The term NAFLD encompasses a spectrum of hepatic disorders ranging from simple benign steatosis to steatohepatitis with the potential to progress to cirrhosis together with its inherent complications such as liver failure or cancer [1]. The clinical condition was first defined by Ludwig in a seminal paper in 1980 [2]. Histologically, NAFLD, is defined as the excessive accumulation of fat in the cytoplasm of more than 5% of the hepatocytes or more than 5% of the weight of liver, without a history of significant alcohol abuse (<20 g/day in women, <30 g/day in men,) or any other aetiologies of chronic liver disease that leads to steatosis. This steatosis when accompanied by periportal and lobular inflammation is referred to as Non-Alcoholic Steatohepatitis (NASH) [3].
Globally, the prevalence of NAFLD has reached pandemic proportions paralleling the increase in associated conditions of obesity, hyperlipidaemia and Type 2 Diabetes Mellitus (T2DM) [4]. In the Asian sub-continent, the figures are approximately 9%-40% and in India, the prevalence ranges from 5%-28% depending upon the socio-demographic, genetic and lifestyle factors [5-12]. The risk factors of the disease include male gender, increasing age, truncal obesity, and other biochemical and metabolic alterations [13]. The disease overall can be described as the hepatic manifestation of the MetS and IR has been shown to be the key pathogenic mechanism in the development of the disease.
The gold standard for the diagnosis of NAFLD is liver biopsy; however it has limited usage due to high risk of complications and sampling bias. In clinical settings, non-invasive markers such as evaluation of serological indices and imaging methods are often used for the diagnosis of NAFLD. Currently, ultrasound and estimation of liver enzymes are the most widely used methods for detecting NAFLD because of their low cost and high accuracy, but they fail to detect <10% steatosis of hepatocytes. Based on these findings, the present study was designed to assess the diagnostic utility of the surrogate markers of IR and their association with biochemical profile of liver function in ultrasonographically diagnosed cases of NAFLD.
Materials and Methods
This cross-sectional clinic-based study was carried out at College of Medicine and Sagore Dutta hospital (CMSDH), a Tertiary Care Hospital and Teaching Institute in Kolkata, West Bengal, India. All the patients attending the Radiology Department at CMSDH from May 2017-May 2018 and showing evidence of fatty liver on ultrasonography were included in the study. The study was carried out in accordance with the guidelines of the Institutional Ethics Committee (Registration No.: ECR/1210/Inst/WB/2019 issued under Rule 122 DD of the Drugs and Cosmetics Rules, 1945) at the College of Medicine and Sagore Dutta Hospital.
The ultrasonography was performed on all participants using a Samsung H 60 ultrasound machine with C2-8 MHz transducer. Patients with osmotic symptoms, history of ketosis, weight loss of more than 3 kg in the preceding 3 months, microvascular complications, recent (within one year) myocardial infarction, acute coronary syndrome, stroke, other co-morbidities (cancer, renal failure, etc.,), alcohol consumption (the critical threshold being <20 g/day in women, <30 g/day in men,), known liver disease, viral hepatitis, steatogenic medication, parenteral nutrition, and three-fold raised alanine aminotransferase were excluded from the study. Apparently, healthy age and sex-matched 100 individuals without any history of alcohol consumption and showing no evidence of fatty liver on ultrasonography and normal liver enzymes were selected as controls.
After obtaining written informed consent, 5 mL overnight fasting blood samples were collected. Detailed history of the 116-patients including information of alcohol consumption (regarding the quantity consumed) was recorded.
Anthropometric parameters like weight and waist circumference (in cm) were measured. For measurement of weight (in kg), the subject was asked to remove all heavy clothing, shoes and accessories. The waist circumference was measured from the mid-point between the lowest rib and the iliac crest using a non-elastic flexible tape in horizontal position, at the end of normal expiration, in the fasting state, with the subject standing erect and looking straight forward and observer sitting in front of the subject.
All reagents used were supplied by ERBA and were procured by the government resources. Blood samples were analysed for glucose levels (ERBA- cat. no. 120266), fasting insulin, HbA1C (ERBA- cat. no. 50.47), lipid profile (cholesterol ERBA- cat. no. 121021, triglycerides ERBA- cat. no. 121024, HDL- ERBA- cat. no. 120706, LDL-ERBA- cat. no. 120707, and liver enzymes namely the transaminases, AST (cat. no. 120272) and ALT (ERBA- cat. no. 120271). Glucose oxidase-peroxidase (GOD-POD) method was used for estimation of blood glucose levels, the transaminases were estimated by the modified IFCC method and the lipid profile parameters were measured as per manufacturer’s instructions using ERBA EM360 Transasia autoanalyser [14-19]. The glycosylated haemoglobin was measured by the HB vario analyser (HPLC) supplied by Transasia. Serum fasting insulin was assayed using Calbiotech Insulin Eliza kit and LISA Scan Elisa reader, and the HOMA-IR was calculated (as a surrogate marker of IR) by the formula HOMA-IR=Fasting insulin x fasting glucose/22.5 [20].
Statistical Analysis
Data was presented as Mean±SD analysed by Statistical Package for Social Sciences (SPSS Inc., Chicago) version 20.0.
The anthropometric and biochemical data of the cases and controls were analysed using the ANOVA for parameters following a normal distribution and Kruskal-Wallis or Wilcoxon Rank Sum for parameters following non-normal distribution. To identify the association of various risk factors (independent variables) of NAFLD (dependent variable), multivariate analysis was performed using logistic regression. Apart from the descriptive statistics, analysis of variance tests was carried out among cases and controls. The p-value <0.05 was considered statistically significant. ROC curves were generated to identify the cut-off values of HOMA-IR, AST, ALT, the AST/ALT ratio and fasting triglycerides to predict the existence of fatty liver. Adjusted OR was also calculated to measure the independent effect of the risk factors.
Results
Statistical analysis of the anthropometric and biochemical data of the cases and controls revealed statistically significant difference in HbA1c, insulin, HOMA -IR, AST, ALT, AST/ALT ratio, total cholesterol, HDL cholesterol and triglycerides among the cases and controls [Table/Fig-1].
Anthropometrical and biochemical parameters of the cases and controls.
| Parameter | Cases (n=116) | Controls (n=100) | p-value |
|---|
| Body weight (kg) | 59.77±9.91 | 57.41±14.88 | 0.18 |
| Waist circumference (cm) | 79.47±9.53 | 78.88±10.03 | 0.67 |
| Fasting glucose (mg/dL) | 111.26±38.94 | 113.30±40.72 | 0.72 |
| HbA1c (%) | 6.0±1.03 | 5.62±1.43 | 0.030* |
| Insulin (microIU/L) | 6.16±4.68 | 2.62±3.78 | 0.033* |
| HOMA-IR | 2.09±4.36 | 1.72±0.99 | 0.049* |
| AST (IU) | 33.47 | 36.71 | 0.015* |
| ALT (IU) | 42.54 | 31.26 | 0.00001** |
| AST/ALT ratio | 0.78±0.41 | 1.628±1.85 | 0.012* |
| Total cholesterol (mg/dL) | 187.94±44.04 | 177±43.91 | 0.0098 |
| HDL cholesterol (mg/dL) | 47.5±84.67 | 51.3±13.55 | 0.010 |
| Triglycerides (mg/dL) | 176.99±8.68 | 142.24±60.37 | 0.00008** |
| LDL cholesterol (mg/dL) | 111.85±28.99 | 116.8±31.17 | 0.27 |
HOMA-IR: Homeostatic model assessment for insulin resistance; HbA1c: Glycated haemoglobin; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; HDL cholesterol: High density cholesterol; LDL cholesterol: Low density cholesterol. ANOVA was performed for body weight, waist circumference, fasting glucose, Insulin, HOMA-IR. Wilcoxon Rank Sum was performed for liver enzymes and parameters of the lipid profile. *p-value <0.05 statistically significant; **p-value <0.001 statistically highly significant
Using Receiver operating characteristic (ROC) analysis, the cut-off for (HOMA-IR) to predict the possibility of existence of fatty liver was observed to be 0.79-0.92 with 63.27% sensitivity and 93.94%specificity [Table/Fig-2].
Receiver operating characteristic (ROC) curve to identify the cut-offs for HOMA-IR in order to predict the existence of fatty liver.
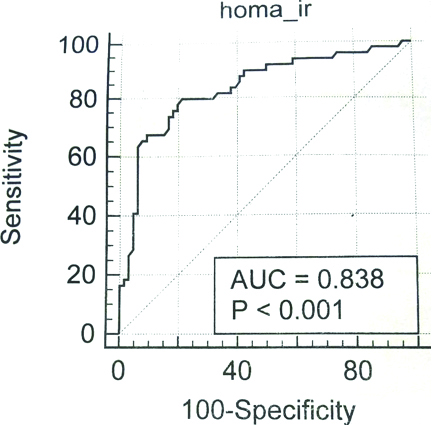
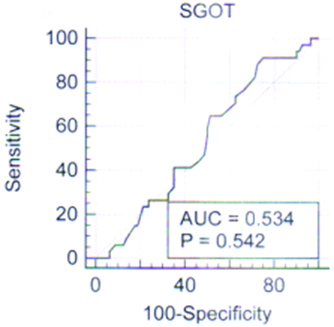
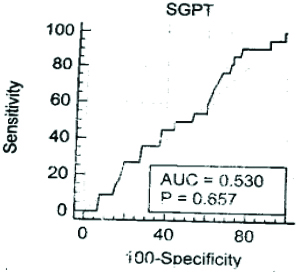
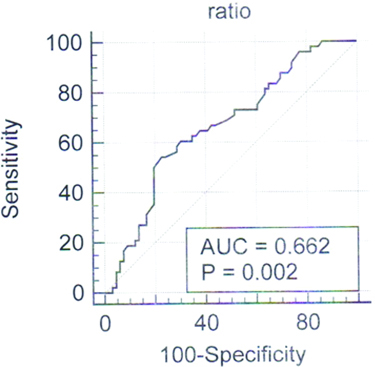
As evident from the curves, SGOT (AUC ROC=0.534) and SGPT (AUC ROC=0.530) individually are poor discriminants and cannot be used to predict the existence of fatty liver. But the ratio of AST/ALT fares slightly better. At 0.74, the ratio has a specificity of 65.15% and a sensitivity of 62.50% (AUC ROC=0.662, 95% CI 0.568-0.748) [Table/Fig-3,4 and 5].
Receiver operating characteristic (ROC) curve to identify the cut-offs for SGOT (AST) in order to predict the existence of fatty liver.
Receiver operating characteristic (ROC) curve to identify the cut-offs for SGPT (ALT) in order to predict the existence of fatty liver.
Receiver operating characteristic (ROC) curve to identify the cut-offs for AST/ALT ratio in order to predict the existence of fatty liver.
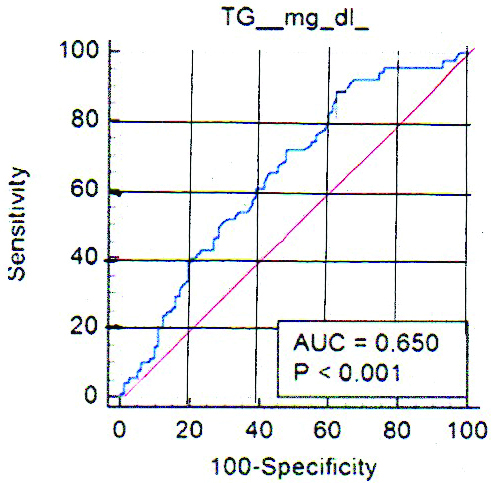
The ROC curve generated for triglygerides has a similar discriminating ability. The AUC ROC being 0.650, 95% CI .0.573-0.721. At Triglyceride ≥137 mg/dL, there is 60.67% sensitivity and 60.98% specificity to predict the existence of fatty liver [Table/Fig-6].
Receiver operating characteristic (ROC) curve to identify the cutoff of triglyceride in order to predict the existence of fatty liver.
Multivariate logistic regression analysis was performed among the various biochemical parameters in order to determine their association with NAFLD in this population. Cholesterol, triglycerides and HDL were found to be the chief variable associated with insulin in the population under study.
For HOMA-IR >2.5, the relative risk was 5.56 and the odds ratio was 7.15. For triglycerides >150 mg/dL, the relative risk was 1.88 and the odds ratio was 2.87.
Discussion
In this study, the levels of IR in patients who were sent for ultrasonography with a clinical suspicion of fatty liver were assessed. Statistical analysis of the data revealed statistically significant difference in insulin (p=0.033), HbA1C (p=0.030) and HOMA-IR (p=0.049), fasting triglycerides (p<0.001) total cholesterol (p=0.01) and HDL cholesterol (p=0.01) among cases and controls. Fasting triglyceridemia is one of the surrogate markers of IR along with HOMA-IR. It may be interesting to note that though the mean AST and ALT was comparable among cases, mean ratio of AST/ALT among the cases is 0.78 while that among controls it is as high as 1.63 and the difference was statistically significant (p-value=0.012). Receiver operating curves were generated, and HOMA-IR ≥2.9 and triglyceride ≥137 mg/dL were identified as cut-offs that may be used to predict the existence of fatty liver.
A closer look at the statistics reveals that the biochemical parameters of the cases are similar to the metabolic risk factors outlined in ATP III guidelines [13]. These metabolic risk factors included BMI >25 kg/m2 and/or waist circumference more than 102 cm in males or 88 cm in females, arterial hypertension (systolic blood pressure of 130 mm Hg or more or diastolic pressure 85 mm Hg or greater), fasting serum glucose of 110 mg/dL or greater, serum fasting triglycerides of 150 mg/dL or greater, HDL cholesterol level less than 40 mg/dL in men and less than 50 mg/dL in women. In the present study, the fasting blood glucose was 112 mg/dL, triglycerides 177 mg/dL and HDL 48 mg/dL in the cases. These findings were various studies on NAFLD patients with characteristics of MetS [20,21].
NAFLD is frequently associated with hypertension, atherosclerosis, DM and even CVD [22]. The cut-offs determined for HOMA-IR and triglycerides by generation of ROC curves were in agreement with Jain V et al., study [23]. The cut-off value for HOMA-IR in our study was 2.9 while some studies report value of 2 or 2.5. At lower values <2.9, there was loss of specificity without any significant gain in sensitivity, thus it can be concluded that 2.9 would be the best estimate to predict the existence of fatty liver in this population. Our findings indicate the appearance of IR in these patients prior to any significant elevation of liver transaminases. This early appearance of peripheral IR itself leads to steatosis in the healthy liver in the early stages of the disease. This increased IR leads to increased transport and deposition of fatty acids from the adipose tissue to the liver, making it more vulnerable to further oxidative stress and inflammatory responses of cytokine like TNF-α. At the molecular level, chronic stimulation of Ikinase β_(IKKβ) followed by continuous activation of NF-Kβ leads to alteration in phosphorylation of serine rather than in tyrosine of Insulin Receptor Substrate (IRS)-1 and becomes the central step in disruption of intracellular insulin signaling [24]. This in turn leads to exacerbation of IR, oxidative stress and finally organelle dysfunction that results in hepato-cellular degradation and fibrosis [25].
The presence of excessive fat in the liver or hepatic steatosis impedes the clearance of insulin resulting in hyperinsulinemia which is a feature of the pre-diabetic state. Studies shows that hepatic fat content correlates with the features of insulin resistance even in patients misdiagnosed by standard clinical evaluation [26,27]. The hepatic fat content correlates not only with hepatic IR but also with muscle and adipose tissue IR and has been described as the central pathogenic event in development of the MetS. Seppala-Lindroos A et al., postulated that the presence of hepatic steatosis itself has been described as a marker of multiorgan IR independent of BMI and intra-abdominal obesity [28]. Targher G et al., reported that visceral adiposity mediates endocrine abnormalities as well since the abdominal fat [29]. Hyperinsulinemia decreases the APO-B100 resulting in decreased export of triglycerides, and increased lipolysis eventually results in hepatic steatosis in these patients. In addition to being esterified to triacylglycerols, the presence of free fatty acids together with endoplasmic stress, oxidative stress and cytokine mediated stresses initiates hepatocyte apoptosis and progressive liver damage in susceptible individuals [30].
The most common cause of elevation of liver transaminases is perhaps NAFLD [31]. Typically, the disease is associated with minor elevations in liver transaminases, about 1.5-5 fold [32]. In view of the fatal consequences of MetS, the appearance of IR prior to any significant elevation of transaminases in our study population merits some consideration. One of the reasons for this biochemical picture may be that the normal baseline values of liver transaminases in the study population were significantly lower, and slight elevation in levels of transaminases are often overlooked [33]. In addition, these patients, though in the prediabetic state are actually in a very early stage of development of IR.
Chen ZW et al., reported strong correlation between the degree of steatohepatitis and levels of ALT [34]. ALT is almost exclusively present in the liver as against AST, which is also present in the heart and skeletal muscle. In the beginning, when the subject is still in the primordial stages of development of IR, the serum ALT levels may actually be normal which gradually increases with acquisition of visceral adiposity and leaving behind an unfavourable “metabolic memory” in the process. The high incidence of NAFLD associated MetS and high mortality rates makes it essential to detect and recognise the inherent developing IR. In view of the ongoing epidemics of obesity and diabetes, it is of paramount importance that the treating physician should check the fasting glucose, lipid profile and if possible, the fasting insulin in patients with evidence of fatty liver in USG irrespective of the changes in levels of liver transaminases, and advise proper lifestyle modification and therapeutic intervention.
Limitation
There are two major limitations of the study. Firstly, there was no facility to perform fibroscan in the Institute, and therefore the degree of liver fibrosis could not be quantified. Secondly, the sample size was relatively small. Further studies with calculated sample sizes are required to extrapolate the results to the general population.
Conclusion
The cut-off for HOMA-IR was found to be 2.9 and triglycerides 137 mg/dL to predict the existence of fatty liver. IR was observed before the elevation of transaminases, thus making further investigation for detection of pre-diabetic or diabetic state essential. In view of the ongoing epidemics of obesity and diabetes, it is of paramount importance that the treating physician should check the fasting glucose, lipid profile and if possible, the fasting insulin in patients with evidence of fatty liver in USG irrespective of the changes in levels of liver transaminases, and advise proper lifestyle modification and therapeutic intervention.
HOMA-IR: Homeostatic model assessment for insulin resistance; HbA1c: Glycated haemoglobin; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; HDL cholesterol: High density cholesterol; LDL cholesterol: Low density cholesterol. ANOVA was performed for body weight, waist circumference, fasting glucose, Insulin, HOMA-IR. Wilcoxon Rank Sum was performed for liver enzymes and parameters of the lipid profile. *p-value <0.05 statistically significant; **p-value <0.001 statistically highly significant