Complex irreducible dislocation of the Interphalangeal Joint (IPJ) of the great toe is a rare injury, due to the inherent stability of the joint. Miki has classified these injuries into two types, and this article is on a case of complex type II dislocation managed by open reduction and internal fixation. These rare injuries, especially the type II variety, invariably need surgical management and overzealous attempts at closed reduction must be avoided as it risks injury to critical neurovascular and joint supporting structures, leading to poorer patient outcomes. An extensive comparative review of literature is presented here along with the optimal surgical approach, technique and post-operative rehabilitation, so as to maximise patient outcomes following these rare and challenging injuries.
Case Report
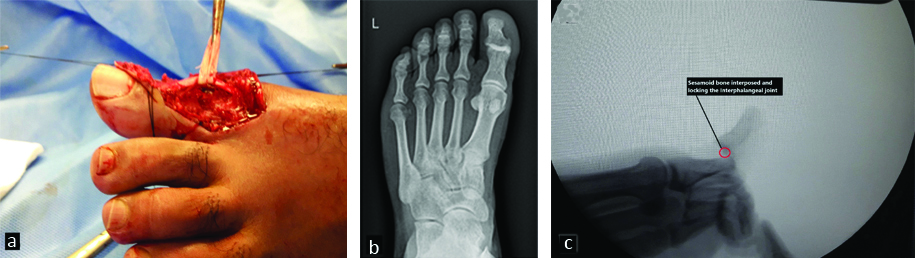
A 39-year-old male presented acutely in the Emergency Room (ER) with a ‘locked toe’, two hours after sustaining the injury, following an accidental fall while playing recreational football. Examination revealed a closed dorsal dislocation injury of the left great toe Interphalangeal Joint (IPJ) with skin dimpling dorsally with mild lateral rotation deformity, neuro-vascular examination was normal [Table/Fig-1]. Repeated attempts at closed reduction in the ER under digital block failed.
Pre-operative image showing visible deformity of irreducible dorsal dislocation great toe with dimpling of skin seen dorsally.

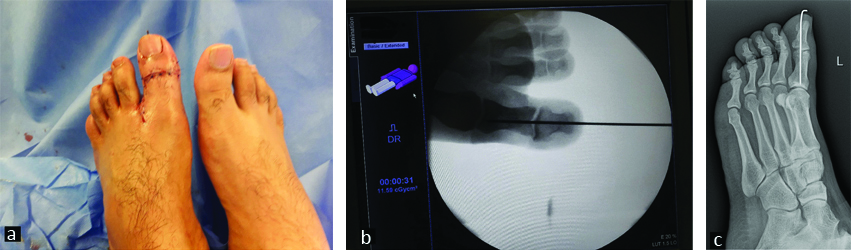
On radiographic evaluation, a dorsal dislocation of great toe with interposition of volar plate and sesamoid bone blocking reduction was suspected; hence it was decided to proceed with open reduction and internal fixation under spinal anaesthesia [Table/Fig-2]. Using a dorsal skin crease incision over the IPJ with mid lateral extension, skin flaps were elevated and Extensor Hallucis Longus (EHL) tendon retracted. Using longitudinal axial traction after opening the dorsal capsule, IPJ was visualised and interposed structures namely volar plate and sesamoid bone pushed from dorsal to plantar direction, away from the joint space and IP joint was reduced. After successful joint reduction, on table Range Of Motion (ROM) testing revealed unstable joint with tendency towards re-subluxation, hence it was decided to stabilise the joint with single axial 1.6 mm k wire [Table/Fig-3].
a) Intraoperative view showing dorsal approach after reduction of dislocation and IPJ seen after retracting EHL tendon. b) X-ray AP view showing overlapping of proximal and distal phalanges with obliteration of joint space typical of Miki type II dorsal dislocation of great toe. c) Intraoperative fluoroscopic image showing lateral view of Miki type II dislocation characterised by distal phalanx hyperextension and over-riding of sesamoid bone over proximal phalanx head.
a) Post-operative image after open reduction and internal fixation with single axial K wire. b) Intraoperative fluoroscopic image after open reduction and internal fixation with single axial K wire. c) Oblique view X ray showing reduced IPJ stabilised with k wire, with joint in good alignment.
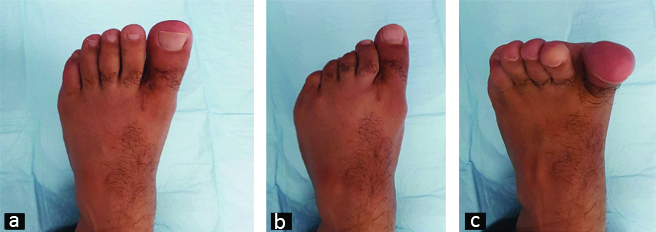
After six weeks implant removal was done, and patient was begun on a rehabilitation program. Patient was followed for upto one year after surgery and has regained almost full motion of his great toe [Table/Fig-4].
Post-operative images at six months showing good and full range of motion of great toe.
Discussion
The IPJ of great toe is a very stable joint due to the box like configuration of supporting structures around the joint namely the dorsal capsule, volar plate, collateral ligaments (both medial and lateral), EHL tendon and Flexor hallucis longus (FHL) tendons, short lever arm of the distal phalanx and the condylar shape of the joint. Normally passive hypertension more than 20° is impossible because of these supporting structures which resist such deforming forces [1-3]. The possible mechanism of injury involves a strong hyperextension force on the IPJ with the foot and metatarso-phalangeal joint fixed in a weight bearing position, such a deforming force is necessary to dislocate the joint [1,2].
Most adults have a sesamoid bone at the level of IPJ of great toe and based on this and the position of volar plate in the IPJ, Miki has classified irreducible dorsal dislocations of great toe into 2 types [1].
Type I Miki: Characterised by both the volar plate and sesamoid found in the IPJ, and the toe is slightly elongated externally, and radiography shows widened joint space on AP view and on lateral view there is good alignment of phalanges. In type I there is detachment of the volar plate from its proximal attachment on the proximal phalanx [Table/Fig-5].
Radiographic image showing Type I Miki Dorsal dislocation of great toe.
[Image courtesy of : Hartog B, Doorn PF, Rijk PC. Sesamoid bone interposition in the interphalangeal joint after dislocation of the hallux: A case report. The Foot and Ankle Online Journal 2009;2(7):3.]
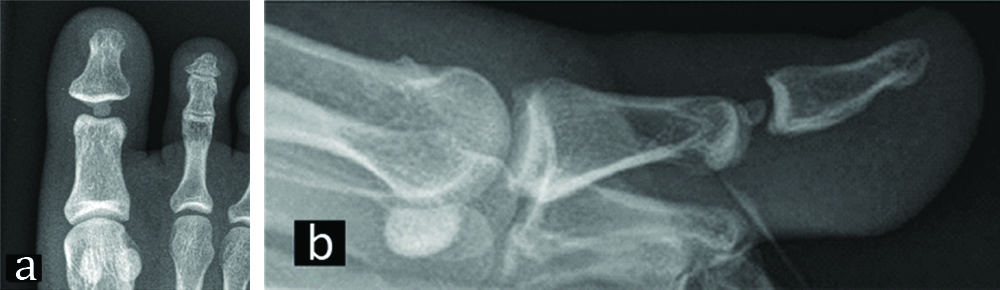
Type II Miki: These are also known as complex dislocations characterised by VP displaced completely dorsal to IPJ and sesamoid bone over-rides the proximal phalanx head. Radiographically, on AP view, there is narrowing or overlapping of phalanges and on lateral view, the distal phalanx is hyperextended with the sesamoid bone seen over the proximal phalanx head. In type II, there is complete detachment of volar plate from its proximal and distal attachment and it is displaced dorsally over the IPJ thereby locking the joint in hyper-extension [Table/Fig-2b,c].
Which surgical approach is better, dorsal, plantar, medial or lateral? Controversy exists in literature regarding the ideal surgical approach for open reduction. The author feels in an open dislocation, the site of wound should guide the approach as it seems unnecessary and illogical to create another opening, hence for dislocation with a dorsal wound, a dorsal approach is preferred and vice-versa. However, most operators prefer the dorsal approach [1,2,4-14], lateral or medial approach allows easy reduction of the trapped sesamoid bone but does not entail easy access for reduction and repair of injured volar plate and will be difficult in complex type II dislocations [2,12]. Some operators using the dorsal approach divide the EHL tendon longitudinally to gain access to joint but this creates additional trauma and instead it is better to retract the tendon laterally. Liberson A et al., and Yasuda T et al., seem to prefer a plantar approach probably because of open plantar wound on presentation in their reports and both went on to repair the volar plate, hence plantar approach has an additional advantage of volar plate repair for added joint stability but the trade-off is the risk of hypertrophic scar on weight bearing part of sole or delayed wound healing [3,6]. Again, the repair of volar plate is controversial with some authors favoring no repair [8]. Hence the surgical approach of choice by consensus would be the dorsal approach as it offers easy access, less scarring and morbidity and faster wound healing [1,2,5,7-12,14].
What is the ideal surgical reduction and fixation technique? After reduction of the joint, ROM and medio-lateral stability of the IPJ is tested, if there is joint instability, then a single axial Kirschner (K) wire (1.4-1.6 mm size) should be inserted to fix the joint for additional stability and kept in place for 4-6 weeks. However, Miki T et al., in his series has not performed k wire fixation and instead immobilised the joint with dorsal splint in slight flexion for 4-6 weeks [1]. The author would like to add that an initial trial of closed reduction under digital block which can sometimes be effective as reported by Sorene ED et al., [10]. Chung DW et al., using a dorso-lateral approach and described repair of ruptured Lateral Collateral Ligament (LCL) that was entrapped in the joint [13], but most operators report excellent outcomes without repair of volar plate and collateral ligaments [1,2,4,8,9,12].
What is the best post-reduction immobilisation protocol? Most authors recommend immobilsation for 3-4 weeks following reduction with/without internal fixation [1,4,6] and the use of a dorsal splint with the IPJ in slight flexion is also recommended [1,3,5]. Alternative methods of stabilisation have been described in literature such as short leg cast [1], buddy splinting [2], bulky compression dressing [4], toe spica and some authors even recommend specialised post-operative shoe for weight bearing e.g., Rocker-bottom shoes [8], wooden-soled shoe [13].
Finally, Woon CY has described a percutaneous reduction technique for irreducible dorsal dislocation of great toe, however the author would caution that percutaneous technique be used only in selective cases like Miki type I dislocations and the use of intraoperative image intensifier is mandatory when performing this minimally invasive technique [15].
A comparative review of previously published cases of irreducible Dorsal hallucal dislocations is shown in [Table/Fig-6] [1-5,7-9,11-16].
Comparative review of previously published cases of irreducible dorsal hallucal dislocations [1-5,7-9,11-16].
| S.No. | Author | Cases | Type of dislocation | Interposed/‘Trapped’ structures | Injured structures | Surgical approach | Procedure done |
|---|
| 1. | Miki T et al., [1] | 22 | Open and closedType I- 14 casesType II- 8 cases | VP, sesamoid bone | Collateral ligaments, VP | Dorsal approach | Open reduction, splint immobilisation for 3-4 weeks. |
| 2. | Nelson TL et al., [2] | 1 | Closed, Miki type II | VP | VP | Dorsal approach | Open reduction |
| 3. | Liberson A et al., [3] | 1 | Open, Miki type II | VP, sesamoid bone | VP | Plantar zig-zag approach | Open reduction, VP repair and dorsal splint. |
| 4. | Crosby LA et al., [4] | 1 | Closed, Miki type II | VP, sesamoid bone | VP | Medial approach | Open reduction and buddy taping and special protective hard sole for three weeks. |
| 5. | Weiss AP et al., [5] | 1 | Closed, Miki type I | FHL tendon, sesamoid bone | Volar plate (VP) and Lateral collateral ligament(LCL) | Dorsal midline approach | Open reduction, ligament and VP repair followed by splinting. |
| 6. | Hartog B et al., [7] | 1 | Closed, Miki type I | VP, sesamoid bone | VP | Dorsal S incision | Open reduction and sesamoid excision |
| 7. | Leung HB et al., [8] | 1 | Closed, Miki type I | VP, sesamoid bone | VP | Dorsal approach | Open reduction and internal fixation with K wire. |
| 8. | Hatori M et al., [9] | 1 | Closed, Miki type I | VP, sesamoid bone | VP | Dorsal approach | Open reduction and internal fixation with K wire. |
| 9. | Bin AbdRazak HR et al., [11] | 1 | Closed, Miki type II | Sesamoid bone | | Dorsal midline with extensor split. | Open reduction, internal fixation with K wire and resection of sesamoid. K wire removal after six weeks. |
| 10. | Kursunoglu S et al., [12] | 1 | Open, Miki type I | Sesamoid bone | | Medial approach | Open reduction and dorsal splint. |
| 11. | Chung DW et al., [13] | 1 | Closed, Miki type I | Lateral collateral ligament | LCL | Dorso-lateral approach | Open reduction, LCL repair, K wire fixation and implant removal after 4 weeks. |
| 12. | Singh R et al., [14] | 1 | Closed, Miki type I | VP, sesamoid bone | VP | Dorso-lateral approach (Inverted L incision) | Open reduction and dorsal splinting. |
| 13. | Woon CY [15] | 2 | Closed, Miki type II | VP, sesamoid bone | | Percutaneous | Percutaneous reduction and k wire fixation. |
| 14. | Kumar MK et al., [16] | 1 | Closed, Miki type II | VP, sesamoid bone | VP | Dorso-lateral approach | Open reduction and k wire fixation and implant removal after four weeks. |
*VP: Volar plate; †FHL: Flexor hallucis longus; ‡LCL: Lateral collateral ligament
Conclusion
Irreducible dorsal dislocations of the hallucal IPJ are challenging and rare injuries especially Miki type II variety and an initial trial of closed reduction is recommended. If closed reduction fails, open reduction and fixation is undertaken with dorsal approach being favored by most operators followed by a period of immobilisation for 3-4 weeks. The results of the treatment of these rare injuries are nevertheless satisfying with excellent outcomes being reported.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
*VP: Volar plate;
†FHL: Flexor hallucis longus;
‡LCL: Lateral collateral ligament
[1]. Miki T, Yamamuro T, Kitai T, An irreducible dislocation of the great toe. Report of two cases and review of the literatureClin Orthop Relat Res 1988 230:200-06.10.1097/00003086-198805000-00023 [Google Scholar] [CrossRef]
[2]. Nelson TL, Uggen W, Irreducible dorsal dislocation of the interphalangeal joint of the great toeClin Orthop Relat Res 1981 157:110-12.10.1097/00003086-198106000-00019 [Google Scholar] [CrossRef]
[3]. Liberson A, Nyska M, Klenerman L, Irreducible interphalangeal dislocation of the big toe: The plantar surgical approachThe Foot 1993 3(1):28-30.10.1016/0958-2592(93)90027-Z [Google Scholar] [CrossRef]
[4]. Crosby LA, McClellan JW 3rd, Prochaska VJ, Irreducible dorsal dislocation of the great toe interphalangeal joint: case report and literature reviewFoot Ankle Int 1995 16(9):559-61.10.1177/1071100795016009088563924 [Google Scholar] [CrossRef] [PubMed]
[5]. Weiss AP, Yates AJ, Irreducible dorsal interphalangeal great toe dislocationOrthopedics 1992 15(4):480-82. [Google Scholar]
[6]. Yasuda T, Fujio K, Tamura K, Irreducible dorsal dislocation of the interphalangeal joint of the great toe: Report of two casesFoot Ankle 1990 10(6):331-36.10.1177/1071100790010006082358262 [Google Scholar] [CrossRef] [PubMed]
[7]. Hartog B, Doorn PF, Rijk PC, Sesamoid bone interposition in the interphalangeal joint after dislocation of the hallux: A case reportThe Foot and Ankle Online Journal 2009 2(7):310.3827/faoj.2009.0207.0003 [Google Scholar] [CrossRef]
[8]. Leung HB, Wong WC, Irreducible dislocation of the hallucal interphalangeal jointHong Kong Med J 2002 8:295-99. [Google Scholar]
[9]. Hatori M, Goto M, Tanaka K, Smith RA, Kokubun S, Neglected irreducible dislocation of interphalangeal joint of the great toe: A case reportJ. Foot Ankle Surg 2006 45(4):271-74.10.1053/j.jfas.2006.04.01116818156 [Google Scholar] [CrossRef] [PubMed]
[10]. Sorene ED, Regev G, Complex dislocation with double sesamoid entrapment of the interphalangeal joint of the halluxJ Foot Ankle Surg 2006 45(6):413-16.10.1053/j.jfas.2006.09.01017145466 [Google Scholar] [CrossRef] [PubMed]
[11]. Bin Abd Razak HR, Chia ZY, Tan HC, Irreducible dislocation of the great toe interphalangeal joint secondary to an incarcerated sesamoidCase Rep Orthop 2015 2015:23168510.1155/2015/23168525874146 [Google Scholar] [CrossRef] [PubMed]
[12]. Kursunoglu S, Resnick D, Goergen T, Traumatic dislocation with sesamoid entrapment in the interphalangeal joint of the great toeJournal of Trauma 1987 27(8):959-61.10.1097/00005373-198708000-000213612878 [Google Scholar] [CrossRef] [PubMed]
[13]. Chung DW, Jeong BO, Irreducible dislocation of the interphalangeal joint of the great toe with lateral collateral ligament entrapment: A case reportJ Korean Fract Soc 2009 22(2):110-13.10.12671/jkfs.2009.22.2.110 [Google Scholar] [CrossRef]
[14]. Singh R, Rohilla R, Siwach R, Irreducible dislocation of the interphalangeal joint of the great toe in a collegiate football player due to sesamoid bone interposition- A case report and literature reviewThe Internet Journal of Orthopedic Surgery 2008 14(1)10.5580/292b [Google Scholar] [CrossRef]
[15]. Woon CY, Dislocation of the interphalangeal joint of the great toe: is percutaneous reduction of an incarcerated sesamoid an option? A report of two casesJ Bone Joint Surg Am 2010 92(5):1257-60.10.2106/JBJS.I.0101820439675 [Google Scholar] [CrossRef] [PubMed]
[16]. Kumar MK, Kumar TA, Traumatic Miki Type 2 dislocation of interphalangeal joint of great toe- A case report and review of literatureIOSR Journal of Dental and Medical Sciences 2015 14(3):42-43. [Google Scholar]