Hypertension (HT) poses significant cardio-vascular burdens globally. World Health Organisation (WHO) terms HT as an important risk factor for premature death globally [1]. Global Burden of Disease study (GBD) in its report reveals that high SBP is accounting for 10.2 million deaths and 208 million disability adjusted life years (DALYs) in 2017 [2]. HT is the most important risk factor in India in causing deaths and disability [3]. Many recent systemic reviews have found that HT prevalence in India is 25% to 30% in urban and 10% to 20% in rural adults [4,5]. Of late, prevalence of HT has started to rise in rural areas of India. One of the major Meta-analysis on prevalence of HT was performed by Anchala R et al., and it shows that its prevalence is 29.8% in India, which is quite high [5].
The importance of non-pharmacological treatment of HT is highly sought as adjuncts to drug therapy in the effective management of HT. According to American Heart Association (AHAs), non-pharmacological therapy is preferred for adults with stage I HT with no elevated Cardio-Vascular Disease (CVD) risks [6,7]. Similarly in Stage I with elevated CVD risks and for Stage II HT, non-pharmacological interventions are encouraged along with medications to manage raised BP efficiently. Even a small reduction in BP is associated with a reduced risk of CVD [8]. One such approach that has to gain attention in recent times in slow breathing.
Slow breathing has multiple physiological benefits like enhancing slowly adapting pulmonary stretch receptors and baroreceptors [9], reducing sympathetic nervous system activity [10] and chemo-receptor activator [11]. Recently, it was found that slow breathing has a role in long-term regulation of BP by lowering partial Pressure of arterial CO2 (PaCO2) thereby preventing renal retention of sodium [12].
In HT, the efficiency of slowly adapting pulmonary stretch receptors is reduced due to suppressed breathing and an accompanying rise in PaCO2 [13]. It was demonstrated that hypocapnia increased forearm blood flow and reduces vascular resistance of the forearm and brachial block does not prevent the flow [14]. This shows the positive influence of low PaCO2 on blood vessels. However, only few studies [12,15] have examined this relationship. Therefore, the purpose of the present investigation was to find out the immediate efficacy of SB in controlling BP as well as to study its influence on EtCO2 of HT patients.
Materials and Methods
Open Randomised control trial-parallel group study was conducted at medicine out patient department of Rajah Muthiah Medical College Hospital (RMMCH), Annamalai University between August 2016 to January 2017 (6 months). Ethical clearance was obtained from Institutional Human Ethics Committee (IHEC). The reference number is IHEC/0150/2016. Informed consent was obtained from the study population before enrolling them into the study procedure.
Sample Size
Sample size was estimated with confidence interval of 99%, (α=2.57) power of 90% (β=1.28), standard deviation (σ) of 5 with clinically significant difference of 6, which was based on the previous studies of similar kind [9,12]. The estimated sample size was 20 in each group.
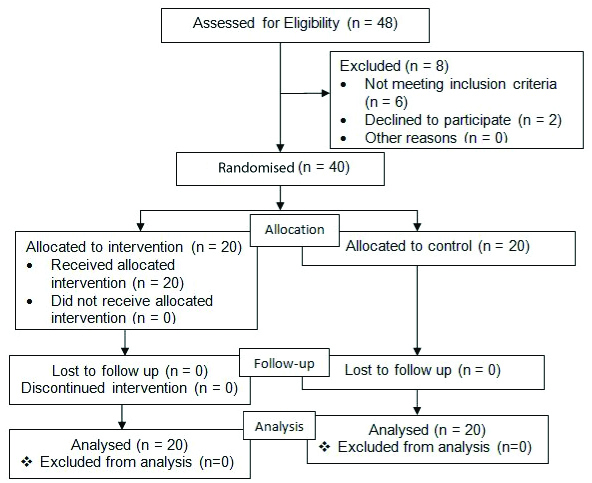
A total of 40 hypertensive patients were chosen and were randomly assigned to either study or control group [Table/Fig-1]. Block randomisation was used for allocation procedure. The block size was 4 and hence allocation was done in six ways. The allocation procedure was carried out by the third person.
Flow Chart – Allocation Procedure.
Selection Criteria
Joint National Committee 7 (JNC-7) classification [16] of pre- and stage IHT (120-159 mmHg)/(80-99 mmHg) were only chosen as they were best suited for non-pharmacological therapy. The subjects’ age range between 30 to 60 years and both the genders were included. For those on medications, Ca channel blockers alone were chosen to prevent the drug influence on autonomic nervous system.
Intervention
The study purpose and procedure was explained to each patient. They were told to relax in a chair for 15 minutes before pre-evaluation of outcome measures. Henceforth, study group were instructed about Slow breathing training and a prior training was given to make sure that there were no flaws in the technique. Slow breathing training consisted of 4 seconds of inspiration and 6 seconds of expiration. Therefore, breathing rate was reduced to 6 breaths/minute. The practice was given for 30 minutes [9,12,17]. Recorded auditory command of inhalation and exhalation was used as the instruction for practising breathing training [17]. The repeated, constant recorded voice was for 30 minutes. For control group, no breathing training was provided.
Outcomes
Blood pressure: The BP was recorded in an arm supported sitting thrice using Omron digital BP apparatus with an interval of 5 minutes. The average of last two measures was considered as final BP reading [18].
End tidal CO2: EtCO2 was measured using EMMA(R) emergency capnograph which uses infra-red mainstream technology to determine EtCO2 as well as respiratory rate [12,19,20]. Patient was told to breathe normally for a few breaths untill the values were displayed on the screen. The measurement was carried out for three times and an average of last two measures was taken as final readings.
Pulse rate: Pulse rate was monitored by hand-held pulse oximetry [21].
The outcome measures were evaluated at baseline and 30 minutes following breathing practices in study group. In control group, post monitoring was performed following 30 minutes of relaxed sitting [9,12]. Special care was taken as the precautionary measures to avoid breath holding during the SB. Special instruction was given about this during the practice session. In case, if the patients were not followed up the sequence of breathing instruction, they were advised to do normal breathing for few times until they were coming back to rhythm of breathing instructions. Control groups were not engaged in SB, instead they were told to relax in a back supported chair for a period of 30 minutes. They were advised to do normal breathing during the stipulated time. No emphasise was given regarding SB.
Statistical Analysis
Baseline characters of the study groups were compared for homogeneity using independent sample t-test. Same group before and after comparison of outcomes was carried out by the paired sample t-test as the variables were continuous in nature. Between group comparison of outcomes (Mean difference of pre-post values) was carried out by independent sample t-test. The entire statistical work was carried out by Statistical Packages of Social Sciences (SPSS-21.0).
Results
The nature of the study population is presented in [Table/Fig-2]. It is inferred that two groups were homogeneous at the baseline.
The basic characteristics of the study population.
| Variables | Study | Control | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| Age (years) | 45.10 | 8.25 | 42.20 | 9.23 | 0.341 |
| Gender (Male/Female) % | 65/35 | 60/40 | 0.799 |
| BMI | 24.78 | 2.91 | 25.57 | 2.58 | 0.369 |
| Systolic BP (mmHg) | 145.65 | 8.78 | 144.50 | 9.29 | 0.690 |
| Diastolic BP (mmHg) | 95.55 | 8.95 | 91.65 | 4.79 | 0.094 |
| PR (Beats/minutes) | 84.55 | 8.06 | 86.25 | 9.77 | 0.552 |
| RR (breaths/minutes) | 17.06 | 2.61 | 16.30 | 1.75 | 0.263 |
| EtCO2 (mmHg) | 31.80 | 2.50 | 33.50 | 3.12 | 0.064 |
SD: Standard deviation
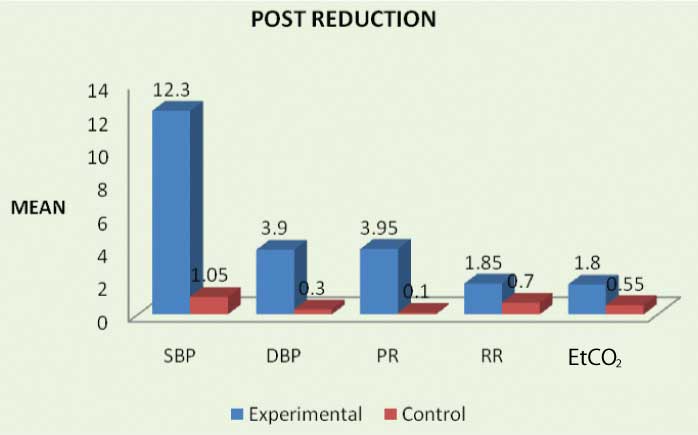
The mean difference in the outcome scores between initial and final measures is presented in [Table/Fig-3]. Further from [Table/Fig-4], it is inferred that, there was statistically significant reduction in all the outcomes following training in study group, whereas statistical significance was not achieved for controls.
Within group-pre post difference.
Comparison of outcomes between groups.
| Outcomes | Study | Control |
|---|
| t-value | p-value | t-value | p-value |
|---|
| Systolic BP (mmHg) | 19.69 | 0.001* | 1.40 | 0.177 |
| Diastolic BP (mmHg) | 3.92 | 0.001* | 0.63 | 0.532 |
| EtCO2 (mmHg) | 3.26 | 0.004* | 1.19 | 0.248 |
*-Significant
Between group analysis shows that there was significantly higher reduction in all the outcomes except EtCO2 following training in study group. The mean difference between groups is also presented [Table/Fig-5].
Comparison of outcomes between groups.
| Post measures (after 30 minutes) | Study | Control | Mean difference | t | p |
|---|
| Mean | SD | Mean | SD |
|---|
| SBP (mmHg) | 133.35 | 9.89 | 144.60 | 11.11 | -11.25 | 11.54 | 0.001* |
| DBP (mmHg) | 91.65 | 9.20 | 91.35 | 6.04 | -3.60 | 3.27 | 0.002* |
| PR (beats/minute) | 81.75 | 7.20 | 86.15 | 8.91 | -3.85 | 3.55 | 0.001* |
| RR (breaths/minute) | 15.25 | 3.32 | 15.60 | 1.60 | -1.15 | 2.46 | 0.018* |
| EtCO2 (mmHg) | 30.00 | 2.51 | 32.95 | 2.56 | -1.25 | 1.74 | 0.09 |
SD: Standard deviation; *-Significant; (-) sign denotes reduction in outcomes
Discussion
The current study result shows that there was significant reduction in SBP and DBP following SB in hypertensive patients. However, such changes were not observed for controls. The present finding correlate well with the study done by Joseph CN et al., who demonstrated significant reduction in systolic and diastolic BP following acute effects of slow breathing, the magnitude of reduction was 8 mmHg and 5 mmHg for systolic and diastolic BP respectively [9]. Anderson DE et al., had demonstrated significant SBP reduction of 6.4±1.8 mmHg [12], whereas DBP had not differed significantly following acute slow breathing. The major difference between the above mentioned two studies is the former author employed voluntary slowing of breathing similar to the present work whereas later used guided breathing device for slow breathing training. Hence present study is more relevant to the study done by Joseph CN et al., and results demonstrate similarity [9]. Present finding shows that there was 12.30±2.79 mmHg drop of systolic and 3.90±4.4 mmHg drop of diastolic BP following SB. The higher reduction in the SBP observed in the present study could have been due to longer duration of training (30 minutes) whereas, in the mentioned previous studies, the time duration of practice was less (5 to 15 minutes).
Joseph CN et al., had demonstrated significant improvement in arterial baroreflex sensitivity following acute slow breathing [9]. The present study has also shown significant reduction in HR and RR following SB. Therefore, reduction of sympathetic activity plays an important role in the reduction of BP following SB. previous studies had demonstrated that excitation of pulmonary stretch receptors following SB, is crucial in reducing sympathetic efferent fibre discharge which helps in causing peripheral vasodilatation [22].
With reference to EtCO2, the present study result shows that there was significant reduction in EtCO2 following SB. The mean reduction was 1.80±2.46 mmHg following training. Anderson DE et al., had also demonstrated significant reduction in EtCO2 following SB [12], but the magnitude of the drop was higher 5±4.5 mmHg. Only very few studies [12,15] have investigated EtCO2 in slow breathing training. It is postulated that the sustained reduction in BP following slow breathing could have been due to changes in the renal retention of sodium and water influenced by PCO2. In the current study, acute effects was only analysed, long-term practice of slow breathing could make greater change in EtCO2. The merit of the present work is, slow breathing training was given by simple recorded verbal instructions. However, in most of the previous studies, guided breathing device was used which is costly and limited in availability [12,15,23]. It is demonstrated that slow breathing rate and not regularisation of breathing that is proper breathing pattern enhanced by breathing device is a crucial factor in reducing BP.
Limitation
In the present work, only acute effects was evaluated. Analysis of long-term influence of SB needs to be extensively studied to better analyse the physiological mechanism of training. The outcomes such as heart rate variability, baroreflex sensitivity and renal measures could be used in future endeavours to make the study more interesting.
Conclusion
Practice of slow breathing is effective in immediate reduction of systolic and diastolic blood pressure. End-tidal carbon dioxide could play a role in reducing blood pressure, but long-term study is warranted to better evaluate its role in blood pressure reduction.
SD: Standard deviation
*-Significant
SD: Standard deviation; *-Significant; (-) sign denotes reduction in outcomes