Reconstruction of Extraoral Fistula of Dental Origin
Metin Berk Kasapoglu1, Gülşah Guven2, Sabri Cemil Isler3, Çetin Kasapoglu4
1 Senior Resident, Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Istanbul University, Istanbul, NA, Turkey.
2 Independent Researcher, Istanbul, NA, Turkey.
3 Associate Professor, Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Istanbul University, Istanbul, NA, Turkey.
4 Professor, Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Istanbul University, Istanbul, NA, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Metin Berk Kasapoglu, Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Istanbul University, Istanbul, NA, Turkey.
E-mail: mbkasapoglu@gmail.com
Odontogenic extraoral fistulas often lead to intense levels of patient discomfort and incidence of complications, which are relieved by treatment. However, the cosmetic outcome following treatment may not meet the expectations of the patient. A 51-year-old male presented with a chronically draining lesion on his left cheek. Clinical examination revealed necrosis in the mandibular left first molar and a panoramic radiograph demonstrated periapical abscess surrounding the root apex. A diagnosis of extraoral fistula of odontogenic origin was made, and the affected tooth was extracted. The extraoral fistula disappeared but the defect on the cheek exhibited no improvement over the 2 month follow-up period. Surgical revision of the defect was therefore necessary. A Limberg flap was designed and then transposed to the defect region, followed by primary closure of the donor region. The 6-month follow-up visit revealed satisfactory results for both the patient and the surgeon. This manuscript is the first case report focusing on residual defect elimination of an extraoral fistula with the use of a transpositional flap in the cheek region.
Cosmetic surgery, Extraoral sinus tract, Limberg flap, Periapical abscess
Case Report
A 51 years old male was referred to the Department of Oral and Maxillofacial Surgery, due to a purulent discharge from a skin fistula on his left cheek [Table/Fig-1]. The patient reported that he had already undergone two surgical interventions for removal of the fistula. However, the scar tissue failed to heal after the second surgery.
Photograph showing clinical appearance of the draining lesion on the left cheek (Arrow: lesion on the soft tissue).

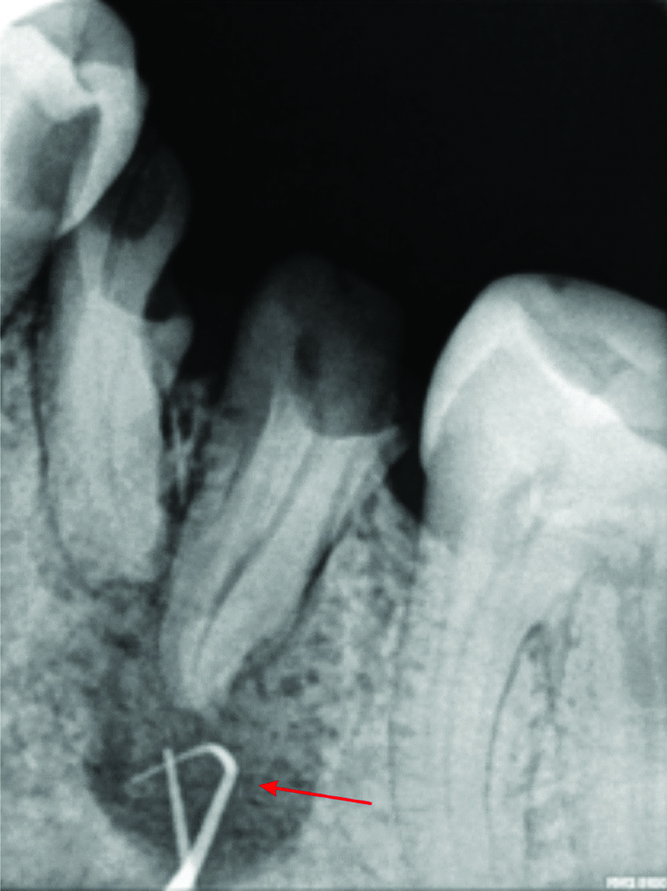
On extraoral examination, a skin fistula located 2 cm above the inferior border of the mandible was noted. Intraoral and radiographic examinations revealed necrosis in tooth 36 and a periapical radiolucent lesion associated with the distal root apex [Table/Fig-2]. A periapical radiograph was acquired with a gutta-percha point inserted into the fistula, which confirmed that the fistula led to the distal root of the first molar [Table/Fig-3,4]. Based on these findings, the left mandibular first molar was extracted and the periapical lesion was curetted. The extra oral fistula disappeared but after 2 months of follow-up, the defect on the cheek had not improved; moreover, the patient considered the defect aesthetically objectionable. As the defect was too large for primary closure, insertion of a rhombic flap (which is useful in the treatment of medium to large-size defects) was planned. It was designed with sides of the same length as the short axis of the rhomboid defect and is designed to lie in parallel with relaxed skin tension lines. After the Limberg flap was designed, the patient was administered local anaesthesia (2% articaine, 1:200 000 epinephrine, 2 mL) and the excision was performed using a rhombus with 60° and 120° angles [Table/Fig-5]. The flap was then transposed to the defect and the donor area was primarily closed [Table/Fig-6]. The six-month follow-up visit revealed satisfactory results [Table/Fig-7].
Panoramic radiograph indicating a periapical lesion associated with the first molar (Arrow: Periapical lesion of tooth 36).

Photograph showing insertion of gutta perchas extra-orally to the fistule.

Periapical radiograph showing gutta perchas in the the sinus tract reaching the distal root of the lesion (Arrow: tip of gutta percha reaching the lesion).
Incision of the Limberg flap.

Suturing following transposition of the Limberg flap.

Appearance at 6 months after closure.

Discussion
Odontogenic extraoral fistulas are seldom periodontal in origin, although the aetiologic factor is typically a periapical infection. These fistulas generally occur in the mandible [1]. In the present case, the aetiologic factor, necrosis in tooth 36 and localisation of the fistula, on the soft tissue covering the mandible, was concordant with previous reports [1-3]. These fistulas are often misdiagnosed. On the basis of their clinical appearance, they can be confused with traumatic lesions, bacterial and fungal infections, squamous cell carcinoma, congenital fistulas and foreign bodies [4,5]. Before the correct diagnosis can be made, such patients often undergo multiple surgical excisions and biopsies and receive many courses of antibiotics. Unless the dental aetiology is eliminated, these fistulas recur, as in the present case [4-6].
Radiographic findings are also important. In such cases, the dental aetiology can be confirmed by tracing the fistulous tract to its origin with gutta-percha during the radiographic examination [2,6].
Either root canal therapy or surgical extraction can be used to treat the affected tooth. Thereafter, spontaneous closure of the tract should occur within 5-14 days. If the remaining defect is deemed to be cosmetically unacceptable, it can be revised surgically [7]. When the defect is too large for primary closure, a local flap may be used to close it [8]. The Limberg flap, which is easy to apply, is commonly used to reconstruct a rhombic defect. It can be used to close defects almost anywhere on the body [9]. It is multi-directional, in that, a random pattern flap can be raised from all corners of the rhomboid. The defect is filled with a tissue of the same thickness and colour, and with good vascularity [9,10].
Another advantage of the flap is that it can be designed in several directions, allowing surgeons to select the orientation; we, therefore, selected this technique [11]. Although satisfactory results were achieved in 6 months, one limitation of this study should be noted. The patient did not attend his routine visits; thus, observations after 6 months could not be recorded. The authors believe that long-term recovery observations can reveal more significant results for such cases.
Conclusion
If the scar tissue associated with the fistula does not resolve over the course of a 2-month follow-up, it can be surgically reconstructed. The goal of reconstruction should be to achieve the best possible medical and cosmetic result. This can be accomplished only by proper surgical planning.
Patient consent: Written informed consent for publication has been obtained from the patient.
[1]. Barrowman RA, Rahimi M, Evans MD, Chandu A, Parashos P, Cutaneous sinus tracts of dental originMed J Aust 2007 186(5):264-65.10.5694/j.1326-5377.2007.tb00886.x17391091 [Google Scholar] [CrossRef] [PubMed]
[2]. Sheehan DJ, Potter BJ, Davis LS, Cutaneous draining sinus tract of odontogenic origin: Unusual presentation of a challenging diagnosisSouth Med J 2005 98(2):250-52.10.1097/01.SMJ.0000129936.08493.E015759963 [Google Scholar] [CrossRef] [PubMed]
[3]. Ozdemir A, Guven G, Dilsiz A, Sencimen M, Diagnosis and treatment of mandibular extraoral sinus of periodontal origin in a 9-year-old boy: A case reportJ Indian Soc Pedod Prev Dent 2008 26(Suppl 2):S76-78. [Google Scholar]
[4]. Soares JA, De Carvalho FB, Pappen FG, Araújo GS, De Pontes Lima RK, Rodrigues VMT, Conservative treatment of patients with periapical lesions associated with extraoral sinus tractsAust Endod J 2007 33(3):131-35.10.1111/j.1747-4477.2007.00058.x18076581 [Google Scholar] [CrossRef] [PubMed]
[5]. Pasternak-Júnior B, Teixeira CS, Silva-Sousa YTC, Sousa-Neto MD, Diagnosis and treatment of odontogenic cutaneous sinus tracts of endodontic origin: three case studiesInt Endod J 2009 42(3):271-76.10.1111/j.1365-2591.2008.01519.x19228218 [Google Scholar] [CrossRef] [PubMed]
[6]. Nakamura Y, Hirayama K, Hossain M, Matsumoto K, A case of an odontogenic cutaneous sinus tractInt Endod J 1999 32(4):328-31.10.1046/j.1365-2591.1999.00233.x10551125 [Google Scholar] [CrossRef] [PubMed]
[7]. Rohrer TE, Nguyen TH, Cook JL, Mellette JR, Migden MR, Flaps and Grafts in Dermatologic Surgery 2007 1st EdPhiladelphia, PAElsevier [Google Scholar]
[8]. Jovanovi MD, Coli MM, Design of the limberg flap by a specially designed ruler: A personal approachPlast Reconstr Surg 2004 113(2):653-58.10.1097/01.PRS.0000101534.00262.C614758230 [Google Scholar] [CrossRef] [PubMed]
[9]. Imran D, Koukkou C, Bainbridge LC, The rhomboid flap: A simple technique to cover the skin defect produced by excision of a mucous cyst of a digitJ Bone Joint Surg Br 2003 85(6):860-62.10.1302/0301-620X.85B6.1406112931806 [Google Scholar] [CrossRef] [PubMed]
[10]. Chasmar LR, The versatile rhomboid (Limberg) flapCan J Plast Surg 2007 Summer 15(2):67-71.10.1177/22925503070150020719554188 [Google Scholar] [CrossRef] [PubMed]
[11]. Singh A, Singh G, Earlobe reconstruction using a Limberg flap in six earsBr J Plast Surg 2003 56(1):33-36.10.1016/S0007-1226(03)00002-X [Google Scholar] [CrossRef]