Trauma forms a major cause of death and disability worldwide. According to the Global burden of disease study, injuries are responsible for 5.1 million deaths and 15.2% of disability adjusted life years lost. It is estimated that by the year 2020, trauma will be the third most common cause of death in the world [1]. A trauma system is an organised, coordinated system for the provision of trauma care to all the injured patients in a defined geographic area [2]. This system starts with pre hospital care and involves central ambulance dispatch centres, paramedical services etc., [3] and on reaching the trauma centre, ATLS principles laid down by the American college of surgeons are then followed. Proper training and implementation of these principles in trauma centres, can improve outcomes of trauma patients [4].
Then comes the role of various injury severity scores, which are the standardised tools to compare the severity and the clinical outcomes as well as for triage of trauma patients. Several trauma scores are used and are classified into physiologic, anatomic and combined anatomic and physiologic scoring system [5].
The Injury Severity Score (ISS) and the NISS are the anatomic scores. Both depend upon Abbreviated Injury Scale (AIS), but differ in the calculation methods. Most studies have shown that NISS is superior to ISS for evaluating injured patients [2,6-9] although some showed that they have similar accuracy [5]. RTS is the best and the most universally used physiological trauma severity scoring system. RTS system can allow rapid characterisation of neurologic, circulatory and respiratory injuries. However, RTS has been criticised as a mere triage tool [10].
Thus, this study was taken up with the objective to correlate various clinico-radiological parameters of the trauma patients and their trauma scores i.e., RTS and NISS and their outcome with respect to survival accordingly.
Materials and Methods
This comparative study was taken up at the Trauma centre, IMS, Banaras Hindu University after getting approval from the Institute’s Ethical Committee (Dean/2015-16/EC/1552). Sixty-one patients that met the criteria for polytrauma and gave informed written consent were selected for this study. Inclusion criteria was, patient with polytrauma and exclusion criteria were, age less down 14 and greater than 65, pregnant women with polytrauma, patients with pre-existing co-morbidities and patient with polytrauma that was brought in dead.
According to the international consensus on the term polytrauma- both anatomical and physiological parameters are included in its definition. It includes severely injured patients with associated injuries i.e., 2 or more severe injuries in at least two areas of the body and less often two or more severe injuries in a single body area. In this study, parameters studied included, demography of patients, mechanism of injury, Systolic Blood Pressure (SBP) Respiratory Rate (RR) and Glasgow Coma Scale (GCS). RTS and NISS were calculated for each patient at the time of arrival, at the time of intervention i.e. surgery and at the time of discharge. Finally, the patient outcome was compared on the basis of mortality and survival. ISS was calculated by giving each injury an AIS score. The highest AIS score in each body region was used. The AIS score of the three most severely injured body regions were then squared and added together to get ISS score (1-75). NISS was defined as the sum of the squares of AIS of the patient’s three most severe injuries, regardless of the body region in which they occurred. RTS aimed at identifying severity based on the SBP, the GCS and the RR. RTS score (0-12) was calculated as GCS value×0.9368+SBP value×0.7326+RR value×0.2908. Patients were divided into two groups i.e., those who died and those who survived [11,12].
Statistical Analysis
The statistical analysis was done using statistical software SPSS for windows (version 16). Chi-square test was used for non parametric variable, Student’s t-test was used for comparing two groups and one-way ANOVA test was used for multiple groups’ comparisons. A p-value <0.05 was stated as statistically significant. ROC curve was used as a tool for diagnostic test evaluation. In the ROC curve, true positive rate (sensitivity) was plotted in the function of the false positive rate (100-specificity) for different cut-off points of a parameter.
Results
In the present study, 61 patients were included and the mean age of presentation was 38.74±13.224 with male: female being 5.7:1. As per the outcome of the patients, 54 (88.5%) survived, while 7 (11.5%) died.
As is evident from the [Table/Fig-1], only ICU requirement showed a significant relation to mortality.
Comparison of various parameters with outcome.
| Survived | Died | p-value |
|---|
| Definitive airway | 4 | 2 | 0.077 |
| Intensive Care Unit (ICU) requirement | 6 | 6 | <0.001 |
| Hemothorax | 23 | 2 | 0.689 |
| Pneumothorax | 20 | 2 | 0.710 |
| Tension pneumothorax | 1 | 1 | 0.218 |
| Flail chest | 2 | 1 | 0.311 |
| Lung contusion | 9 | 0 | 0.580 |
| Blood transfusion | 34 | 6 | 0.40 |
| Focused Assessment with Sonography in Trauma (FAST) | 26 | 6 | 0.106 |
| Shock | 52 | 6 | 0.311 |
Findings in NCCT head could not establish a significant relation to the patient outcome according to this study [Table/Fig-2].
Non contrast CT head vs. outcome.
| Finding | Survived | Died | Inference |
|---|
| No head injury | 39 | 6 | χ2=0.624 |
| Brain Contusions | 14 | 1 | p=0.706 |
| Diffuse axonal injury | 1 | 0 | |
Out of all the patients with a positive finding in CECT abdomen, patients with both solid and hollow viscus injury had worse prognosis as compared to patients with either of them alone [Table/Fig-3].
Contrast enhanced CT abdomen vs outcome.
| CECT abdomen | Total (n=61) | Survived | Died | Inference |
|---|
| No finding | 29 | 28 | 1 | χ2=14.346a |
| Solid organ injury | 17 | 14 | 3 | p=0.081 |
| Hollow viscus injury | 12 | 10 | 2 | |
| Both solid and hollow viscus injury | 3 | 2 | 1 | |
Out of 61 patients, NISS at presentation of survived patients (17.39±6.614) and expired (26.29±4.990), with p-value <0.001 signifying that NISS value is a significant predictor of patients outcome [Table/Fig-4].
Comparison of various parameters with outcome.
| Variables | Mean±SD | t-value | p-value |
|---|
| Survived | Died |
|---|
| Age | 38.22±13.026 | 42.71±15.130 | -0.844 | 0.402 |
| Duration from injury | 8.7833±6.18387 | 6.2857±2.37236 | 1.052 | 0.297 |
| RR | 29.33±7.919 | 30.29±12.175 | -0.281 | 0.780 |
| Pulse | 107.93±16.271 | 108.57±26.063 | -0.092 | 0.927 |
| SBP | 96.15±13.861 | 82.57±15.131 | 2.415 | 0.019 |
| DBP | 59.70±11.409 | 52.57±13.100 | 1.532 | 0.131 |
| GCS presentation | 14.19±2.075 | 13.43±2.820 | 0.871 | 0.387 |
| GCS operation | 14.30±1.929 | 11.57±3.359 | 3.201 | 0.002 |
| GCS discharge | 15.02±0.495 | 15.00±.00 | 0.037 | 0.971 |
| SBP presentation | 96.00±13.753 | 82.57±15.131 | 2.405 | 0.019 |
| SBP operation | 108.56±6.412 | 96.67±8.165 | 4.197 | ≤0.001 |
| SBP discharge | 112.91±14.957 | 116.00±.00 | -0.205 | 0.838 |
| RR presentation | 29.46±7.630 | 30.29±12.175 | -0.250 | 0.804 |
| RR operation | 25.04±3.273 | 33.00±6.197 | -5.112 | ≤0.001 |
| RR discharge | 20.07±2.746 | 22.00±.00 | -0.695 | 0.490 |
| RTS presentation | 7.2504±0.73178 | 6.0990±1.23611 | 3.593 | 0.331 |
| NISS presentation | 17.39±6.614 | 26.29±4.990 | -3.424 | 0.001 |
| Hospital stay | 9.50±3.284 | 6.57±5.884 | 2.006 | 0.049 |
The [Table/Fig-5] shows the comparison of the mean scores in the survived patients at presentation and discharge. It shows the improvement in the NISS at the time of discharge while same is not true for RTS. Thus NISS is a better indicator of patient condition also.
Comparison of mean GCS, SBP, RR, RTS and NISS at presentation/operation/surgery.
| At presentation (1) | At operation (2) | At discharge (3) | p-value (1 vs 2) | p-value (1 vs 3) |
|---|
| GCS | 14.10±2.158 | 13.98±2.277 | 15.02±0.490 | 0.499 | 0.003 |
| SBP | 94.63±14.500 | 107.37±7.451 | 112.96±14.824 | ≤0.001 | ≤0.001 |
| RR | 29.92±7.709 | 25.83±4.322 | 20.11±2.733 | ≤0.001 | ≤0.001 |
| RTS | 7.1559±0.82933 | 7.5568±0.63020 | 7.8410±0.00001 | ≤0.001 | ≤0.001 |
| NISS | 18.23±6.944 | 18.33±6.896 | 17.59a±6.580 | 0.321 | - |
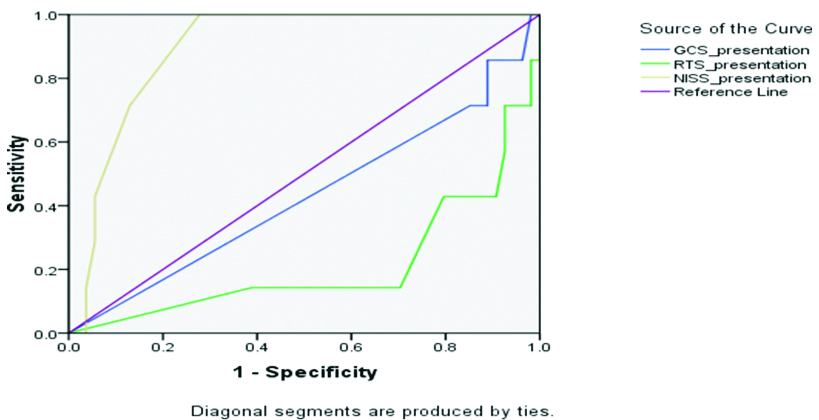
ROC shows that RTS was 85% sensitive and 100% specific with p-value being 0.014, while NISS was 100% sensitive and 73% specific with p-value being 0.001. Hence, NISS, carrying a significant p-value, was a more sensitive predictor for hospital stay, ICU requirement and mortality as compared to RTS, which in turn demonstrated a great specificity [Table/Fig-6].
 |
|---|
| Test result variable (s) | Area | Cut-off value | Sensitivity | Specificity | p-value | Asymptomatic 95% confidence interval |
|---|
| Lower bound | Upper bound |
|---|
| GCS | 0.430 | 6.0 | 100% | 100% | 0.549 | 0.189 | 0.671 |
| RTS | 0.212 | 4.5 | 85% | 100% | 0.014 | 0.008 | 0.416 |
| NISS | 0.896 | 20 | 100% | 73% | 0.001 | 0.812 | 0.979 |
Discussion
The present authors can finally infer from this study, that NISS which is an anatomical scoring system, is a better predictor of outcome in comparison to RTS, which takes into account the physiological parameters, in adult polytrauma patients.
Road traffic injuries are a leading cause of death in India [13]. Proper field triage along with a fixed trauma protocol for all the injured patients, tends to positively affect all the aspects of trauma care system [14]. A systematic approach was used for all the patients included in this study design i.e., preparation, triage, primary survey (according to protocols of ATLS), resuscitation, secondary survey (head to toe evaluation with history), continued post resuscitation monitoring and reevaluation and finally definitive care. Improved research is though, needed to assess the impact of such protocols for proper resource allocation, health care financing and funding and most importantly for patient outcomes.
Hueber Wegner S et al., found that Whole Body CT (WBCT) scan during trauma resuscitation is justified if performed quickly in a well structured environment and by a well organised team [15]. Moreover, given the low sensitivity, a negative FAST without confirmation by CT scan may result in missed intra abdominal injuries and thus should be reserved for haemodynamically unstable patients [16]. So, Contrast Enhanced CT chest and abdomen was done for all the study patients.
The task of incorporating various factors such as pre-existing morbidity, Age, Immunological differences and genetic predispositions into a scoring system, has made the prospectus of creating a universally acceptable and applicable trauma scoring system extremely arduous, if not impossible. Thus, the pre-existing comorbidities were kept in exclusion criteria of patients of this study.
On comparing the results of this study with the available literature, the present authors found that there have been some studies comparing two anatomical scoring systems [17,18] or two physiological scoring systems [19]. Fewer studies have been there comparing the two of them i.e., anatomical with physiological system [19-21]. There are hardly any studies, actually replicating the results of this study although, certain studies have given some conclusions which can be actually said to corroborate the results of this study. According to Jones JM et al., NISS was the strongest predictor of mortality out of all the variable that they tested for creating their own new trauma model i.e., NORMIT model [22]. Orhon R et al., determined that anatomical trauma scores predicted hospitalisation and ICU necessities better than the anatomo-physiological score i.e., TRISS model [23]. Dillon B et al., in their studies also concluded that on including a score, which takes into account body region locations of all injuries i.e., an anatomical scores gives better outcome prediction for trauma patients [24].
There were studies which also gave results contrary to the present study. Servia L et al., concluded that in trauma patients admitted to the ICU, the physiological models have some advances than the anatomical ones in terms of prediction of survival [20]. Soni KD et al., concluded that physiological based trauma scoring systems are much better predictor of in hospital mortality in comparison to anatomical based scoring systems for unintentional paediatric falls [21].
Limitation
The limitation of the present study is that it was conducted at a single centre and that too with a limited number of patients. To be able to generalise this finding, it would have to be tested in other groups of patients with a larger sample size.
Conclusion
According to this study, New Injury Severity Score (NISS) is a better predictor of outcome in comparison to Revised Trauma Score (RTS), in adult polytrauma patients, where the outcome is being measured by the survival rate. Hence, calculation of NISS should be included as a part of routine trauma protocol for all patients.