Misplaced Internal Juglar Vein Central Venous Catheter due to Thrombosis in Subclavian Vein: A Rare Occurrence
Sameer Sethi1, Deepanshu Dhiman2, Kaman Lileswar3, Kaptan Singh4
1 Additional Professor, Department of Anaesthesia and Intensive Care, Postgraduate Institute of Health Sciences, Chandigarh, India.
2 Senior Resident, Department of Anaesthesia and Intensive Care, Postgraduate Institute of Health Sciences, Chandigarh, India.
3 Professor, Department of General Surgery, Postgraduate Institute of Health Sciences, Chandigarh, India.
4 Senior Resident, Department of General Surgery, Postgraduate Institute of Health Sciences, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sameer Sethi, Additional Professor, Department of Anaesthesia and Intensive Care, Post Graduate Institute of Medical Education and Research (PGIMER), Sector 12, Chandigarh-160012, India.
E-mail: sameersethi29@gmail.com
Here, authors report a case of Central Venous Catheter (CVC) malposition in a patient posted for Whipple’s procedure. A 65-year-old male diagnosed with carcinoma head of pancreas, post-chemotherapy was posted for Whipple’s procedure. Ultrasound (USG) guidance CVC line and arterial cannula placement were planned for invasive monitoring and administration of fluids and drugs post-operatively. A post-operative chest radiograph was done which showed that the CVC was malpositioned into the subclavian vein. The venography delineated a clot at the junction of the Internal Jugular Vein (IJV) and the Subclavian Vein (SCV). It was further concluded that presence of this thrombus at the junction of both the vessels prevented the movement of the guidewire towards the Superior Vena Cava (SVC) and therefore the catheter into the SVC. This case report highlights the use of USG not only to visualise the target vessel but also to scan completely till the junction SVC and right atrium for any clot or anatomic malformations in the vasculature.
Complications of central venous catheters, Misdirected catheters, Ultrasound, Venous thrombosis
Case Report
A 65-year-old male diagnosed with carcinoma head of pancreas, post-chemotherapy was posted for Whipple’s procedure. All baseline investigations before the procedure were normal. The anaesthetic plan for the procedure was general anaesthesia with invasive pressure monitoring. CVC line and arterial cannula placement were planned for invasive pressure monitoring and post-operative administration of fluids and drugs. After intravenous induction, the right side IJV was cannulated by a trainee resident under USG guidance, in the presence of an anaesthesia consultant. The seven French triple lumen CVC was placed by Seldinger’s technique, free flow was confirmed in all the three ports and CVC was fixed at 12 cm.
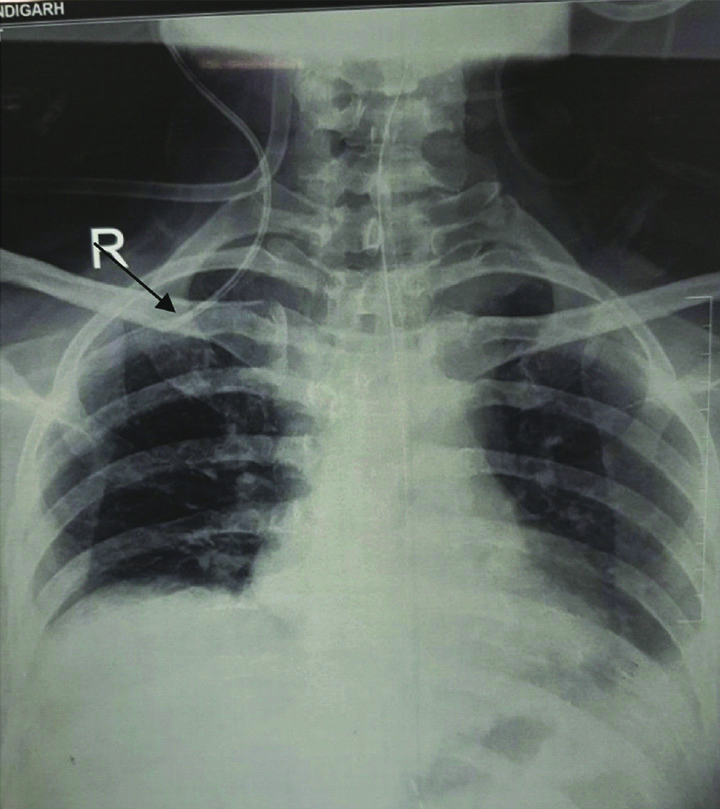
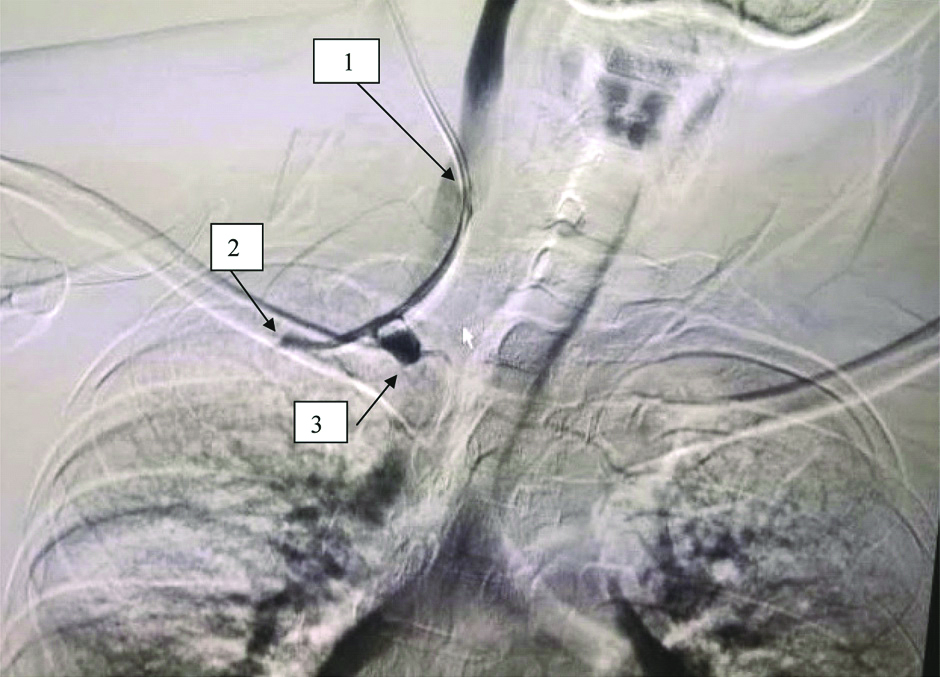
Intraoperatively, no complications were reported and patient was extubated. A post-operative chest radiograph was done which showed that the CVC was malpositioned into the SCV [Table/Fig-1]. Following the catheter malposition, it was planned to take up the patient for further radiological investigation, in order to find out the cause of catheter malposition. The patient was taken-up into the radiological suite and venography was done to find out any vascular abnormality as a cause of malposition. The venography delineated a clot at the junction of the IJV and the SCV [Table/Fig-2].
Chest X-ray anteroposterior view showing CVC tip in SCV.
Venography image; 1- CVC in IJV, 2- tip of CVC in subclavian vein and 3- Thrombus at junction of IJV and SCV.
As the patient was stable in the post-operative and back flow in all the three ports was present and no administration of any inotropes was required, the CVC was not repositioned. Central venous catheter was removed on day 5th postoperatively. Patient was on follow-up for two months on outpatient basics by the surgical team for the primary disease and has not reported of any complications.
Discussion
Central Venous Catheter (CVC) placement is a commonly done procedure for various indications both elective and emergency. It is recommended that CVC should be inserted under USG. USG helps in reducing complications of CVC insertion like haematoma, pneumothorax, arterial puncture and other vascular injury [1]. USG also helps in reconfirming the position of guidewire up to the cardiac chambers before threading of the catheter. Although real time USG has reduced the rate of complications, CVC insertion related complications and malposition are known to occur. Hence, post-insertion chest radiograph is always recommended to look for malpositions and other complications.
In the present case, venography delineated thrombus was present at the junction of the IJV and SVC. Therefore, it was concluded that presence of this thrombus at the junction of both the vessels prevented the movement of the guidewire and the catheter got lodged into the SCV. When using USG for CVC, a complete scan of the major vessels should be done to rule out any clot or anatomical malformations. Complications of dislodgement of such thrombus must also be borne in mind during central venous cannulation procedures.
CVC malposition is defined as presence of catheter tip at any other anatomical site except the superior vena cava or right atrium [2]. CVC malposition although not commonly reported, can result in catheter wedging, erosion and perforation, local venous thrombosis, inadvertent passage of fluid or drugs into mediastinum, thoracic spaces and more cephalad towards the brain tissue [3]. Therefore, CVC position must always be confirmed by a chest radiograph as malposition is associated with increased morbidity and mortality.
The causes of CVC malposition are multiple which include anatomical abnormalities, congenital vascular malformations and bevel position during insertion [4,5]. As reported by Schummer W et al., that left IJV catheterisation is most commonly associated with malpositions followed by right subclavian, left subclavian and right internal jugular vein [6]. Whenever, CVC malposition is detected, it is advised to correct it at the earliest to prevent any further complications. Although catheter malposition occurs commonly, the general approach is to remove the catheter and place it again; only when recurrent malposition occurs the cause for malposition is sought. Commonly anatomical malformations are encountered as a cause of malposition.
Venous thrombosis must be kept in mind when patient is at increased risk of thrombosis formation like malignancy, chemotherapy, pregnancy, obesity, recent surgery, immobilisation and haemodialysis [7]. As in the present case, patient was diagnosed with carcinoma pancreas and had received chemotherapy, the present authors implicate that this may have led to thrombus formation in the subclavian vein. Dislodgement of the thrombus during insertion or removal of the CVC could have led to dreaded complications like systemic embolism. Although none of the complications of catheter malposition and thrombus migration was reported in the present case and also we advocate for always checking for CVC position. A chest radiograph must always be done at the earliest.
USG if available can be used during and prior to insertion to rule out any pre-existing thrombus in the major vessels up to the junction of SVC with right atrium, especially in patients at risk of venous thrombosis as mentioned earlier. USG can also be used to see for the entire course of guidewire before vessel cannulation. In the present case a complete scanning of the vessels and the guidewire was not done hence leading to missed diagnosis of malposition before cannulation.
Conclusion
Replacement or removal of a malpositioned catheter must always be done after diagnosing the cause of malposition as done in the present case. Inadvertent pulling of catheter can cause vascular injury and dislodgement of the thrombus. Hence, it should always be kept in mind that even though CVC placement is a commonly performed procedure its complications increase morbidity and mortality. When available, USG should be used both before and after guidewire insertion, to look for the complete course up till the junction of SVC with right atrium. Patient at risk of venous thrombosis with catheter malposition in them, venous thrombosis must be kept as differential diagnosis for the malposition.
[1]. Palepu GB, Deven J, Subrahmanyam M, Mohan S, Impact of ultrasonography on central venous catheter insertion in intensive careIndian J Radiol Imaging 2009 19:191-98.10.4103/0971-3026.5487719881083 [Google Scholar] [CrossRef] [PubMed]
[2]. Rolden N, Paniagua L, Central venous catheter intravascular malpositioning: causes, prevention, diagnosis, and correctionWest J Emerg Med 2015 16(5):658-64.10.5811/westjem.2015.7.2624826587087 [Google Scholar] [CrossRef] [PubMed]
[3]. Walshe C, Phelan D, Bourke J, Buggy D, Vascular erosion by central venous catheters used for total parenteral nutritionIntensive Care Med 2007 33:534-37.10.1007/s00134-006-0507-917235513 [Google Scholar] [CrossRef] [PubMed]
[4]. Demos TC, Posniak HV, Pierce KL, Olson MC, Muscon M, Venous anomalies of the thoraxAm J Roentgenol 2004 182:1139-50.10.2214/ajr.182.5.182113915100109 [Google Scholar] [CrossRef] [PubMed]
[5]. Park HP, Jeon Y, Hwang JW, Han SH, Bahk JH, Oh YS, Influence of orientations of guidewire tip on the placement of subclavian venous cathetersActa Anaesthesiol Scand 2005 49:1460-63.10.1111/j.1399-6576.2005.00758.x16223390 [Google Scholar] [CrossRef] [PubMed]
[6]. Schummer W, Schummer C, Rose N, Nisen WD, Sakka SG, Mechanical complications and malposition of central venous cannulations by experienced operators. A prospective study of 1794 catheterizations in critically ill patientsIntensive Care Med 2007 33:1055-59.10.1007/s00134-007-0560-z17342519 [Google Scholar] [CrossRef] [PubMed]
[7]. Agarwal AK, Patel BM, Haddad NJ, Central vein stenosis: a nephrologist’s perspectiveSemin Dial 2007 20:53-62.10.1111/j.1525-139X.2007.00242.x17244123 [Google Scholar] [CrossRef] [PubMed]