Rare Case of Symptomatic Ovarian Leiomyoma in Perimenopausal Woman
Vaibhav Kanti1, Vandana Verma2, Savita Agarwal3
1 Associate Professor, Department of Obstetrics and Gynaecology, Uttar Pradesh University of Medical Sciences, Saifai, Etawah, Uttar Pradesh, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, Uttar Pradesh University of Medical Sciences, Saifai, Etawah, Uttar Pradesh, India.
3 Associate Professor, Department of Pathology, Uttar Pradesh University of Medical Sciences, Saifai, Etawah, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vandana Verma, Flat 202, Type 4, Block C, New Campus, Uttar Pradesh University of Medical Sciences, Saifai, Etawah -206130, Uttar Pradesh, India.
E-mail: drvandana19@gmail.com
Leiomyoma is a very rare benign tumour to be found in ovary. Here, we report a case of 40-year-old perimenopausal women with large left ovarian mass. The Computerised Tomography (CT) showed left ovarian solid mass without ascites, right ovary was normal. Her CA125 level was 46 units/mL. Total abdominal hysterectomy with bilateral salpingo-oophrectomy was done. Histopathological findings were suggestive of ovarian leiomyoma. Since, it is very rare to be found in ovary so immunohistochemistry was done to confirm the diagnosis. Symptomatic ovarian leiomyoma is very rare but it should always be considered in the differential diagnosis of ovarian mass.
Desmin, Immunohistochemistry, Smooth muscle actin, Spindle cell tumour
Case Report
A 40-year-old perimenopausal patient with parity 3, presented to the hospital with complaint of bloating sensation in abdomen, indigestion and palpable mass in lower abdomen for 3.5 to 4 months. She also complained that the mass was gradually increasing in size. Her menstrual cycle was of 26-30 days, regular with normal flow for 5-6 days and there was no history of dysmenorrhea.
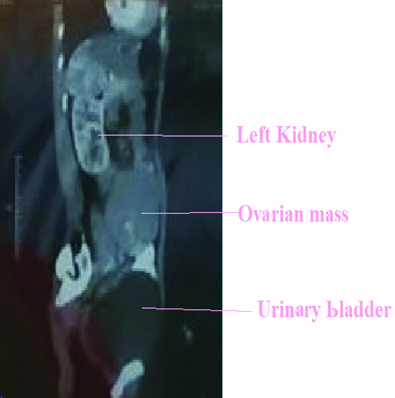
On examination, the patient was of thin built with mild pallor. Per abdominal examination revealed a firm, non tender mass of 9×8 cm extending in left iliac fossa, hypogastrium and umbilical region, with side to side mobility. On bimanual examination, uterus was normal size deviated to right side and a mass was felt through left fornix. The ultrasonography report showed irregular mass in left ovary, no ascites and normal sized uterus. CT [Table/Fig-1] showed left ovarian solid mass of 9×9 cm and no ascites. Right ovary was normal. The CA125 level was 46 units/mL.
CT scan whole abdomen showing ovarian mass (sagittal view).
On laparotomy no ascites was found, left ovarian mass with solid areas were present, uterus was of normal size and shape and the right ovary was normal. Total abdominal hysterectomy with bilateral salpingo-oophrectomy was done, after taking consent from the patient. Multiple deposits were present on pelvic peritoneum on left side. Rest of peritoneum, surface of liver, bowel, omentum, undersurface of diaphragm was normal. Biopsy was taken from peritoneal deposits. All the tissues were then sent for histopathological examination.
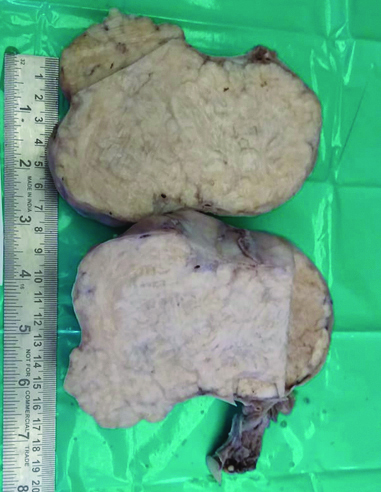
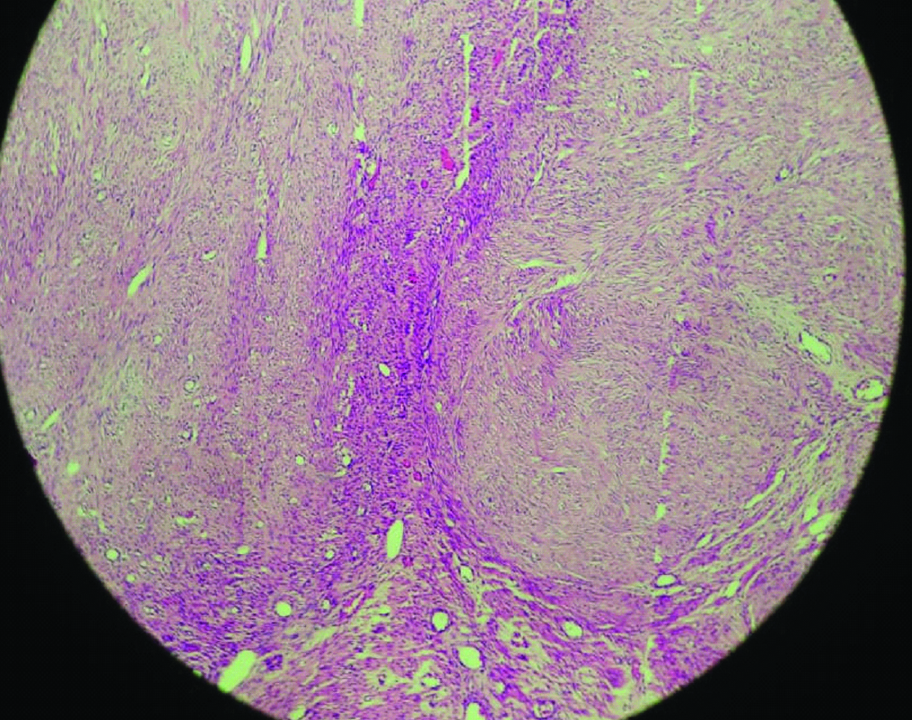
Cut section of left ovarian mass showed gray colour and was whorled in appearance [Table/Fig-2]. There was no area of hemorrhage and necrosis. Microscopic examination of tissues in left ovary showed interlacing fascicles of smooth muscle cells and these fascicles were separated by well vascularised connective tissue, there were no areas of mitosis, necrosis or atypia [Table/Fig-3]. Uterus showed small leiomyoma and in cervix chronic cervicitis was present. Peritoneal deposits showed leiomyomatosis.
Cut section of left ovarian mass showing gray colour and whorled appearance.
Microscopic picture showing interlacing fascicles of smooth muscle cells (H&E,100X).
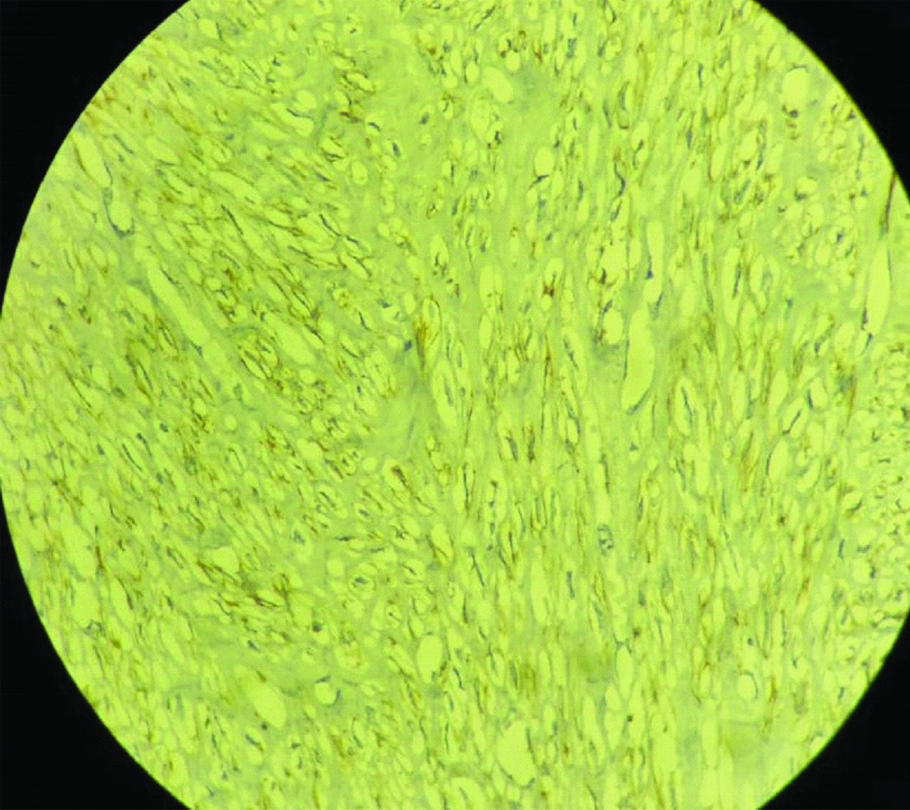
To confirm the diagnosis of ovarian leiomyoma immunohistochemistry was done, which was found positive for desmin and smooth muscle actin [Table/Fig-4].
Immunohistochemistry smooth muscle actin positive (400X).
Discussion
Leiomyoma is a very common benign tumour in uterus, but it is a rare one to be found in ovary. The prevalence of ovarian leiomyoma is very low and accounts only for 0.5 to 1% of all benign tumours of ovary [1]. They may be bilateral in paediatric age group or young adults but no bilateral leiomyoma of ovary is reported in age more than 35 years. Ovarian leiomyoma is seen in 78% cases of uterine leiomyoma and suggests the similar hormonal stimulation responsible for its occurrence [2]. Ovarian leiomyoma most probably arises from smooth muscle in ovarian hilar vessels but it may arise from cells present in ovarian ligament, smooth muscle cell in ovarian stroma, undifferentiated germ cells or metaplasia of cortical smooth muscle [3].
Mostly ovarian leiomyomas remain asymptomatic and they are found either during surgery or during autopsy. In symptomatic cases it presents as abdominal lump, pain in abdomen, hydronephrosis, elevated CA-125 or with Meigs’ syndrome [2]. Often it is difficult to differentiate ovarian leiomyoma with pedunculated uterine myoma, ovarian fibroma or even ovarian endometrioma, preoperatively [4].
Microscopically, it is difficult to differentiate ovarian leiomyoma and ovarian fibroma because in ovarian fibroma bundles of spindle shaped cells with pointed nuclei are seen which often exhibit storiform pattern, whereas in ovarian leiomyoma fascicular pattern of spindle shaped cells are found. Masson Trichrome is used to distinguish smooth muscle cells from fibrous tissue. Thecoma should also be differentiated from ovarian leiomyoma which is comprised of lipid laden theca cells in a fibrous stroma and in thecoma tumour cells are stained with oil red O [5].
Immunohistochemistry is used for confirmation of diagnosis in cases of doubt. Desmin, α-SMA (Alpha-Smooth Muscle Actin) and inhibin differentiate leiomyomas from fibromatous tumour. Ovarian leiomyoma shows diffuse desmin positivity whereas fibromatous tumours are typically negative or may show focal positivity for desmin. SMA is not very useful in differentiating thecoma and leiomyoma as sometime both may show positivity for SMA. Thecomas are strongly positive for α-inhibin and negative for SMA [2].
Taskin MI reported a case of ovarian leiomyoma that presented as infertility and abdominal pain and on transnaginal sonography right ovarian mass was found [6]. In contrast, Kataria SP et al., reported a case of 65-year-old female with backache. The ovarian leiomyoma in this case showed areas of adenofibroma like tissue in right ovary along with serous cyst adenoma in both ovaries [7].
Sanverdi I et al., also reported a case of ovarian leiomyoma in post hysterectomy patient of 52 years [8]. She had complaints of abdominal pain and bloating. Wang QM et al., reported a case of ovarian leiomyoma in 52-year-old post hysterectomy female that presented with abdominal mass and distension, which was similar to the index case [9].
Conclusion
Ovarian leiomyoma is a very rare tumour. However, we should always keep it in differential diagnosis of ovarian masses. On histopathology it should be differentiated from thecoma, fibroma, sclerosing ovarian tumour, etc. In these cases immunohistochemistry should be done to confirm the diagnosis.
[1]. Prajapati S, Meerabai V, Jayalakshmi M, Primary ovarian leiomyoma: A diagnostic dilemmaInternational Journal of Reproduction, Contraception, Obstetrics and Gynecology 2018 7(4):1645-47.10.18203/2320-1770.ijrcog20181372 [Google Scholar] [CrossRef]
[2]. Rajabi P, Hani M, Bagheri M, Mirzadeh F, Large ovarian leiomyoma in young womanAdv Biomed Res 2014 3:8810.4103/2277-9175.12800124761396 [Google Scholar] [CrossRef] [PubMed]
[3]. Tomas D, Lenicek T, Tuckar N, Puljiz Z, Ledinsky M, Kruslin B, Primary ovarian leiomyoma associated with endometriotic cyst presenting with symptoms of acute appendicnitis: A case reportDiagn Pathol 2009 4:2510.1186/1746-1596-4-2519642987 [Google Scholar] [CrossRef] [PubMed]
[4]. Koo YJ, Cho YJ, Kim JY, Lee JE, Kim ML, Kim JM, Ovarian leiomyoma as a potential cause of compromised fertilityFertil Steril 2011 95:112010.1016/j.fertnstert.2010.09.00720947074 [Google Scholar] [CrossRef] [PubMed]
[5]. Gunasekaran I, Phansalkar M, Palo LB, Varghese RG, Ovarian leiomyoma along with uterine leiomyomata: A common tumour at an uncommon siteJ Clin Diagn Res 2015 9(11):ED01-ED02.10.7860/JCDR/2015/13378.670326674537 [Google Scholar] [CrossRef] [PubMed]
[6]. Taskin MI, Ozturk E, Yildirim F, Ozdemir N, Inceboz U, Primary ovarian leiomyoma: A case reportInt J Surg Case Rep 2014 5(10):665-68.10.1016/j.ijscr.2014.07.02025194600 [Google Scholar] [CrossRef] [PubMed]
[7]. Kataria SP, Chawla N, Singh G, Kum S, Ovarian leiomyoma associated with serous cystadenoma- A case report of an uncommon entityGlobal J Pathol Microbiol 2014 14(4):38-42. [Google Scholar]
[8]. Sanverdi I, Vural F, Temizkan O, Temel O, Ayvaci H, Gunes P, Primary ovarian leiomyoma in a postmenopausal woman: A case reportNorth Clin Istanb 2016 3(3):222-24.10.14744/nci.2015.0737928275755 [Google Scholar] [CrossRef] [PubMed]
[9]. Wang QM, Zhao Y, Ma Y, Yao LT, Han X, One case report of giant atypical leiomyoma of the ovaryMedicine (Baltimore) 2018 97(40):e1252610.1097/MD.000000000001252630290610 [Google Scholar] [CrossRef] [PubMed]