Introduction
One challenge that endodontists may face during clinical practice is intracanal separation of an instrument. This situation is disappointing for both the patient and practitioner [1].
Root canal shaping instruments can separate due to torsional failure, cyclic fatigue, or both and several other factors, such as instrument design, instrument composition, canal configuration, canal preparation technique and the number of uses can also contribute to the separation process [2-5].
The separation rate of stainless steel instruments has been reported to range between 0.25% to 6% [4,6] while that of nickel-titanium instruments ranges between 1.3% to 5.77% [6-8].
Although some studies have reported no effect on the outcome of teeth with a retained instrument fragment [4,7,9], others have reported a lower healing rate [10,11].
The main concern is that a separated instrument can hinder the cleaning effectiveness of a root canal, affecting the treatment outcome indirectly. Therefore, the benefits of retrieval should be weighed against the risks of other complications that could occur during the retrieval process [3,12].
Several methods have been suggested for separated instrument retrieval and specialised devices have been introduced for this purpose, such as ultrasonic devices, the Instrument Removal System, and the Masserann kit [11,13,14].
This paper includes four cases in which an ultrasonic tip was used to retrieve separated instrument fragment.
Case Report-1
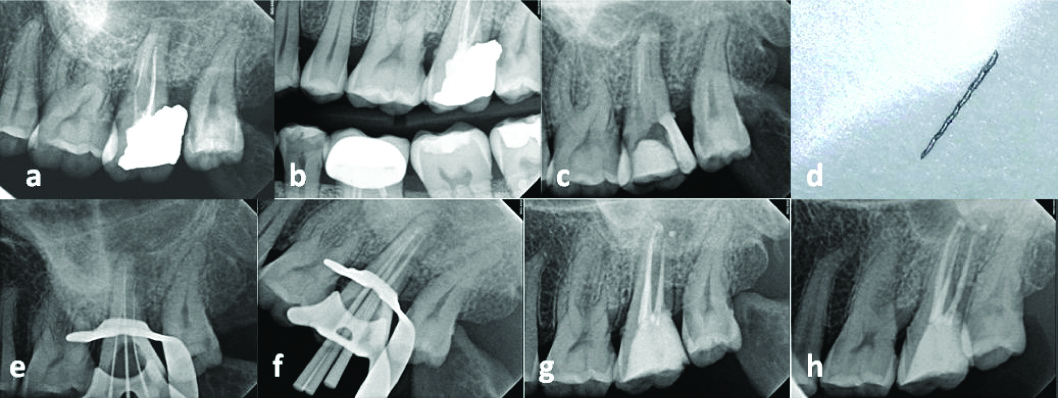
A 40-year-old female patient was referred from the Restorative Department clinic for root canal retreatment of the maxillary left second molar (#27) due to defective amalgam restoration and poor root canal treatment. The patient reported to the restorative clinic for routine checkup. The medical history was unremarkable. The molar had undergone a root canal treatment five years back. On clinical examination, it was noted that tooth #27 had a defective amalgam restoration. It was not tender to percussion or palpation and there were no signs of mobility or periodontal affection. Radiographic examination of the tooth showed a poor/unacceptable root canal treatment with apical radiolucency and separated file located apically in the Mesiobuccal (MB) canal [Table/Fig-1a]. An overhanging amalgam restoration was noticed [Table/Fig-1b]. The tooth was diagnosed with asymptomatic apical periodontitis [15]. Informed consent was obtained from the patient prior to the retreatment. Root canal retreatment was initiated, with removal of the old amalgam restoration and building up of the tooth with Glass ionomer cement (GIC) (Fuji IX GP®; GC, Chicago, IL, USA) to allow rubberdam isolation [Table/Fig-1c]. Next, an access cavity was created under the rubberdam isolation using a Dental operating microscope (DOM) (OPMI Pico; Zeiss, Oberkochen, Germany) and three canals were identified. The old gutta-percha was removed using Protaper retreatment files (Dentsply Maillefer, Ballaigues, Switzerland). A staging platform was created using a Gates Glidden bur (size #2; Dentsply-Maillefer) to expose the tip of the separated fragment in the MB canal, and an ultrasonic tip (Satelec/Acteon, Merignac, France) was then used intermittently at medium frequency (36 kHz) without simultaneous coolant irrigation to successfully retrieve the instrument fragment [Table/Fig-1d]. The working length was determined radiographically [Table/Fig-1e] and the canal was prepared using the Protaper Next system (Dentsply Maillefer) to size X3, with copious irrigation of 5% NaOCl solution followed by 17% EDTA. The canals were dried and filled with gutta-percha and sealer cement (AH26 sealer; Dentsply Detrey Gmbh, Konstanz, Germany) using System B (Courtesy SybronEndo, Orange, CA, USA) and Hotshot (Discus Dental, Culver City, CA, USA) devices [Table/Fig-1f,g]. The access cavity was immediately sealed with GIC and then replaced one week later by a composite restoration (GC America, Chicago, IL, USA). The patient was referred back to the Restorative Department for crown restoration. She decided to delay the crown due to financial reason. At the six-month follow-up visit, the tooth was clinically asymptomatic and radiographs showed that the lesion had reduced in size [Table/Fig-1h].
a) pre-operative periapical radiograph showing the separated instrument in the mesial root; b) Bitewing radiograph of the left side. (c) Glass Ionomer build-up and removal of old gutta-percha; d) image of the retrieved instrument; e) Determination of working length; f) Master cone selection; g) Postoperative periapical radiograph; h) 6 months follow-up periapical radiograph.
Case Report-2
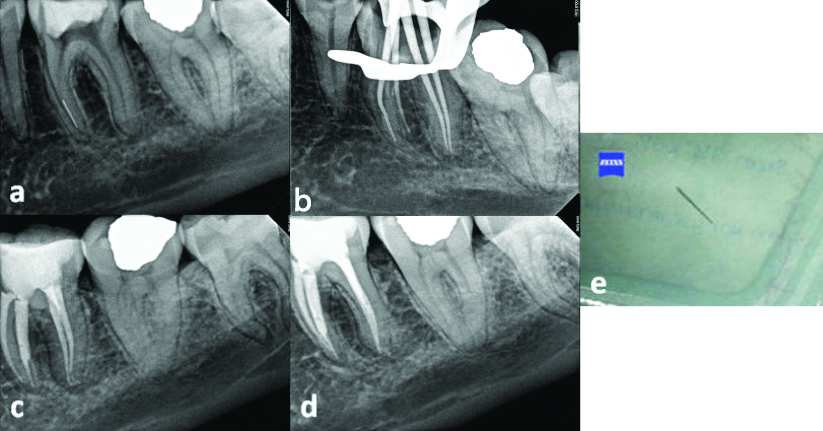
A 30-year-old female patient with an unremarkable medical history was referred by a general dentist to the endodontic clinic for retrieval of an instrument that had accidentally separated during root canal treatment of the mandibular left first molar (#36) one week back. The dentist had decided not to continue the treatment due to separation of an X1 file in the MB canal and referred the case to specialised endodontic clinic with a microscope and better facilities. On clinical examination, tooth #36 was tender to percussion with no signs of mobility or periodontal infection. Radiographs showed widening of the Periodontal ligament (PDL) at the apex of the mesial root and a separated file located apically in the MB canal [Table/Fig-2a]. Symptomatic apical periodontitis was diagnosed. Root canal treatment of the involved tooth was initiated under rubberdam isolation and DOM magnification. A glide path was prepared carefully by gate glidden bur sizes 2 and 3 from the canal orifice to the tip of the separated instrument then an ultrasonic tip was used to remove it. The separated file was retrieved and the canals were prepared and filled with gutta-percha and AH26 sealer cement using System B and Hotshot devices [Table/Fig-2b,c]. The six-month follow-up revealed no clinical symptoms or radiographic apical abnormalities [Table/Fig-2d]. [Table/Fig-2e] shows the retrieved instrument.
a) Preoperative periapical radiograph of tooth #36; b) shows gutta-percha master cone trial; c) Postoperative radiograph; d) Follow-up radiograph; e) The retrieved instrument.
Case Report-3
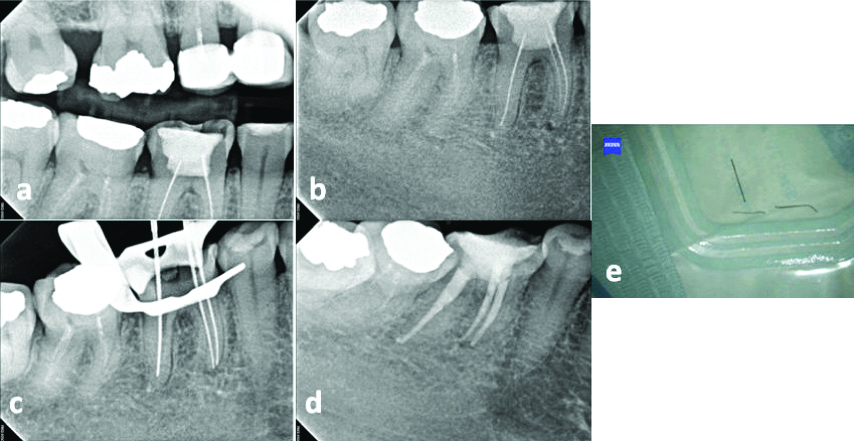
A 41-year-old female patient, in good health, was referred from the Restorative Department for root canal retreatment of the mandibular right first molar (#46). She was having pain on chewing in tooth #46 since last two days. The tooth had undergone previous endodontic treatment nine years ago. On clinical examination, the involved tooth was tender to percussion and palpation, with no signs of mobility. The radiographic examination showed a previous poor/unacceptable root canal treatment and three separated files (two in the mesial root and one in the distal root) and a widened PDL space [Table/Fig-3a,b]. The patient was diagnosed with symptomatic apical periodontitis. The rubberdam was applied and access was established under DOM. The three separated files were successfully removed using an ultrasonic tip vibrating intermittently at medium frequency (36 kHz) without simultaneous coolant irrigation. The working length was determined using Root ZX apex locator (J. Morita Co., Kyoto, Japan) and confirmed with periapical radiograph taken with mesial shift [Table/Fig-3c] and all canals were cleaned and shaped using a Protaper Next system with NaOCl 5% irrigation. The canals were flushed with EDTA 17% and then dried and obturated with gutta-percha and AH26 sealer cement using System B and Hotshot devices [Table/Fig-3d]. The access cavity was temporarily sealed and the patient was referred back to the Restorative Department for final restoration. [Table/Fig-3e] shows the retrieved instrument.
a) Bitewing radiograph of the right side; b) Preoperative periapical radiograph of tooth #36; c) Working lengths determination; d) Postoperative radiograph; e) The retrieved instrument.
Case Report-4
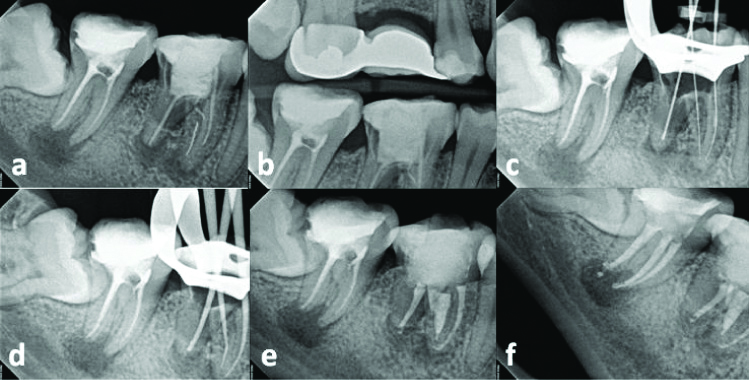
A 31-year-old male patient was referred from the Restorative Department for root canal retreatment of the mandibular right first (#46) and second (#47) molars. The patient complained of pain on chewing in the right posterior tooth region since the last three days. The medical history was unremarkable. The molars had undergone root canal treatment 3 years back. On clinical examination, tooth #46 was tender to percussion and palpation, whereas tooth #47 was not tender to percussion. A radiographic examination showed a previous poor/unacceptable root canal treatment with apical radiolucency of both teeth and separated instrument in the Mesiolingual (ML) canal [Table/Fig-4a]. Tooth #46 showed radiolucency at the furcation area [Table/Fig-4b] and was diagnosed with symptomatic apical periodontitis, while tooth #47 was diagnosed with asymptomatic apical periodontitis. The patient was referred to surgery clinic for extraction of third molar tooth (#48). Both teeth (#46 and 47) were retreated under rubberdam isolation. The old gutta-percha was removed using ProTaper retreatment files (Dentsply Maillefer, Ballaigues, Switzerland) under DOM. The furcation perforation was repaired with mineral trioxide aggregate (MTA) (Dentsply Tulsa Dental, Tulsa, OK, USA). The ML canal was overflared due to a previous attempt to remove the separated file. There was no need to create a staging platform since the fragment was clearly visible. The instrument fragment was successfully retrieved using an ultrasonic tip vibrating intermittently at medium frequency (36 kHz) without simultaneous coolant irrigation. The working length was determined [Table/Fig-4c], and all canals were cleaned and shaped using the Protaper Next system and then flushed with 5% NaOCl solution and 17% EDTA. Canals were filled with gutta-percha and AH26 sealer cement using System B and Hotshot devices [Table/Fig-4d,e]. Root canal treatment was performed for tooth #47 in another visit [Table/Fig-4f]. The access cavities were temporarily sealed and the patient was referred back to the Restorative Department for final restoration. The 48 tooth was planned for extraction but the patient missed the appointment in the surgical clinic. Patient was given an appointment for follow-up, but he did not show-up.
a) Preoperative periapical radiograph of teeth #46 & #47; b) Bitewing radiograph of the right side; c) Working lengths determination of tooth #46; d) Master cone selection; e) Postoperative radiograph of tooth #46; f) Postoperative radiograph of both teeth #46 and #47.
Discussion
The final goal of management of separated instruments is not only to remove broken instruments, but also to preserve the integrity of the tooth structure.
The presence of separated instrument in the root canal usually prevents straight line access to the root apex, which hinders cleaning, disinfection, and filling of the entire root canal system. Management strategies include bypassing, retrieving or leaving the fragment inside the canal as part of the obturation material to be monitored during follow-up [3,12]. Bypassing the separated instrument using small size hand file should always be attempted because oftentimes it can be successful removed [16]. Care should be taken while bypassing a separated long fragment to avoid engagement of the bypassing file around the separated fragment, or perforation of the root. The separated instrument can be retained and incorporated into the root canal filling if it cannot be removed. This was a treatment option that was recommended before the use of ODM and the ultrasonic tips [17].
In the present report, the separated instruments were located at different levels. All were successfully removed. Successful removal of separated instruments depends on several factors, such as the position of the instrument in relation to the canal curvature, the depth of the instrument within the canal, the type of separated instrument, and the size of the fragment [3,12].
Straight line access should be used for successful removal of a separated instrument. This is achieved by creating a staging platform using a Gates Glidden bur. With the help of DOM, this technique improves intracanal visibility and offers better control of the ultrasonic tip inside the canal [13,18]. This technique was successfully used in case #1. Different techniques have been used by Suter B et al., to retrieve separated instruments. He concluded that success depends not on the fragment location, but also on the time taken to remove it [4]. Ultrasonics are also frequently effective for retrieval of separated instruments, as in the present report. A study have reported that ultrasonics allows for faster removal of instruments than the microtube devices [19]. Another study found that a combination of ultrasonic and a microtube is very helpful [14]. Souter NG et al., reported higher success rates using ultrasonic to remove the separated instruments from the coronal third portion of the canal than from the apical portion [20]. The success rate is usually lower when the instrument fragment is located beyond the curve [21].
When using ultrasound, the ultrasonic tip should be activated in a dry field without simultaneous coolant irrigation to allow better visibility under the DOM. To overcome the heat generated during this procedure, medium power should be used and the device should be applied intermittently [22,23]. Although the retrieval of apical separated instruments allows for better disinfection of the root canals, the process usually removes dentin along with the obturation material [24]. Care should be taken to avoid weakening the root, which could result in the fracture of root. Apical lesions seem to affect healing more significantly than retained instrument fragments [7,25]. However, Spili P et al., reported minimal influence of a periapical lesion in the outcome of the endodontic treatment with the presence of separated instrument, provided the procedure is performed to a high technical standard [7]. He further reported poor prognosis, if the technique used to remove the separated instrument is suboptimal. Surgical intervention should be considered when the non-surgical trial fails, symptoms persist, or periapical radiolucencies are detected radiographically during follow-up visits [26].
It is difficult to decide which technique is better. Careful evaluation of the case and determination of the possible risks should be considered before attempting the removal of the instrument. The morphology of the root canal, restorative status of the tooth structure, availability of armamentarium and prognosis of the case should be considered too.
Conclusion
Use of ultrasonic tips in combination with DOM after creating a staging platform is very effective for removing separated instruments from the root canal. Individual case evaluation and planning are essential for a positive outcome and care must be taken during any retrieval attempt to avoid further canal damage.
[1]. Madarati AA, Watts DC, Qualtrough AJ, Opinions and attitudes of endodontists and general dental practitioners in the UK towards the intracanal fracture of endodontic instruments: part 1Int Endod J 2008 41(12):1079-87.10.1111/j.1365-2591.2008.01473.x19133097 [Google Scholar] [CrossRef] [PubMed]
[2]. Sattapan B, Nervo GJ, Palamara JEA, Messer HH, Defects in rotary nickel-titanium files after clinical useJ Endod 2000 26(3):161-65.10.1097/00004770-200003000-0000811199711 [Google Scholar] [CrossRef] [PubMed]
[3]. Parashos P, Messer HH, Rotary NiTi instrument fracture and its consequencesJ Endod 2006 32(11):1031-43.10.1016/j.joen.2006.06.00817055902 [Google Scholar] [CrossRef] [PubMed]
[4]. Suter B, Lussi A, Sequeira P, Probability of removing fractured instruments from root canalsInt Endod J 2005 38(2):112-23.10.1111/j.1365-2591.2004.00916.x15667633 [Google Scholar] [CrossRef] [PubMed]
[5]. Sigueira JF, Aetiology of root canal treatment failure: why well-treated teeth can failInt Endod J 2001 34(1):01-10.10.1046/j.1365-2591.2001.00396.x11307374 [Google Scholar] [CrossRef] [PubMed]
[6]. Iqbal MK, Kohli MR, Kim JS, A retrospective clinical study of incidence of root canal instrument separation in an endodontics graduate program: a PennEndo database studyJ Endod 2006 32(11):1048-52.10.1016/j.joen.2006.03.00117055904 [Google Scholar] [CrossRef] [PubMed]
[7]. Spili P, Parashos P, Messer HH, The impact of instrument fracture on outcome of endodontic treatmentJ Endod 2005 31(12):845-50.10.1097/01.don.0000164127.62864.7c16306815 [Google Scholar] [CrossRef] [PubMed]
[8]. Al-Nazhan S, Al-Attas MH, Al-Maflehi N, Retrieval outcome of separated endodontic instruments by Saudi endodontic board residents: A Clinical retrospective studySaudi Endod J 2018 8(2):77-81.10.4103/sej.sej_13_18 [Google Scholar] [CrossRef]
[9]. Panitvisai P, Parunnit P, Sathorn C, Messer HH, Impact of a retained instrument on treatment outcome: a systematic review and meta-analysisJ Endod 2010 36(5):775-80.10.1016/j.joen.2009.12.02920416418 [Google Scholar] [CrossRef] [PubMed]
[10]. Strindberg L, The dependence of the results of pulp therapy on certain factors: an analytic study based on radiographic and clinical follow-up examinationActa Odontol Scand 1956 14(Suppl):1-175. [Google Scholar]
[11]. Fu M, Zhang Z, Hou B, Removal of broken files from root canals by using ultrasonic techniques combined with dental microscope: a retrospective analysis of treatment outcomeJ Endod 2011 37(5):619-22.10.1016/j.joen.2011.02.01621496659 [Google Scholar] [CrossRef] [PubMed]
[12]. Madarati AA, Hunter MJ, Dummer PM, Management of intracanal separated instrumentsJ Endod 2013 39(5):569-81.10.1016/j.joen.2012.12.03323611371 [Google Scholar] [CrossRef] [PubMed]
[13]. Ruddle CJ, Nonsurgical retreatmentJ Endod 2004 30:827-45.10.1097/01.don.0000145033.15701.2d15564860 [Google Scholar] [CrossRef] [PubMed]
[14]. Al-Zahrani MS, Al-Nazhan S, Retrieval of separated instruments using a combined method with a modified vista dental tipSaudi Endod J 2012 2(1):41-45.10.4103/1658-5984.104421 [Google Scholar] [CrossRef]
[15]. AAE Consensus Conference Recommended Diagnostic TerminologyJ Endod 2009 35:163410.1016/j.joen.2009.09.035 [Google Scholar] [CrossRef]
[16]. Al-Fouzan KS, Incidence of rotary ProFile instrument fracture and the potential for bypassing in vivoInt Endod J 2003 36(12):864-67.10.1111/j.1365-2591.2003.00733.x14641426 [Google Scholar] [CrossRef] [PubMed]
[17]. McGuigan MB, Louca C, Duncan HF, Clinical decision-making after endodontic instrument fractureBr Dent J 2013 214(8):395-400.10.1038/sj.bdj.2013.37923619858 [Google Scholar] [CrossRef] [PubMed]
[18]. Gencoglu N, Helvacioglu D, Comparison of the different techniques to remove fractured endodontic instruments from root canal systemsEur J Dent 2009 3(2):90-95. [Google Scholar]
[19]. Alomairy KH, Evaluating two techniques on removal of fractured rotary nickel titanium endodontic instruments from root canals: an in vitro studyJ Endod 2009 35(4):559-62.10.1016/j.joen.2008.12.01919345805 [Google Scholar] [CrossRef] [PubMed]
[20]. Souter NG, Messer HH, Complications associated with fractured file removal using an ultrasonic techniqueJ Endod 2005 31(6):450-52.10.1097/01.don.0000148148.98255.15 [Google Scholar] [CrossRef]
[21]. Ward JR, Parashos P, Messer HH, Evaluation of an ultrasonic technique to remove fractured rotary nickel-titanium endodontic instruments from root canals: clinical casesJ Endod 2003 29(11):764-67.10.1097/00004770-200311000-0001814651286 [Google Scholar] [CrossRef] [PubMed]
[22]. Madarati AA, Qualtrough AJ, Watts DC, Factors affecting temperature rise on the external root surface during ultrasonic retrieval of intracanal separated filesJ Endod 2008 34(9):1089-92.10.1016/j.joen.2008.05.01818718371 [Google Scholar] [CrossRef] [PubMed]
[23]. Hashem AA, Ultrasonic vibration: temperature rise on external root surface during broken instrument removalJ Endod 2007 33(9):1070-73.10.1016/j.joen.2007.06.00517931935 [Google Scholar] [CrossRef] [PubMed]
[24]. Madarati AA, Qualtrough AJ, Watts DC, A microcomputed tomography scanning study of root canal space: changes after the ultrasonic removal of fractured filesJ Endod 2009 35(1):125-28.10.1016/j.joen.2008.10.00519084141 [Google Scholar] [CrossRef] [PubMed]
[25]. Di Fiore P, A dozen ways to prevent nickel-titanium rotary instrument fractureJ Am Dent Assoc 2007 138(2):196-201.10.14219/jada.archive.2007.013617272374 [Google Scholar] [CrossRef] [PubMed]
[26]. Satheesh SL, Jain S, Bhuyan AC, Devi LS, Surgical management of a separated endodontic instrument using second generation platelet concentrate and hydroxyapatiteJ Clin Diagn Res 2017 11(6):ZD01-03.10.7860/JCDR/2017/25761.999128764303 [Google Scholar] [CrossRef] [PubMed]