Case Report
A 75-year-old man with a chief complaint of worn dentition and inability to chew properly visited the department of Oral Medicine. He had no past medical history and overall health was good. The patient was a habitual tobacco chewer, often visited the local dentist in past for the treatment of painful teeth. The treatment given was usually extraction of certain teeth to relieve the pain.
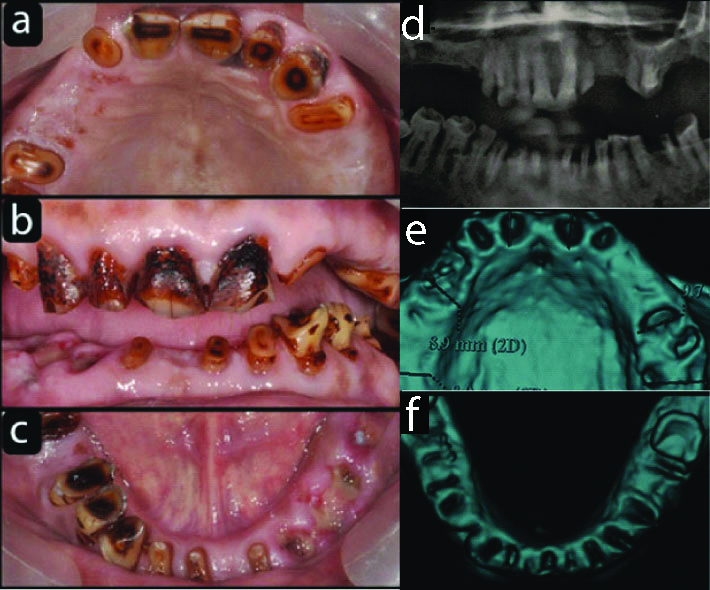
After careful examination, the patient was referred to Department of Periodontics for oral hygiene evaluation and better treatment of remaining dentition. Intraoral examination revealed debilitated anterior dentition with missing posterior teeth. Tobacco stains were visible on all present teeth [Table/Fig-1a-c]. A careful oral examination of the remaining dentition was done, all the present teeth were evaluated for their prognosis and survival. The remaining anterior dentition had severe attrition in both upper and lower arches. The posterior teeth were missing in maxillary arch. The orthopantomogram of the patient showed periapical pathologies in several teeth [Table/Fig-1d]. A diagnosis of doubtful prognosis was made for the entire dentition and was referred to Oral Surgery Department for extraction of all the teeth.
a) Preoperative maxillary occlusal view; b) Preoperative Frontal view. c) Preoperative mandibular occlusal view; d) Preoperative OPG; e) Maxilla Denta Scan after extraction
Soft tissues healed well after six weeks of the extraction. The patient was advised for complete cessation of tobacco chewing habit before undertaking the next step for complex reconstruction.
Patient was quite compliant in avoiding tobacco habit, as it was evaluated in periodic checkups. Patient insisted on fixed prosthesis as replacement of teeth.
Patient was referred to radiology department for full mouth Dentascan. The 3D view after the scan showed fresh extraction sockets for both maxilla and mandible [Table/Fig-1e,f].
The scan report for each socket showed good cortical bone apically and palatally in maxilla. The same favourable report was for mandible as thick cortical bone was present. Interarch space was less than 10 mm and the tissue biotype was thick. A screw retained segmental full arch prosthesis for both maxilla and mandible was planned.
The patient was clearly explained about the segmental detachable prosthesis planned with eight and six implants in maxilla and mandible respectively [1]. The complications involved with waiting period of one year till prosthesis delivery and the financial aspect with strict follow-up was also explained to the patient. Cessation of the tobacco chewing habit was advised, as it was risk factor for failure of complex reconstruction. This was in complete agreement and the consent form was signed by the patient.
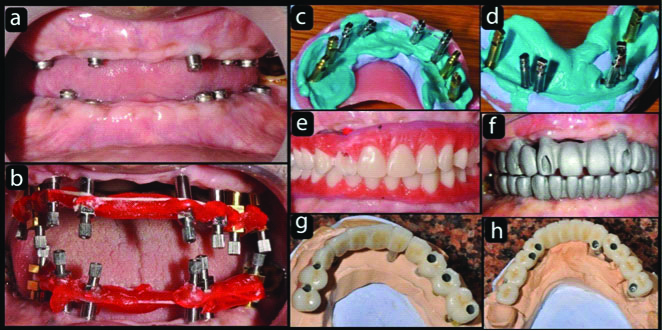
Impressions were made with an irreversible hydrocolloid material (Zhermack Tropicalgin Alginate, Italy). They were poured in type IV dental stone (Kalabhai Kalstone). Maxillo Mandibular Relation was recorded. Master casts were mounted on semi adjustable articulator (Bio Art Plus k7). The wax up of both arches with complete set of teeth till first molars was done. This was duplicated as surgical stent in vacuum form guides. The guides fabricated gave an orientation of each tooth in the edentulous arches. Each guide was prepared in such a way that palatal part of maxillary guide and lingual part of mandibular guide was removed in a way to visualise the orientation of implants in mouth during surgery and their respective position. It was decided to complete the surgery in two parts i.e., maxilla and mandible separately. The surgical procedure was same for both arches, one hour before; patient was kept on 2 gm Amoxycillin. After adequate anaesthesia, the flaps of each arch were reflected midcrestally because of abundance of keratinized gingiva. Naso palatine foramen was taken as an anatomical guide for ideal orientation of implants in maxilla. Further surgical guide of maxilla gave correct position of teeth. According to the manufacturer’s instructions, eight end osseous screw type implants (Bio horizon tapered internal, Birmingham, AL, USA) 3.4 mm to 3.8 mm in diameter and 10.5 mm to 12 mm in length were installed in maxilla, four were placed in inter canine region and two bilaterally in premolar and molar regions. Six implants (Bio horizon tapered internal) 3.4 mm to 3.8 mm in diameter and 10.5 mm to 12 mm in length were placed in mandible, two were placed in canine regions and two bilaterally in premolar and molar regions [Table/Fig-2a-e].
a) Soft tissue healing of the extraction wounds after six weeks; b) Nasopalatine foramen used as the guide for placement of implants in maxilla; c) Initial implants in maxilla parallel to guide in nasopalatine foramen; d) Implants in maxilla; e) Six Implants in mandible.
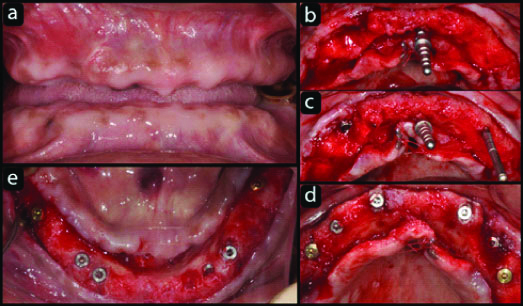
Narrow implants were used in both arches, keeping in mind the decreased vascularity and more bone formation around the abutment. Buccal bone grafting (Bio Oss, Geistlich Pharma AG, Wolhusen, Switzerland) in maxilla was done for biological and aesthetic reasons. Tension free flap closure was done by placing apical mattress suture (6-0 Coated Vicryl, Ethicon), 1 cm from the incision line. Amoxicillin clavulanic acid 625 mg thrice a day for 7 days, diclofenac sodium 100 mg twice a day were prescribed.
The patient was kept on recall every month and an interim complete denture was fabricated for the waiting period of four months.
Following radiographic confirmation of osseointegration, third surgical procedure was undertaken for healing caps on each implant in both arches [Table/Fig-3,4 and 5].
Eight Implants in maxilla (on right side the 2nd implant is hidden below the gingiva).
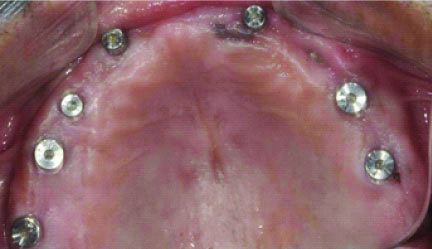
Six implants in mandible.

Four weeks later, impressions were taken with the addition silicone (Aquasil, Dentsply) of each arch. Impression posts were screwed on all the implants and splinted with resins (Pattern resin, GC Corporation, Japan) which were further checked with radiographs for the precise fit. Individual customised acrylic impression trays were used with open tray technique [Table/Fig-6a-d]. In clinical practice, correct positioning and precise recording of implants are essential for passive fit of the framework. Implant analogues were attached to the posts and the impressions were poured with type IV dental stone (Kalabhai Kalstone). Base plates were made from autopolymerising methacrylate material on the master cast. Holes were drilled for each of the implants position and occlusal rims (Occlusal rim wax, Coltene) were constructed on the base plates, maxillomandibular relations were estimated three dimensionally. Master cast were mounted on a semi adjustable articulator. Artificial teeth setting were done to demonstrate the dimension, location, position and occlusion of forthcoming fixed prosthesis. Dentofacial analysis was done keeping in mind lip support, smile line, incisal edges with lower lip, cervical level, ridge lapping and necessity for pink colour porcelain. A setup wax-up trial was done to evaluate the occlusal relation of definitive fixed prosthesis [Table/Fig-6e]. Castable abutments were used for screw type prosthesis for both arches with no cantilevers. Metal frameworks (d.Sign 30, Ivoclar Vivadent AG, Liechtenstein) were made in order to obtain adequate space for veneering ceramics [Table/Fig-6f]. Clinical try-in and passive fit of the segmental frameworks (three in maxilla and mandible, canine to canine, first premolar to molar each on either side) were verified by radiographs.
a) Frontal view with healing caps; b) Impression posts attached to the implants and stabilised with pattern resin; c) Upper Direct Impressions with customised Tray; d) Lower direct impressions with customised tray; e) Wax setup of teeth to check occlusion, phonetics and smile; f) Metal Framework Try in; g) Screw retained Metal ceramic maxillary prosthesis; h) Screw retained Metal ceramic mandibular prosthesis.
Interocclusal space for porcelain veneering which was analysed three dimensionally and bite registration records (DMG O Bite, Germany) were taken. Bisque trials of the segmental fixed retrievable prosthesis of both the arches were tried before glazing. Further corrections were made with centric, eccentric relations and interferences were eliminated. Finally, full mouth, segmental retrievable implant supported metal ceramic prosthesis were delivered [Table/Fig-6 g,h].
During the screwing, a complication was noted. Right side upper molar implant became loose. It could be an early implant failure which was due to fibro-osseous integration and the region of implant placement (posterior maxilla) were the density of the bone was least. It was removed and prosthesis was send back to the laboratory for new segmental prosthesis on right upper side. It was an advantage with segmental prosthesis. The new fabrication was replaced in very short time as no further tedious procedures were required.
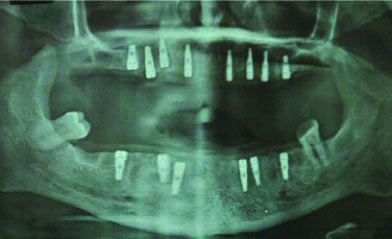
The prosthesis was screwed on the implants in mouth carefully starting from posteriors bilaterally. Each implant and abutment fit was verified by individual radiographs. Occlusion plays a major role in functional and biological aspects of full arch implant restorations. Mutually protected occlusal scheme was given to protect both anterior and posterior teeth in centric relation and canines guided the lateral excursive moment [Table/Fig-7a-d].
a) Maxillary and Mandibular segmental prosthesis in left lateral occlusal view; b) Maxillary and Mandibular segmental prosthesis in right lateral occlusal view; c) Frontal centric occlusion of Segmental Prosthesis; d) Postoperative OPG; e) Six Months Post OPG with replaced implant in right molar region.
*White patch evident on upper lateral incisor bilaterally. It is a follow-up view of the prosthesis depicting deterioration of composite restorations within one year
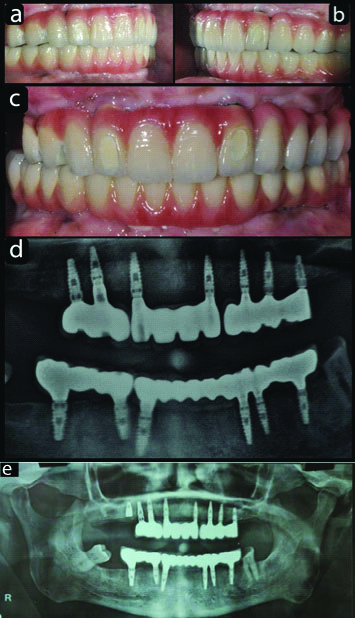
Final torque was given to each abutment screw after one week of satisfaction by patient report. Screw access holes were closed with teflon tape and resin composite material (Dyad Flow, Kerr Corporation, USA). Water Piks and Super Floss were advised to keep intaglio surface of prosthesis clean. Oral hygiene was reinforced with two times proper brushing with fluoride paste. Patient was kept on recall of three months initially. On one recall visit after a year there was substantial deterioration of the composite restorations especially on the labial surface of the maxillary prosthesis. This could have been avoided if ceramic inlays were used as plugs as they appear to be more predictable, aesthetic and successful method of sealing the screw access holes of screw retained implant restorations. After six months the loosened implant was replaced in right molar region [Table/Fig-7e]. Further, patient was followed for next two years and reported no complications like ceramic fracture, screw loosening or peri-implantitis.
Discussion
Complete edentulism is still a common health problem. A complete denture is a classical therapy for fully edentulism. But there are many problems associated with dentures. Insufficient chewing abilities, articulation problems, physiological strain and social impairment are some. There is multiple treatment for edentulous patients. Fortunately, the progress made by dental science, especially in the field of dental implants, offers many revolutionary treatment options for edentulous patients. Among these are full arch implant reconstructions, implant supported removable denture (overdenture) and combination of both solutions. Acceptance, circumstances and financial capacities are often priorities in decision making. Anatomic limitations and surgeon’s knowledge determined the procedure. Therefore, treatment goals should be based on clear concept and expertise [1].
Four or six implants, axial or divergent in each arch for removable and fixed prosthesis had been well accepted methods. Complications associated are often fracturing or detachment of acrylic teeth, porcelain chips, improper cantilevers and poor implant distribution [1]. In present case of an edentulous patient which was reconstructed with 8 implants in maxilla and six for mandible, the prosthesis were segmented and screw retained. The reason for selection of such prosthesis was no cantilever, easy retrievability, correction of prosthesis with divergent angulations of implants in maxilla and simplification of laboratory procedures. The rehabilitation of edentulism by means of fixed prosthesis has always been a priority. The restoration of edentulous maxilla using dental implants is often challenged by multiple factors that influence clinical decision making. Bone volume is remarkably low in maxilla as compared to mandible. Bone grafting, short implants, tilted implants along with extra alveolar implants may solve the problem with better clinical outcomes. However, implants survival in grafted bone had been repeatedly demonstrated to be lower than natural bone [2-6]. Zygomatic and pterygoid implants offer high implant survival but complications are high and additional training is required for appropriate utilisation of extra alveolar implants [7-9]. Thus, treatment with implant supported fixed prosthesis for maxilla is critically dependent upon initial clinical scenario. A minimum invasive surgery through pre fabricated surgical guides could be a better option for less morbidity in full arch treatment cases. However, flapless surgery requires sufficient bone volume and keratanized mucosa to avoid regenerative procedures [8,9].
In our case buccal aspect of maxillary ridge needed augmentation as the anterior sockets resorbs fast because of bundle bone loss. Therefore flap reflection was indicated to perform l bone regeneration.
Edentulous mandible with adequate bone height and width can be successfully restored with fixed implant supported prosthesis. A common strategy for edentulous mandible is installation of implants in inter foraminal region and a full arch fixed implant supported prosthesis with cantilever of distal extension [10-12]. However, this type of prosthesis can promote high level of stress that can be harmful to the patient and implants because of unfavourable arms [13]. This drawback led to the use of multiple implants in anterior and posterior mandible to further improve the distribution of stress with more favourable implant support [14]. Further, it was discussed that biomechanical effects of medial mandible flexure is accumulation of stress in implant supported restoration [15]. To counteract median mandibular flexure of mandible due to pterygoid muscle contraction, the segmental prosthesis is preferred [16].
In present case in mandible; the prosthesis till molars was extended to avoid cantilevers. It is suggested that using more implants with wider distribution in arches provide long term survival for complex reconstructions. Segmental maxillary supported fixed prosthesis survival is higher as suggested by systemic review [17]. Splinted prosthesis for restoration of edentulous maxilla are the issues that address divergent angulations of implants in anterior versus posterior maxilla. Laboratory procedure become easy and there is excellent passive fit of prosthesis. However, this type of prosthesis requires experienced team and comprehensive knowledge of surgical and restorative aspects of therapy following detailed pre-surgical analysis.
The shortcoming of the present case was the composite restorations which were used to close the buccal screw access holes that became unaesthetic in appearance in follow-up visits. The use of multi unit abutments instead of straight castable could have avoided the buccal access holes in maxillary anterior prosthesis. Further, the use of ceramic plugs instead of composite would have offered more longevity in terms of predictability and successful method for sealing screw access holes of implant retained prosthesis [18].
The segmented approach of prosthesis may be an alternative modality for full arch rehabilitation to avoid complications like chipping of veneered ceramic, implant failure and ease of repair.
Conclusion
The longevity of the rehabilitation should be the concern for the clinician. Segmented full arch prosthesis on implants may be a viable alternative for increased survival of the prosthesis without technical and biological complications.
[1]. Gallucci GO, Avrampou M, Taylor JC, Elpers J, Thalji G, Cooper LF, Maxillary Implant-Supported Fixed Prosthesis: A Survey of Reviews and Key Variables for Treatment PlanningInt J Oral Maxillofac Implants 2016 31:192-97.10.11607/jomi.16suppl.g5.327228251 [Google Scholar] [CrossRef] [PubMed]
[2]. Chiapasco M, Casentini P, Zaniboni M, Bone augmentation procedures in implant dentistryInt J Oral Maxillofac Implants 2009 24:237-59. [Google Scholar]
[3]. Becktor JP, Isaksson S, Sennerby L, Survival analysis of endosseous implants in grafted and nongrafted edentulousmaxillaeInt J Oral Maxillofac Implants 2004 19(1):107-15. [Google Scholar]
[4]. Esposito M, Grusovin MG, Felice P, Karatzopoulos G, Worthington HV, Coulthard P, The efficacy of horizontal and vertical bone augmentation procedures for dental implants-a Cochrane systematic reviewEur J Oral Implantol 2009 2(3):167-84. [Google Scholar]
[5]. Pjetursson BE, Tan WC, Zwahlen M, Lang NP, A systematic review of the success of sinus floor elevation and survival of implants nserted in combination with sinus floor elevationJ Clin Periodontol 2008 35:216-40.10.1111/j.1600-051X.2008.01272.x18724852 [Google Scholar] [CrossRef] [PubMed]
[6]. Rocchietta I, Fontana F, Simion M, Clinical outcomes of vertical bone augmentation to enable dental implantplacement: a systematic reviewJ Clin Periodontol 2008 35(8):203-15.10.1111/j.1600-051X.2008.01271.x18724851 [Google Scholar] [CrossRef] [PubMed]
[7]. Curi MM, Cardoso CL, Ribeiro Kde C, Retrospective study of pterygoid implants in the atrophic posterior maxilla: implant and prosthesis survival rates up to 3 yearsInt J Oral Maxillofac Implants 2015 30(2):378-83.10.11607/jomi.366525830398 [Google Scholar] [CrossRef] [PubMed]
[8]. Prithviraj DR, Vashisht R, Bhalla HK, From maxilla to zygoma: A review on zygomatic implantsJ Dent Implant 2014 4:44-47.10.4103/0974-6781.130973 [Google Scholar] [CrossRef]
[9]. Chrcanovic BR, Abreu MH, Survival and complications of zygomatic implants: a systematic reviewOral Maxillofac Surg 2013 17(2):81-93.10.1007/s10006-012-0331-z22562293 [Google Scholar] [CrossRef] [PubMed]
[10]. Gallucci GO, Benic GI, Eckert SE, Papaspyridakos P, Schimmel M, Schrott A, Consensus statements and clinical recommendations for implant loading protocolsInt J Oral Maxillofac Implants 2014 29:287-90.10.11607/jomi.2013.g4 [Google Scholar] [CrossRef]
[11]. Jacques LB, Moura MS, Suedam V, Souza EA, Rubo JH, Effect of cantilever length and framework alloy on the stress distribution of mandibular-cantilevered implant-supported prosthesesClin Oral Implants Res 2009 l 20(7):737-41.10.1111/j.1600-0501.2009.01712.x19489929 [Google Scholar] [CrossRef] [PubMed]
[12]. Sivaraman K, Chopra A, Venkatesh SB, Clinical importance of median mandibular flexure in oral rehabilitation: a reviewJ Oral Rehabil 2016 43(3):215-25.10.1111/joor.1236126498998 [Google Scholar] [CrossRef] [PubMed]
[13]. Kwon T, Bain PA, Levin L, Systematic review of short- (5-10 years) and long- term (10 years or more) survival and success of full-arch fixed dental hybrid prostheses and supporting implantsJ Dent 2014 42(10):1228-41.10.1016/j.jdent.2014.05.01624975989 [Google Scholar] [CrossRef] [PubMed]
[14]. Millen C, Brägger U, Wittneben JG, Influence of prosthesis type and retention mechanism on complications with fixedimplant-supported prostheses: a systematic review applying multivariate analysesInt J Oral Maxillofac Implants 2015 30(1):110-24.10.11607/jomi.360725615920 [Google Scholar] [CrossRef] [PubMed]
[15]. Castellon P, Blatz MB, Block MS, Finger IM, Rogers B, Immediate loading of dental implants in the edentulous mandibleJ Am Dent Assoc 2004 135(11):1543-49.10.14219/jada.archive.2004.008015622658 [Google Scholar] [CrossRef] [PubMed]
[16]. Zarb GA, Hobkirk J, Eckert S, Jacob R, Prosthodontic treatment for edentulous patients:complete dentures and implant-supported prostheses 2013 13th editionSt. Louis, Mo, USAMosby [Google Scholar]
[17]. Lambert FE, Weber HP, Susarla SM, Belser UC, Gallucci GO, Descriptive analysis of implant and prosthodontic survival rates with fixedimplant-supported rehabilitations in the edentulous maxillaJ Periodontol 2009 80(8):1220-30.10.1902/jop.2009.09010919656021 [Google Scholar] [CrossRef] [PubMed]
[18]. Mihali S, Canjau S, Bratu E, Wang HL, Utilization of ceramic inlays for sealing implant prostheses screw access holes: a case-control studyInt J Oral Maxillofac Implants 2016 31(5):1142-49.10.11607/jomi.473327632271 [Google Scholar] [CrossRef] [PubMed]