Right Psoas Abscess as a Consequence of Ruptured Appendix with Caecal Perforation and Presenting as Right Lumbar Swelling in a Toddler: A Rare Presentation of Appendicitis
Rafey Abdul Rahman1, Umesh Kumar Gupta2
1 Assistant Professor, Department of Paediatric Surgery, Uttar Pradesh University of Medical Sciences, Saifai, Etawah, Uttar Pradesh, India.
2 Assistant Professor, Department of Paediatric Surgery, Uttar Pradesh University of Medical Sciences, Saifai, Etawah, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Umesh Kumar Gupta, Type 4, Block-C, Room No-202, New Campus, Etawah, Uttar Pradesh, India.
E-mail: dukg9999@gmail.com
Psoas Abscess (PA) is a very rare form of presentation of appendicular pathology, especially in a toddler. A three-year-old male child presented to the casualty with complaint of right lumbar swelling for 14 days. There was no other significant history. On clinical examination, there was 5×5 cm right lumbar swelling with a prominent bulge, which was non tender. USG and Contrast Enhanced Commuted Tomography (CECT) abdomen revealed PA which was drained by incision made on the bulge. There was feculent output noted from the incision and drainage site the following day. Child underwent exploratory laparotomy and was found to have ruptured partially sloughed of appendix along with perforated caecum going deep to the psoas muscle which in turn was communicating via tract to the incision and drainage site. Residual appendectomy along with caecal repair was done. Diverting proximal loop ileostomy was made and an abdominal drain was placed. Postoperatively, the child recovered well and was discharged on postoperative day 5 with a functioning ileostomy and on full oral feeds. In the follow-up distal cologram was done which revealed free flow of contrast along the entire colon up to rectum. The child has now been planned for stoma closure. Prompt diagnosis and prompt intervention was responsible for significantly reducing morbidity in the present case.
Complicated retro-caecal appendicitis, Faecal fistula, Pyogenic abscess
Case Report
A three-year-old male child presented to casualty with complaint of obvious swelling in right lumbar region for last two weeks. There was no history of abdominal pain, trauma, urinary tract infection, fever or vomiting. However, child was passing little amount of stool for last two days.
Abdomen was soft, non-tender and no organomegaly was noted. There was 5×5 cm right lumbar swelling with a prominent bulge, which was non tender. There was no difficulty in walking or standing. Spine was grossly normal. Ultrasound was done and it was suggestive of a right PA.
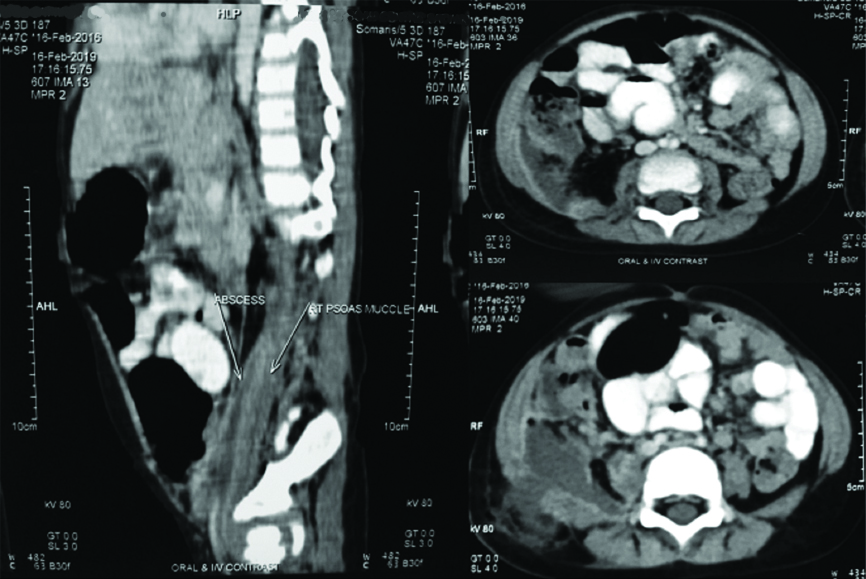
Child was admitted and IV antibiotics were started. To rule out secondary causes of PA, a CECT of the abdomen was done [Table/Fig-1]. CECT revealed large non enhancing collection measuring 5.3×4×10 cm in the lower aspect of right psoas muscle and whole of the iliacus muscle. Laterally, it extended into abdominal wall parieties above the right iliac bone. Inferiorly, it extended up to the right hip joint. No associated caecal or appendicular pathology was noted. Few necrotic iliac nodes were noted on the right side suggestive of tubercular aetiology. The report of CECT was available after two days of admission and by this time there was an obvious bulge which was ready for drainage.
CECT abdomen showing right psoas abscess.
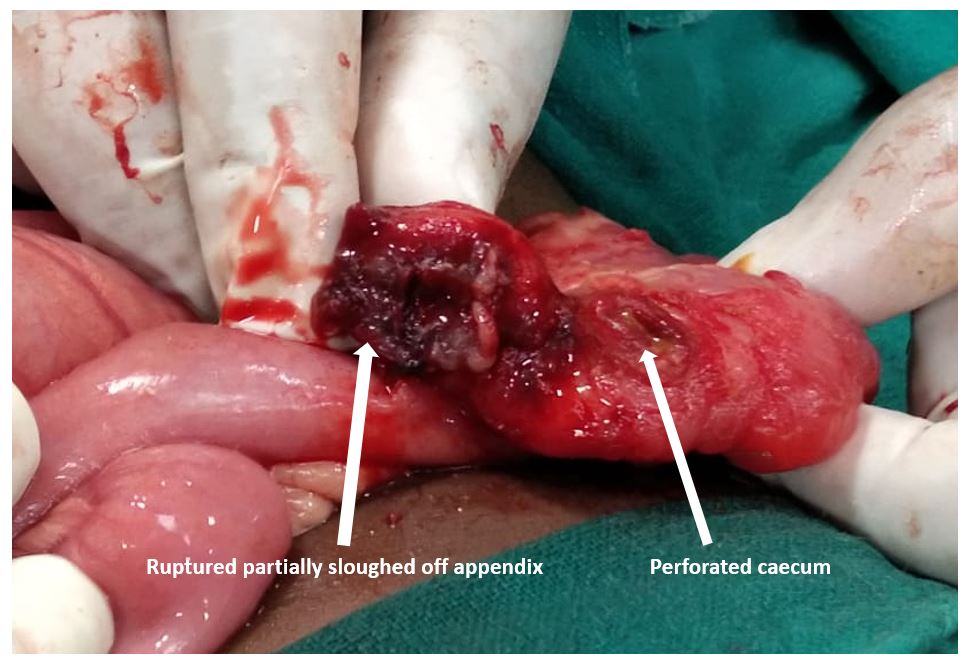
Consent was taken from the patient before the surgery. A small incision was made over the swelling, 40 mL of pus was drained and the incision was packed with the gauze piece. Next day, the packed gauze piece was removed and some amount of pus with faecal matter was noted to be coming out from the incision and drainage site. It was highly unlikely for the bowel to be injured during incision and drainage procedure as the incision made was very superficial. Clinically, child was well preserved with no signs of peritonitis and abdomen was soft. Exploratory laparotomy was performed the same day. The abdomen was not contaminated with stool. Ruptured, partially sloughed off appendix along with perforated caecum was found going deep into the right psoas muscle which in turn was communicating via tract to the incision and drainage site [Table/Fig-2]. Perforation site at the caecum was close to the base of the appendix. Residual appendectomy was performed. Caecal perforation was repaired and diverting proximal loop ileostomy was made. The cavity and the tract were thoroughly washed and drain was placed through the incision and drainage site.
Clinical photograph showing ruptured appendix with a caecal perforation.
Postoperatively, the child recovered well. Ileostomy started functioning on Postoperative day 2. Drain was removed on Postoperative day 3. Child was discharged on Postoperative day 5 with a functioning ileostomy. Histopathology of the residual appendectomy revealed features consistent with the diagnosis of appendicitis [Table/Fig-3]. Child is presently on follow-up and has undergone distal cologram, which revealed free flow of contrast along the entire colon upto rectum without any evidence of leak. Child has now been planned for ileostomy closure.
Histopathology appendix (100x) showing mix infiltration in mucosa.

Discussion
The PA is a rare infectious pathology occurring as a result of accumulation of pyogenic collection in the iliopsoas muscle compartment. It is called as “Psoitis” and was first described by Mynter in 1881 [1]. It is a rare condition and usually occurs secondary to local infection and inflammatory process. It is also a well-recognised complication of tuberculosis of spine. Acute appendicitis, Crohn’s disease, colorectal carcinomas and diverticulitis have been held responsible for secondary PA [2,3]. Incidence of PA is 12 cases/100,000/year in the world with increasing incidences in industrialised countries [4,5].
Acute appendicitis is one of the most common causes of abdominal pain. Secondary PA is much more common in adults than in children [6]. However, appendicitis presenting as PA or retro-peritoneal abscess, especially in toddler is a rare entity. Secondary PA as a consequence of acute appendicitis has a high mortality rate (19%) [7].
Psoas is a retroperitoneal muscle having its origin from lateral border of 12th thoracic to 5th lumbar vertebrae and its insertion onto the trochanter of femur. The muscle has close proximity to caecum, appendix, ureters, aorta, jejunum, spine and iliac nodes. Infections of these structures sometime present as iliopsoas abscess.
In the present case the appendix had ruptured, cecum had perforated and both structures buried themselves deep into the psoas creating an abscess mixed with feculent matter along the iliopsoas muscle. In-spite of the extension of abscess up to the hip joint, child did not present with hip pain or difficulty in walking. Also, parents never gave the history of pain in abdomen in recent times. Only complaint was swelling in the right lumbar region.
The sensitivity and specificity of CECT in diagnosing appendicular pathology preoperatively is 96.4% and 95.4%, respectively [8]. In this case CECT done did not reveal a clear appendicular or caecal pathology. Possible explanation for this can be because, in presence of large amount of necrotic tissue debris inflamed and partially sloughed off appendix could not be identified. Another reason can be the low index of suspicion by the radiologist as appendicitis is a very rare cause of PA. Possible cause of caecal perforation could be trauma unwitnessed by the parents and it may be due to tip of inflamed appendix eroding the caecal wall. As the child was initially taken to another private hospital two days before presenting to the casualty, iatrogenic causes like needle aspiration was also considered as the possible cause. But the parents did not give history of any such intervention. Exploratory laparotomy clearly demonstrated the cause of PA and the pathology was dealt in a standard fashion. Caecostomy was also an option rather than proximal diverting loop ileostomy. We chose the latter because the perforated caecal site was very close to the appendicular stump.
The case is unique because of various reasons. Firstly, such a presentation of appendicular pathology in toddler is rare. Furthermore, ruptured appendix along with perforated cecum burying (going deep inside) itself into the psoas has not been described previously. Also, because of the caecal perforation the pus was mixed with faecal content in this case which was spread along the plane of the ilio-psoas muscle. The child remained well preserved without any sign of peritonitis, fever and abdominal pain which is not the usual mode of presentation of appendicular pathology. There is high probability that pain of acute appendicitis that may have occurred two weeks prior to presentation in the casualty may have been ignored by the parents. Staphylococcus is usually the pathogen involved in primary PA and E.coli in secondary PA [9,10]. In this case the pathogen was E.coli pointing towards the diagnosis of secondary PA.
A similar case report has been published recently in which PA secondary to acute appendicitis was described in a 16-year-old male child [11]. The child in the published case report had classical features of appendicitis as well as PA. However, there was no caecal perforation. In the present case associated caecal perforation with no clinical features of PA (limp, walking difficulty) and no clinical signs of appendicitis (abdominal pain, leucocytosis, peritonitis) at the time of presentation was unique making the diagnosis difficult. CECT of the abdomen also failed to reveal the appendicular and caecal pathology in the present case.
Conclusion
Prompt diagnosis and prompt intervention were responsible for significantly reducing morbidity in this case. We are of the view that in case of PA especially on the right side, appendicular pathology should always be kept in mind and a thorough preoperative work up should be done to establish the diagnosis at the earliest followed up by a prompt intervention to significantly reduce mortality and morbidity in this condition.
[1]. Garner J, Meiring P, Ravi K, Gupta R, Psoas abscess? not as rare as we think?Colorectal Disease 2007 9(3):269-74.10.1111/j.1463-1318.2006.01135.x17298628 [Google Scholar] [CrossRef] [PubMed]
[2]. Petrovic I, Pecin I, Prutki M, Augustin G, Nedic A, Gojevic A, Thigh abscess as an extension of psoas abscess: The first manifestation of perforated appendiceal adenocarcinoma: Case reportWiener klinische Wochenschrift 2014 127(15-16):645-48.10.1007/s00508-014-0651-025412593 [Google Scholar] [CrossRef] [PubMed]
[3]. Choi S, Han H, Kim W, Song T, Choi S, A case of a recurrent iliopsoas abscess masking a complicated appendicitis successfully treated by a laparoscopic approachSurgical Laparoscopy, Endoscopy & Percutaneous Techniques 2010 20(2):e69-e72.10.1097/SLE.0b013e3181d6969520393325 [Google Scholar] [CrossRef] [PubMed]
[4]. Gruenwald I, Abrahamson J, Cohen O, Psoas Abscess: Case report and review of the literatureJournal of Urology 1992 147(6):1624-26.10.1016/S0022-5347(17)37650-4 [Google Scholar] [CrossRef]
[5]. Franco-Paredes C, Blumberg H, Psoas Muscle abscess caused by Mycobacterium tuberculosis and Staphylococcus aureus: Case report and reviewThe American Journal of the Medical Sciences 2001 321(6):415-17.10.1097/00000441-200106000-0000811417755 [Google Scholar] [CrossRef] [PubMed]
[6]. Ricci M, Rose F, Meyer K, Pyogenic psoas abscess: Worldwide variations in etiologyWorld Journal of Surgery 1986 10(5):834-42.10.1007/BF016552543776220 [Google Scholar] [CrossRef] [PubMed]
[7]. Mallick I, Iliopsoas abscessesPostgraduate Medical Journal 2004 80(946):459-62.10.1136/pgmj.2003.01766515299155 [Google Scholar] [CrossRef] [PubMed]
[8]. Park JS, Jeong JH, Lee JI, Lee JH, Park JK, Moon HJ, Accuracies of diagnostic methods for acute appendicitisAm Surg 2013 79:101-06. [Google Scholar]
[9]. Taiwo B, Psoas abscess: A primer for the internist: Case ReportSouth Med J 2001 94(1):02-05.10.1097/00007611-200194010-0000111213936 [Google Scholar] [CrossRef] [PubMed]
[10]. Santaella R, Primary vs secondary iliopsoas abscessArchives of Surgery 1995 130(12):130910.1001/archsurg.1995.014301200630097492279 [Google Scholar] [CrossRef] [PubMed]
[11]. Sahu SK, Singh PK, Singh BP, Sachan PK, Acute appendicitis leading to pyogenic psoas abscess; Case reportCer San D (J Surg Arts) 2013 6(1):28-31. [Google Scholar]