discharge. Myiasis is a condition which was first identified and coined by Hope FW in 1840 [2] and later described by Laurence in 1909 [6]. Methods of infestation in humans may occur in two ways, either due to accidental inoculation of fly directly or by ingestion of infected material such as meat [23]. In most of the above mentioned cases, the location was predominantly involving the anterior palate and anterior gingiva which suggest a direct inoculation of fly in these tissues. In few other cases, it showed other sites involving floor of the mouth, mandibular molar region etc., which shows to have a possibility of ingestion of food contaminated with eggs or larvae of varying species, as it would be difficult for the fly to infest the tissues of molar region directly.
Myiasis of oral cavity is usually caused by flies of the order Diptera. The number of species causing infestation of oral cavity depends on the geographical distribution of the Dipteran species [8]. The life cycle of all these species involves four stages namely egg, larvae, pupae and finally the adult fly. The larvae stage involves three sub stages namely, first, second and third instar stage termed as maggots during which it reaches 11 to 15 mm in diameter. After the third instar stage, the maggot usually burrows for pupation and after 5 to 15 days during summer they emerge as adult flies. The average life span of an adult fly may range from 1 to 3 months. In humans, female flies lay over 500 eggs directly over the diseased tissue, the eggs hatch in less than 1 week and the life cycle is completed in about 2 weeks. The larvae obtain their nutrition from surrounding tissues and burrows deeper by forming a track or a path separating muco-periosteum from bone. The three main families causing myiasis includes Calliphoridae, Sarchophagidae and Oestridae. Majority of these species are larviparous i.e. they produce their younger ones in form of larvae [4].
Myiasis is a worldwide phenomenon, the prevalence of which is linked to the latitude and life cycle of the species. It frequently affects the rural areas infecting live stocks and pets such as dogs and cats. It is extremely rare in Europe and countries in northern hemisphere and more common in tropics and sub tropics [20]. The tropical climate of Brazil favours the growth of larvae [6]. A high rainfall may facilitate the maturation of the pupae. The flies responsible for this condition prefer warm and humid temperature, therefore myiasis is restricted to summer months in temperate zones and all year round in tropics. Rise in global trade, immigration and global warming will also increase the likelihood of myiasis, causing the flies to migrate to native areas or areas where they have been eradicated. It is also called as “traveller’s disease” as it is most commonly seen in travellers returning from the tropics and sub tropics [7].
It occurs in patients with poor oral hygiene, ill-fitting dentures, uncleaned prosthesis, advanced periodontal disease, at tooth extraction sites, thumb-sucking habits, seizures and incompetent lips. Alcoholism, senility, mental retardation, hemiplegia and mouth breathing during sleep may facilitate the development of oral myiasis [8]. Review of the available literature showed that it was most commonly seen in patients who needed assistance and were not able to take care of themselves and patients with CNS disorders namely cerebral palsy, neurological defect, learning disability etc., were more commonly affected. Mental illness refers to a wide range of mental health conditions i.e., disorders that affect mood, thinking and behaviour. When the ability to do normal functions is lost it leads to serious mental illness which is the main cause for poor hygiene which eventually acts as a cause for myiasis.
A slight male predilection is observed, the reasons may include adverse habits like smoking, tobacco chewing etc. which leads to poor oral hygiene, sleeping outdoors and spending more time outdoors. It is not confined to any particular age, it may occur in both children and older adults. It most commonly affects the anterior part of the palate followed by gingiva, being the less commonly affected site.
The larvae can be identified only after its isolation from the affected site. This helps to plan the treatment and also to promote preventive measures [4]. After removal, the larvae should be killed by immersing it into a very hot but not boiling water for 30 seconds which prevents decay and helps to maintain the natural colour. Later, it should be preserved in a solution of 70 to 95% ethanol or 70% isopropyl alcohol [4]. The use of formalin is contraindicated as it causes the tissue to harden making them difficult to process. Identification is the most challenging and demanding task. So a Specific knowledge about the morphological aspects of the larvae is necessary for its identification, which is a task usually done by trained entomologist [4].
The treatment of choice includes mechanical removal or surgical debridement of the larvae under local anaesthesia followed by antibiotic therapy. Ivermectin, a semi-synthetic, anthelminthic agent for oral administration. It is a macrolide antibiotic which is derived from the avermectins, a class of highly active broad spectrum, anti-parasitic agent isolated from Streptomyces avermitillis. It was initially used as a prophylactic treatment for filariasis and also for the treatment of scabies. It is generally administered at a dosage of 150 to 200 mg/kg. The trade name for ivermectin is STROMECTOL. The possible undesirable effect may include dermal eruption, dizziness, fever, migraine, muscular and joint pain [4].
Measures taken to control the fly have emerged as an alternative strategy to prevent the infestation. Basic sanitation and eradication of foci of adult fly proliferation are the initial steps in prevention of this disease. Adequate sanitation can be reached only when government, population and education programs work together. The use of screens and mosquito nets is essential to prevent flies from reaching the skin. Usage of insect repellents containing DEET (diethyltoluamide) can also be an alternative method. Other general precautions include covering wounds, avoiding falling asleep outdoors etc., [4].
Conclusion
Oral myiasis is relatively a rare entity of the oral cavity with very few reported and documented case studies. Hence further documentation of cases is required to comment elaborately on the inherent susceptibility of individuals with similar condition and associated complications of the disease. The eyes does not see what the mind does not know. Hence, the dentists, as well as the general public, should be educated about the potential implications of the disease throwing light on prevention and treatment aspects. The importance of early diagnosis should be emphasised upon. Frequent educational programmes will enable reaching out to the general public. Oral myiasis as a potential health hazard must be documented and elaborated upon, for only sound knowledge will help eradication of this preventable but substantially grave and morbid condition.
[1]. Sharma J, Mamatha GP, Acharya R, Primary oral myiasis: A case reportMed Oral Patol Oral Cir Bucal 2008 13(11):E714-16. [Google Scholar]
[2]. Shinohara EH, Martini MZ, de Oliveira Neto HG, Takahashi A, Oral myiasis treated with ivermectin: Case reportBraz Dent J 2004 15:79-81.10.1590/S0103-6440200400010001515322651 [Google Scholar] [CrossRef] [PubMed]
[3]. Meinking TL, Burkhart CN, Burkhart CG, Changing paradigmsin parasitic infections: common dermatological helminthic infections and cutaneous myiasisClin Dermatol 2003 21:407-16.10.1016/j.clindermatol.2003.08.00414678721 [Google Scholar] [CrossRef] [PubMed]
[4]. Francesconi F, Lupi O, MyiasisClinical Microbiology Reviews 2012 25(1):79-105.10.1128/CMR.00010-1122232372 [Google Scholar] [CrossRef] [PubMed]
[5]. Bhola N, Jadhav A, Borle R, Adwani N, Khemka G, Jadhav P, Primary oral myiasis: a case reportCase Rep Dent 2012 2012:73423410.1155/2012/73423423125939 [Google Scholar] [CrossRef] [PubMed]
[6]. Laurence SM, Dipterous larvae infectionBr Med J 1909 9:88 [Google Scholar]
[7]. Sharma N, Malhotra D, Manjunatha BS, Kaur J, Oral myiasis-a case reportAustin J Clin Case Rep 2014 1(8):1039 [Google Scholar]
[8]. Lukin LG, Human cutaneous myiasis in Brisbane: a prospective studyMed J Aust 1989 150(5):237-40.10.5694/j.1326-5377.1989.tb136454.x [Google Scholar] [CrossRef]
[9]. Zeltser R, Lustmann J, Oral myiasisInt J Maxillofac Surg 1988 17:288-89.10.1016/S0901-5027(88)80004-3 [Google Scholar] [CrossRef]
[10]. Bozzo L, Lima IA, de Almeida OP, Scully C, Oral myiasis caused by Sarcophagidae in an extraction woundOral Surg Oral Med Oral Pathol 1992 74:733-35.10.1016/0030-4220(92)90399-B [Google Scholar] [CrossRef]
[11]. Günbay Ş, Biçakçi N, Canda T, Candaş ., A case of myiasis gingivaJ Periodontol 1995 66(10):892-95.10.1902/jop.1995.66.10.8928537873 [Google Scholar] [CrossRef] [PubMed]
[12]. Lata J, Kapila BK, Aggarwal P, Oral myiasis: a case reportInt J Oral Maxillofac Surg 1996 25(6):455-56.10.1016/S0901-5027(96)80083-X [Google Scholar] [CrossRef]
[13]. Bhatt AP, Jayakrishnan AM, Oral myiasis: a case reportInt J Paediatr Dent 2000 10(1):67-70.10.1046/j.1365-263x.2000.00162.x [Google Scholar] [CrossRef]
[14]. Ramli R, Rahman RA, Oral myiasis: case reportMalays J Med Sci 2002 9(2):47 [Google Scholar]
[15]. Hakimi R, Yazdi I, Oral mucosa myiasis caused by Oestrus ovisArch Iranian Med 2002 5(3):194-96. [Google Scholar]
[16]. Gursel M, Aldemir OS, Ozgur Z, Ataoglu T, A rare case of gingival myiasis caused by diptera (Calliphoridae)J Clin Periodontol 2002 29(8):777-80.10.1034/j.1600-051X.2002.290816.x12390576 [Google Scholar] [CrossRef] [PubMed]
[17]. Gomez RS, Perdigão PF, Pimenta FJ, Rios Leite AC, Tanos de Lacerda JC, Custódio Neto AL, Oral myiasis by screwworm Cochliomyia hominivoraxBr J Oral Maxillofac Surg 2003 41:115-16.10.1016/S0266-4356(02)00302-9 [Google Scholar] [CrossRef]
[18]. Ng KH, Yip KT, Choi CH, Yeung KH, Auyeung TW, Tsang AC, A case of oral myiasis due to Chrysomya bezzianaHong Kong Med J 2003 9(6):454-56. [Google Scholar]
[19]. Yazar S, Ozcan H, Dincer S, Sahin I, Vulvar myiasisYonsei Med J 2002 43(4):553-55.10.3349/ymj.2002.43.4.55312205748 [Google Scholar] [CrossRef] [PubMed]
[20]. Droma EB, Wilamowski A, Schnur H, Yarom N, Scheuer E, Schwartz E, Oral myiasis: a case report and literature reviewOral Surg Oral Ames Oral Pathol Oral Radiol Endod 2007 103(1):92-96.10.1016/j.tripleo.2005.10.07517178500 [Google Scholar] [CrossRef] [PubMed]
[21]. Aggarwal A, Daniel MJ, Shetty RS, Kumar BN, Sumalatha CH, Srikanth E, Oral myiasis caused by Chrysomya bezziana in anterior maxillaCase Rep Dent 2014 2014:51842710.1155/2014/51842724872898 [Google Scholar] [CrossRef] [PubMed]
[22]. Saravanan T, Mohan MA, Thinakaran M, Ahammed S, Oral myiasisIndian J Palliat Care 2015 21(1):9210.4103/0973-1075.15020025709196 [Google Scholar] [CrossRef] [PubMed]
[23]. McGraw TA, Turiansky GW, Cutaneous myiasisJ Am Acad Dermatol 2008 58(6):907-26.10.1016/j.jaad.2008.03.01418485982 [Google Scholar] [CrossRef] [PubMed]