Meningitis is a significant cause of mortality and morbidity worldwide, especially in developing countries, even though there are advances in antibiotic therapy and vaccine application [1,2]. for efficient treatment and favourable outcome, rapid and accurate diagnosis plays a significant role. However, still differentiating Bacterial Meningitis (BM) from other types of meningitis, especially Tuberculous Meningitis (TBM) or Viral Meningitis/Encephalitis (VM/E) is a great challenge. Delay in distinguishing between bacterial, viral and tubercular meningitis and treatment may have serious consequences that lead to significant morbidity and mortality [3,4]. A number of biochemical markers of CSF like protein, glucose levels and leukocytes are routinely used to differentiate various types of meningitis. For BM, CSF examination is the gold standard test with an accuracy rates of 50%-90% with Gram staining and 70%-90% with CSF culture among untreated patients [3]. However, in clinical practice, CSF cultures are time-consuming. The major problem in this scenario is that the diagnostic yields of CSF Gram staining and subsequent culture in tertiary hospitals decrease significantly for the patients who have received empirical antibiotic pre-treatment, in a primary care setting or by self-medication, which is common, particularly in developing countries with severe antibiotic abuse [5]. Therefore, there is an urgent need for reliable tools to deal with the differential diagnosis dilemma in patients with suspected meningitis. CSF lactate level has been reported to be a potential marker to differentiate between bacterial meningitis from other types of meningitis [6]. CRP is an acute phase reactant. It is obvious that any inflammation in the body would lead to detection of CRP in serum or other body fluids associated with the affected tissues. Certain studies have reported that CSF C-reactive protein have high sensitivity and specificity in differentiating pyogenic meningitis from aseptic meningitis [7-9].
In view of such observations, the present study was conducted to find out the usefulness of these two tests, CSF-Lactate and CSF-CRP for the rapid diagnosis and differentiation of bacterial, tubercular and viral meningitis.
Materials and Methods
A cross-sectional study was conducted in Department of General Medicine and Department of Neurology at Malabar Institute of Medical Sciences, Kozhikode, Kerala, India, including 90 adult patients of age more than 15 years with clinical features of meningitis and abnormal CSF analysis for a period of 20 months (August 2014 to March 2016) while patients with seizures, recent stroke or brain trauma, patients with acute infections at sites other than the central nervous system, those in whom lumbar puncture was contraindicated and those with severe hepatic dysfunction were excluded from the study. Similarly, patients who received empirical antibiotics for meningitis prior to admission, those with fungal meningitis, patients on steroids and those with concomitant illness like HIV/on immuno-suppressive therapy were also excluded.
The study was approved by the Institutional Ethics Committee (IEC Reg. No. ECR/301/Inst/KL/2013) and informed consent was obtained from all patients. Sample size required for a sensitivity of 83% with an allowable error of 10% was 110 cases of meningitis. However, the authors could analyse only 92 patients during the study period. This was because the authors had to exclude patients with meningitis and seizures as it interferes with lactate levels.
History and clinical examination findings were recorded in a proforma. The patients were enquired about common symptoms of meningitis like fever, headache, vomiting, seizures, altered mental status and other relevant history like prior antibiotic intake, steroid intake, head trauma and other concomitant illness. CSF samples were collected after performing a lumbar puncture before starting any antibiotics. Estimation of CSF CRP was done using latex agglutination method. CSF lactate was assayed by means of lactate oxidase method. Depending on clinical features, investigations like CSF biochemistry, cytology, culture and other investigation, these patients were further divided into three groups.
Group I (BM group) was defined by clinical and CSF laboratory findings consistent with BM. Clinical features being the acute onset of symptoms of meningitis may be associated with sinusitis, otitis media and signs of meningeal irritation. CSF analysis showing Pleocytosis of >250 cells/mm3 predominantly neutrophils, Proteins >100 mg/dL, Sugar <40 mg/dL or CSF to serum glucose ratio <0.5, and Gram stain or culture positivity, neuroimaging showing evidence of contrast enhancement of the leptomeninges and abscesses or parameningeal focus.
Group II- Tubercular meningitis: This group included patients with clinical and CSF findings and neuroimaging consistent with TBM. Clinical features being the insidious in onset may be associated with tuberculosis of other organs, signs of meningeal irritation. CSF analysis shows Pleocytosis of >20 cells/mm3, predominantly lymphocytes, Proteins >100 mg/dL, Sugar <60% of blood sugar, Ziehl-Neelsen positive for acid fast bacilli. Neuroimaging shows evidence of meningeal enhancement, basal exudates and/or tuberculoma.
Group III-Viral meningitis: This group included Patients with clinical, CSF and laboratory findings consistent with VM. Clinical features are usually acute in onset with signs of meningeal irritation. CSF analysis shows pleocytosis of 5-500 cells/mm3, predominantly lymphocytes, Proteins 50-150 mg/dL, Sugar-normal.
Statistical Analysis
Data were analysed using SPSS version 17.0. Descriptive statistics is represented using mean with standard deviation or median with interquartile range for continuous variable. Categorical data were represented using frequency with percentages. Continuous variable between the groups were tested using ANOVA/Kruskal wallis test. Post-hoc Tukey test used for pair wise comparison. Sensitivity, Specificity and other statistical tools for diagnostic test is used to assess the performance of lactate level in differentiating meningitis types. For all test, p-value <0.05 is considered as statistically significant.
Results
During the study period, 90 patients were included in the study after obtaining the informed consent. There were 44 males and 46 females. Their age was distributed between 19 and 82 years with an average age of 47 years (SD=18). Depending on CSF cytology, protein and other parameters, 23 patients had bacterial meningitis, 26 patients had tuberculous meningitis and 43 patients had viral meningitis. Mean CSF cell count and mean CSF protein was highest in bacterial meningitis as shown in [Table/Fig-1].
Routine CSF analysis in different types of meningitis.
| Variables | Bacterial | TBM | Viral | p-value |
|---|
| CSF cell count (mm3)±SD | 3603±6776 | 184±160 | 146±197 | 0.003 |
| CSF Neutrophils % | 82±15.4 | 10±14 | 6.5±7.7 | <0.001 |
| CSF protein (mg/dL)±SD | 684±899 | 173.8±63 | 81±44 | <0.001 |
| CSF sugar (mg/dL)±SD | 39±19.1 | 52.6±22.4 | 68±19.3 | 0.16 |
The mean CSF lactate level was significantly raised in bacterial compared to tuberculous and viral meningitis (p<0.001) as shown in [Table/Fig-2].
CSF Lactate Levels in different types of meningitis.
| Variables | Bacterial meningitis | Viral meningitis | TBM | p-value* |
|---|
| Mean±SD | 10.67±6.19 | 2.84±1.03 | 4.46±1.86 | <0.001 |
| Median | 9.3 | 2.6 | 3.9 | |
| IQR | 10.3 | 0.60 | 1.68 | |
| Minimum | 1.4 | 1.6 | 1.6 | |
| Maximum | 22.5 | 7.9 | 8.1 | |
*Statistical analysis by one-way ANOVA
In a pairwise comparison, the mean CSF lactate in bacterial meningitis group differed significantly from both viral (p-value <0.001) and TB meningitis (p-value <0.001). However, mean CSF lactate did not differ between viral and TB meningitis.
The mean CSF CRP level in bacterial, tuberculous and viral meningitis was 4.44, 3.04 and 3.16 respectively [Table/Fig-3]. The difference was not significant (p-value 0.393). In a pairwise comparison, mean CSF CRP-value in bacterial meningitis did not differ from both viral and tuberculous meningitis.
CSF CRP levels in different types of meningitis.
| Variables | Bacterial meningitis | Viral meningitis | Tuberculous meningitis | *p-value |
|---|
| Mean±SD | 4.4±3.15 | 3.16±1.19 | 3.04±1.18 | 0.393 |
| Median | 3.3 | 3.28 | 3.28 | |
| IQR | 2.76 | 0.11 | 0.11 | |
| Minimum | 0.34 | 0.29 | 0.01 | |
| Maximum | 12.7 | 5.90 | 5 | |
*Statistical analysis by One-way ANOVA
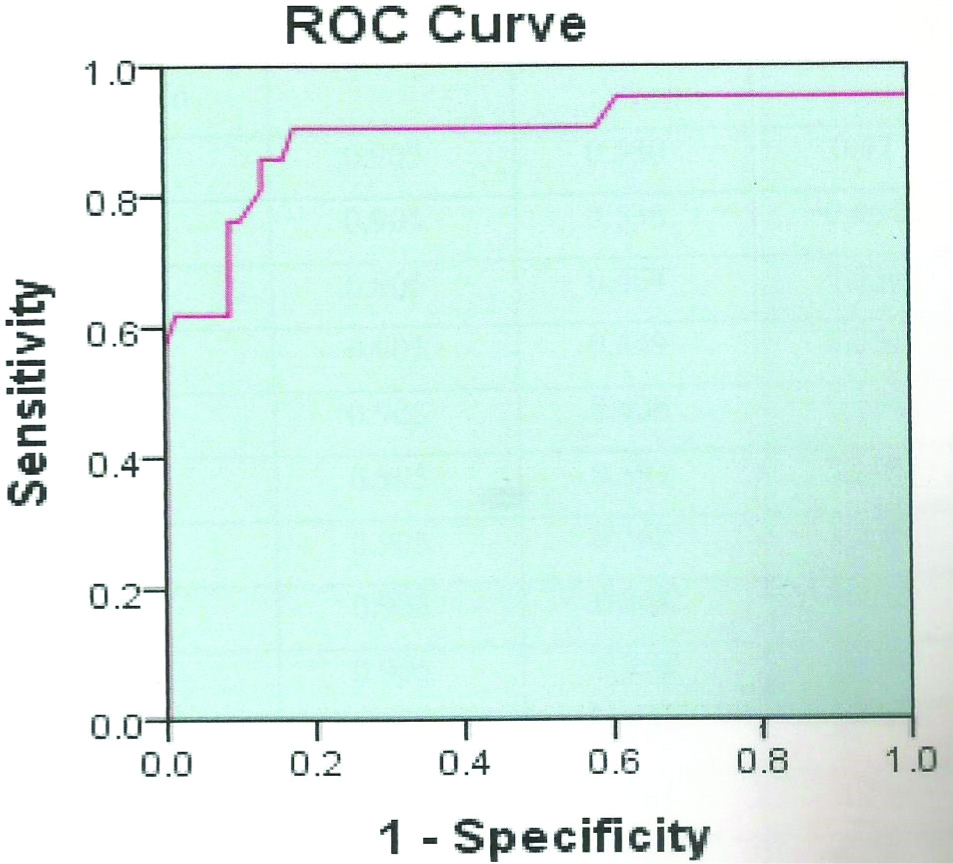
At cut-off level of 4.5 mmol/L, the sensitivity and specificity of Lactate for BM was 90.5% and 82.6% respectively. A very high negative predictive value of 96.6% was seen. It indicates that if lactate levels are <4.5 mmol/L, the probability of being bacterial meningitis is negligible. An ROC curve for CSF lactate was plot and area under the curve value of 0.892 was obtained [Table/Fig-4].
ROC Curve for CSF lactate.
Discussion
It was found that CSF lactate was the best single biomarker with an AUC of 0.892 on ROC curve, suggesting a very high diagnostic accuracy. This is in line with the two meta-analyses that reported high diagnostic accuracy of CSF lactate [10,11] but in contrast to older studies not finding a significant diagnostic ability [12,13].
Measuring CSF lactate levels may be helpful in diagnosis of bacterial meningitis, because CSF lactate concentration is dependent on CNS glycolysis. It was also found that lactate concentration increases proportionally to the number of inflammatory cells in CSF [14]. A lactate concentration of 4.2 mmol/L accurately predicted 24 out of 25 bacterial meningitis as per literature [15]. Unlike glucose, CSF lactate typically remains elevated for a significant time even after appropriate therapy is initiated. This may help in diagnosing bacterial meningitis in which antibiotics had been given already [16]. Limitation of CSF lactate is that it may increase in case of cerebral haemorrhage, malignant hypertension, hepatic encephalopathy, diabetes mellitus and hypoglycaemic coma [17]. Another study reported a D-lactate level of 0.15 mM has high sensitivity and specificity in patients who have partially treated bacterial meningitis [18].
In the current study, there was a significant difference in the average lactate level among different types of meningitis with p-value of <0.001. CSF lactate level was significantly raised in bacterial meningitis with mean value of 10.67. The present authors found that mean CSF lactate in the bacterial meningitis, group differed significantly from both viral meningitis (p-value <0.001) and TB meningitis (p-value <0.001). This is comparable with previous studies [19,20]. In a study done by Cameron PD et al., CSF lactate level was significantly raised in bacterial meningitis (mean 6.5, range 4.5-10.2) [19]. Another study by Curtis GD et al., observed that in 109 patients of proven bacterial meningitis the mean lactate concentration was elevated (over 2.8 mol l-1) in all cases [20]. In current study, it was also observed that at a cut-off level of 4.35 mmol/L, CSF lactate level can differentiate bacterial from non-bacterial meningitis with a sensitivity of 90.5%, specificity of 82.6%, positive predictive value of 61.3% and negative predictive value of 96.6% with overall accuracy of 84.4. Study by Viallon A et al., by taking a cut-off CSF lactate level of 3.8 mmol/L showed a sensitivity of 94%, specificity of 92%, negative predictive value of 99%, and positive predictive value of 82% for lactate which is comparable with the present study [21]. Sakushima K et al., and Huy NT et al., and one including 31 studies with 1885 patients and the other having 25 studies with 1692 patients showed sensitivities of 97 and 93% and specificities of 94% and 96%, respectively, in differentiating bacterial from aseptic meningitis [10,11]. In a recent study by Giulieri S et al., about community acquired bacterial meningitis which included 61 patients, came to conclusion that CSF lactate had a best accuracy for discriminating bacterial from viral meningitis with 100% sensitivity and specificity (cut-off value of 3.5 mol l-1) [22]. A very high negative predictive value of 96.6% was seen at a cut-off level of 4.5 mmol/L in current study, which indicates that at a lactate level of <4.5 mmol/L, the probability of being bacterial meningitis is negligible.
As per published data, in concentrations above 10 mg/dL, CSF CRP is quite sensitive for differentiating bacterial from viral meningitis [7]. CRP response is normal in viral meningitis as per literature [23]. Blood CRP is not specific and it can increase in other inflammatory and necrotic conditions. In current study, bacterial meningitis had a mean CRP-value of 4.44. Lowest CRP-value was 0.34 and highest value was 12.7. The mean value of CRP was almost comparable in different groups of meningitis. Using statistical methods like one-way anova and post-hoc tukey test, the present authors could not find any significant difference in mean value of CRP in bacterial meningitis when compared with other meningitis types like viral meningitis (p-value=-0.182) and tuberculous meningitis (p-value=0.191). So CRP is not a good marker to differentiate bacterial meningitis from viral/TB meningitis cases based on available data from current study. Many earlier studies suggested CSF CRP as a useful marker in differentiating bacterial meningitis from other non-bacterial meningitis [23,24]. A meta-analysis of 24 studies concluded that a negative CRP test can actually rule out bacterial meningitis with sensitivity ranging from 18-100% and specificity ranging from 75-100% [7]. Rajs G et al., observed that CSF-CRP levels were higher in gram negative bacterial meningitis because gram negative organisms cross blood brain more easily [9]. In literature, most of the studies conducted with regard to CSF CRP had a few number of bacterial meningitis patients. In many of the previous studies, gram negative bacteria were the common isolate, as per literature CSF CRP will be elevated in gram negative meningitis compared to gram positive cases [9]. This may be the reason for getting a high mean value for CRP and statistical significance in those studies [25]. In current study, the authors had 21 cases of bacterial meningitis and isolates were all gram positive strains, except for 1 (E.coli) leading to low mean value of CRP and less significance in differentiation from non-bacterial meningitis. Thus, it is evident that neither CSF lactate level nor CRP level alone could differentiate these three types of meningitis completely. However, their simultaneous use along with other tests of meningitis may be helpful in differential diagnosis of these three meningitis.
Limitation
The main limitation of this study is the small sample size. Further studies with larger sample size are needed in this regard.
Conclusion
This study concludes that Lactate levels in CSF along with other CSF differentials can be used for early differentiation of bacterial, viral and tuberculous meningitis. This is necessary when gold standard test for meningitis like Smear and/or culture for AFB, smear and/or culture for bacteria is not available or negative or time consuming. These tests can help in early diagnosis and prompt treatment which can bring down the mortality and morbidity of patients with meningitis and reduces unwanted or harmful therapy.
*Statistical analysis by one-way ANOVA
*Statistical analysis by One-way ANOVA