Management of oral leukoplakia should begin with elimination of predisposing habits. Several treatment modalities have been proposed for the treatment of Leukoplakia. Excision of precancerous oral lesions using LASER offers comparative advantages over traditional scalpel excision. These advantages include homeostasis, precision in removal, good patient acceptance, low morbidity and reduced postoperative complications. In the present case, patient reported minimal intraoperative and postoperative discomfort and the wound healing was also satisfactory.
Case Report
A 40-year-old male patient reported to the department of Dental Surgery, Moti Lal Nehru Medical College, Prayagraj with chief complaint of a white patch on his left cheek since 2 years. There was no similar family history and no history of trauma or surgery. The patient’s medical and dental histories were non-contributory. Patient reported habit of smoking tobacco, 1 pack of bidi (25 bidis) per day from past 5 years.
On clinical examination, a solitary white patch with a wrinkled surface and irregular margins was visible on the left buccal mucosa extending from the second molar to the first premolar, measuring approximately 4 cm posterior-anteriorly and 1.5 cm superio-inferiorly in dimensions. It was not tender on palpation. The lesion was non scrapable and was having crack mud appearance, the surrounding mucosa appeared to be normal [Table/Fig-1].
Intraoral view showing characteristic white patch with “crack mud” appearance on the left buccal mucosa characteristic of homogenous Leukoplakia.

The differential diagnosis which was kept in consideration was candidiasis as the lesion was non scrapable so, was ruled out. Another possibility of leukoedema and reticular lichen planus were also excluded due to its unilateral nature, did not disappear on stretching, absence of white striae. There was a negative history of genodermatoses, thus white sponge nevus was also not considered. After excluding the presence of any local chronic irritation and trauma in the area around the patch, frictional keratosis was omitted after working on differential diagnosis. On the basis of clinical history a provisional diagnosis of Homogenous Leukoplakia was made.
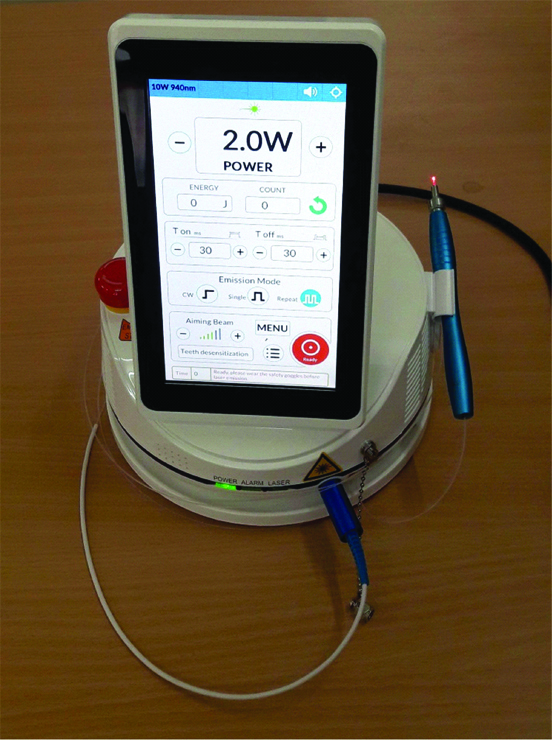
Patient counselling was done and the patient was asked to completely quit the habit of smoking tobacco. The patient was kept on antioxidants for 1 month duration. The patient did not respond to conservative medical management after a month so he was advised complete excision of the lesion using LASER. Routine Blood investigations were advised. The complete procedure was explained to the patient and an informed written consent was obtained. On the day of surgery, local anesthetic was infiltrated around the lesion. The lesion was excised using 940 nm Diode LASER (Faith Innovations) [Table/Fig-2]. All protective measures were taken while performing the LASER surgery. The procedure was performed in a closed operatory with controlled access and a laser hazard warning sign was placed at the entrance, all the operating staff in the operatory including the operator, assistant and patient were wearing protective eye wear, unnecessary reflecting objects were avoided from the path of the beam and adequate suction was provided in the operating field.
940 nm Diode LASER (Faith Innovations).
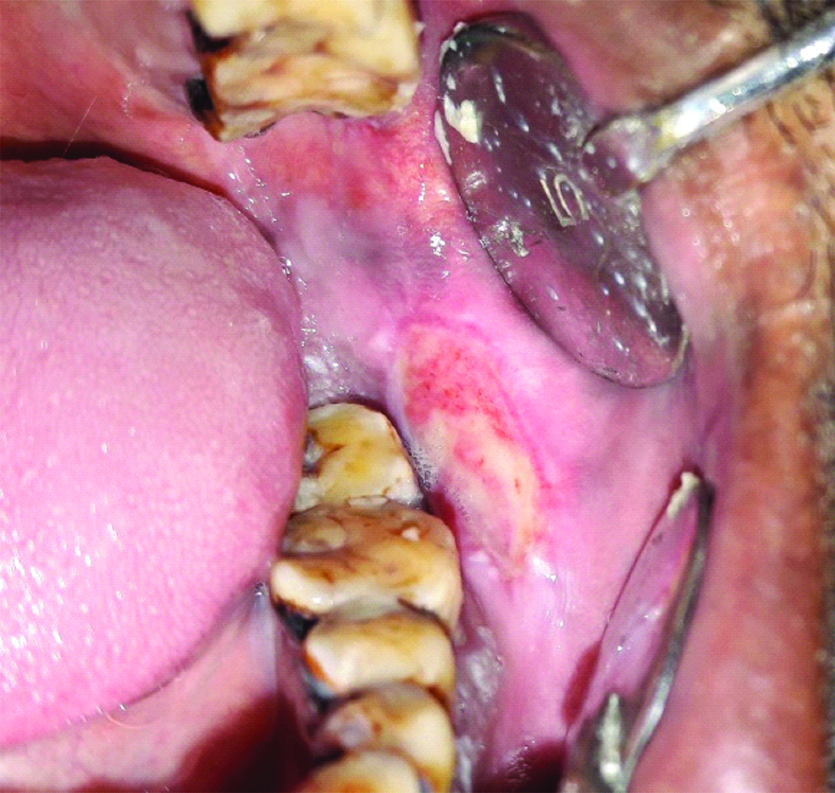
LASER beam was used in continuous mode in a paint brush manner. The LASER tip was used in direct contact mode with tissue to be ablated. The wound was left to heal by secondary intention [Table/Fig-3].
Immediate postoperative view showing excision of the lesion using Diode LASER.

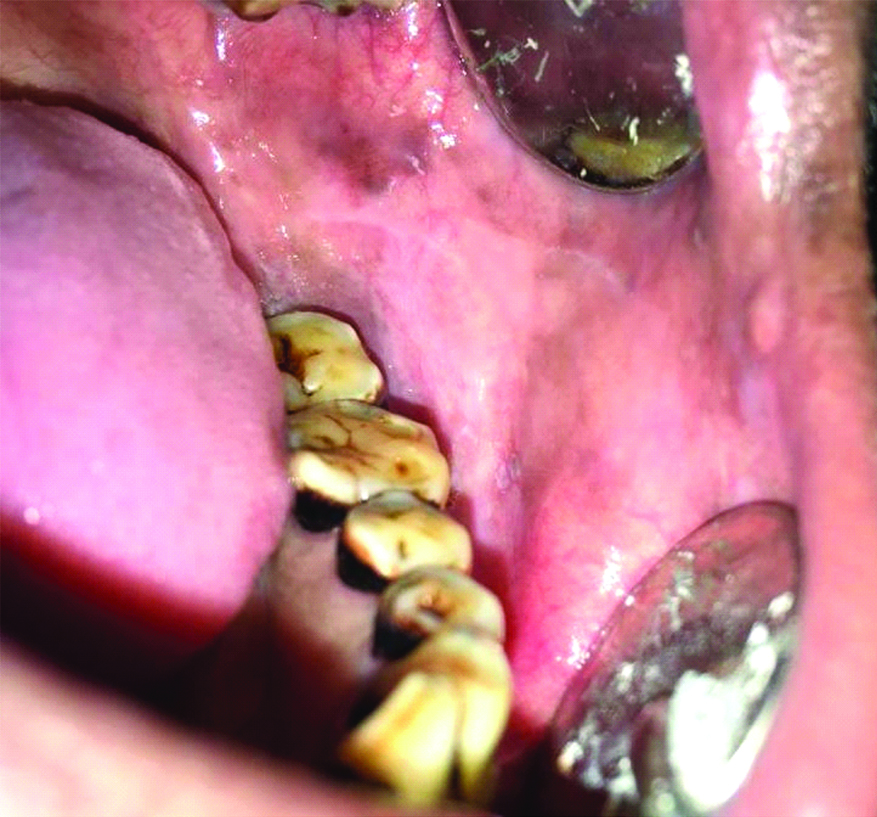
The patient was advised to take capsule amoxicillin 500 mg tds. and tablet diclofenac 50 mg tds for 3 days. He was reviewed after 1 week [Table/Fig-4], 15 days [Table/Fig-5], 1 month [Table/Fig-6] and 3 months [Table/Fig-7] after the procedure, and no complications or recurrence were noted and healing was good.
One week postoperative view showing good healing.
A 15 days postoperative view.

One month postoperative view.
Three months postoperative view showing no signs of recurrence.

Discussion
The World Health Organisation (WHO, 1978) defined leukoplakia as “a white patch or plaque that cannot be identified, clinically, or microscopically as any other disease” [1]. There are a number of white lesions that should be excluded before the clinical diagnosis of oral leukoplakia is made [2].
The various aetiologies of Leukoplakia include tobacco in smoked and smokeless forms, alcohol consumption, infection due to virus (HPV strains 16, 18) and fungus (Candida albicans), levels of Vitamin A, B12, C, beta-carotene, folic acid and syphilis are associated [3].
Clinically Oral Leukoplakia is of 2 types:
Homogenous leukoplakia: They appear as uniform, white, flat lesions. It is the most common form and most prevalent in the buccal mucosa. They have a low premalignant potential.
Non-homogenous leukoplakia: They have a mixed white and red colour. They may be speckled, nodular, verrucous or proliferative type. They have a higher malignant potential than homogenous variant [4].
The most common site for occurrence of oral leukoplakia is buccal mucosa while the most common site for malignant transformation is tongue. The rate of malignant transformation ranges from 0.13% to 34.0%. The mean rate of malignant transformation among all studies is 14.9% [5]. Oral Leukoplakia can transform into malignant form [6]. Malignant transformation of the lesion can be avoided by early detection and management.
Leukoplakia can be managed using different modalities including Cessation of predisposing habits. Topical management can be done using anti-inflammatory agents, carotenoids, retinoids, antimycotic agents and cytotoxic agents, etc. Chemo preventive agents such as vitamins (A, C, E), fenretinide (Vitamin A analogue), carotenoids (beta carotene, lycopene), green tea, curcumin are also beneficial, Surgical excision of the lesion, electro cautery, cryotherapy, LASER surgery, Photodynamic Therapy (PDT) or combined treatment can be employed [4,7,8].
Conventional surgery may lead to certain side effects like scar formation, contraction of wound, and contamination of the surgical field [8]. Excision of precancerous lesions using LASER has comparative advantages over surgical excision. These advantages include a bloodless field because of the haemostatic effect, procedure is less painful, precision in removal, favourable healing, less scarring, less postoperative pain, swelling, oedema and infection resulting in good patient compliance, fewer complications and low morbidity [9]. As this procedure can be repeated, it is favoured for oral leuoplakia treatment as it is a recurring condition. Because of these advantages, LASER removal by vaporisation or excision appears useful in treatment of oral leukoplakia.
A number of studies have been done on the excision of oral leuoplakia using LASER and have shown promising results [8-14] [Table/Fig-8]. In the present case, patient reported minimal intraoperative and postoperative pain and discomfort. These results are similar to the findings of Mohan R et al., in year 2017 who reported minimal postoperative pain and discomfort [13].
Previous studies done on treatment of leukoplakia using LASER.
| Author | Study |
|---|
| Praveen KNS et al., [10] | Ten cases leukoplakia were treated using 810-nm diode LASER followed up for 3 months and assessed for pain and healing postoperatively. In almost all cases healing was complete within 3-4 weeks duration. There was mild pain in the majority of cases following laser therapy. |
| Kharadi UAR et al., [11] | Ten cases having homogenous leukoplakia were excised using a 940 nm diode laser. Out of 10 patients, 8 showed complete disappearance of lesion even after 6 months follow-up. They concluded that laser can be safely and effectively used as a treatment modality for homogenous leukoplakia, without any complication and without compromising health and function of patients. |
| Ramwala Vet al., [12] | Ten systemically healthy patients having oral leukoplakia were treated with diode laser and bleeding, pain, healing and recurrence were observed. Results showed that overall healing was good to very good on 7th day and Excellent on 30th day in all the cases. Pain disappeared in all the cases on 7th postop day with less bleeding. No recurrence was reported on 1 year follow-up. |
| Giri D et al., [9] | Reported a case of verrucous leukoplakia using diode Laser. They obtained excellent results with no signs of recurrence. |
| Mohan R et al., [13] | Minimal intraoperative and postoperative pain after diode LASER therapy. They also reported minimal intraoperative bleeding during the procedure and wound healing was also good. |
| Gupta P et al., [8] | Reported a case of leukoplakia excision using 970 nm Diode Laser. They reported uneventful healing and minimal patient discomfort. |
| Natekar M et al., [14] | Performed a comparative assessment of cryosurgery, diode laser and CO2 laser surgery in the treatment of Leukoplakia. According to their study, CO2 and diode laser exhibited significantly better clinical parameters in terms of reduced pain intensity, infection, and scar formation when compared with cryosurgery. |
The wound healing was also satisfactory similar to the studies of Praveen KNS et al., and Mohan R et al., [10,13]. In the present case the patient did not show any signs of recurrence on follow-up. This was similar to findings of study conducted in Natekar M et al., [14], the patients in their study showed no sign of recurrence on 6 months follow-up, Ramwala V et al., also reported no recurrence on 1 year follow-up [12].
There are few disadvantages of using LASER which includes prolonged healing time required after LASER due to the sealing of blood vessels and lymphatic in the surgical field, LASER can also lead to ocular damage of the operator if not used with appropriate eye wear, it is important to follow specific preventive measures while performing the LASER therapy. LASER can lead to lateral tissue damage if not used with caution, LASER system is expensive and requires training and therefore overall cost of the procedure is more as compared to treatment with scalpel. Some of the other disadvantages include respiratory or environmental hazards, combustion hazards and electrical problems [10,15].
Conclusion
The main purpose of treating oral leukoplakia is to prevent transformation into malignant form as the patients are mostly asymptomatic. Avoiding tobacco and alcohol abuse is the first step to prevent disease progression. The cases which do not respond to conventional medical management should be advised complete excision. Excision of precancerous oral lesions using LASER offers comparative advantages over traditional scalpel excision.
[1]. WHO Collaborating Center for Oral Precancerous LesionsDefinition of leukoplakia and related lesions. An aid to studies on oral precancerOral Surg Oral Med Oral Pathol 1978 4:518-39.10.1016/0030-4220(78)90383-3 [Google Scholar] [CrossRef]
[2]. Carrard VC, van der Waal I, A clinical diagnosis of oral leukoplakia; A guide for dentistsMed Oral Patol Oral Cir Bucal 2018 23(1):e59-64. [Google Scholar]
[3]. Goyal D, Goyal P, Singh HP, Verma C, An Update on precancerous lesions of oral cavityInt J Med and Dent Sci 2013 2(1):70-75.10.19056/ijmdsjssmes/2013/v2i1/86738 [Google Scholar] [CrossRef]
[4]. Deliverska EG, Petkova M, Management of oral leukoplakia-analysis of the literatureJ of IMAB 2017 23(1):1495-504.10.5272/jimab.2017231.1495 [Google Scholar] [CrossRef]
[5]. Warnakulasuriya S, Ariyawardana A, Malignant transformation of oral leukoplakia: a systematic review of observational studiesJ Oral Pathol Med 2016 45:155-66.10.1111/jop.1233926189354 [Google Scholar] [CrossRef] [PubMed]
[6]. Hernandez BY, Zhu X, Goodman MT, Gatewood R, Mendiola P, Quinata K, Betel nut chewing, oral premalignant lesions, and the oral microbiomePLoS ONE 2017 12(2):017219610.1371/journal.pone.0172196 [Google Scholar] [CrossRef]
[7]. Lodi G, Franchini R, Warnakulasuriya S, Varoni EM, Sardella A, Kerr AR, Interventions for treating oral leukoplakia to prevent oral cancerCochrane Database Syst Rev 2016 7:CD00182910.1002/14651858.CD001829.pub4PMC6457856 [Google Scholar] [CrossRef] [PubMed]
[8]. Gupta P, Thakur J, David CM, Excision of Oral Leukoplakia using 970 nm Diode LASERInt J Adv Integ Med Sci 2017 2940:208-11.10.5005/jp-journals-10050-10109 [Google Scholar] [CrossRef]
[9]. Giri D, Agarwal N, Sinha A, Srivastava S, Mishra A, Diode laser: In treatment of recurrent verrucous leukoplakiaContemp Clin Dent 2016 7:250-54.10.4103/0976-237X.18304327307679 [Google Scholar] [CrossRef] [PubMed]
[10]. Praveen KNS, Veeraraghavan G, Reddy S, Kotha P, Koneru J, Yelisetty K, Management of oral leukoplakia using diode laser: A pilot studyBJMMR 2015 10(7):01-06.10.9734/BJMMR/2015/19178 [Google Scholar] [CrossRef]
[11]. Kharadi UAR, Onkar S, Birangane R, Chaudhari S, Kulkarni A, Chaudhari R, Treatment of oral leukoplakia with a diode laser: a pilot study on Indian subjectsAsian Pac J Cancer Prev 2015 16(18):8383-86.10.7314/APJCP.2015.16.18.838326745089 [Google Scholar] [CrossRef] [PubMed]
[12]. Ramwala V, Use of diode laser in the management of oral leukoplakia-A Study of 10 CasesIOSR Journal of Dental and Medical Sciences 2016 15(7):81-85.10.9790/0853-150768185 [Google Scholar] [CrossRef]
[13]. Mohan R, Sunil MK, Raina A, Krishna K, Basu M, Khan T, Diode laser therapy of homogenous leukoplakia- a clinical studyTMU J Dent 2017 4(3):90-92. [Google Scholar]
[14]. Natekar M, Raghuveer HP, Rayapati DK, Shobha ES, Prashanth NT, Rangan V, Panicker AG, A comparative evaluation: Oral leukoplakia surgical management using diode laser, CO2 laser, and cryosurgeryJ Clin Exp Dent 2017 9(6):e779-84.10.4317/jced.5360228638555 [Google Scholar] [CrossRef] [PubMed]
[15]. Sandhya J, Lasers in dentistry-short reviewPharm. Sci. & Res 2016 8(7):638-41. [Google Scholar]