Excessive gingival display is a widespread condition that adversely affects the aesthetic of the smile [1]. For the periodontist, Altered passive eruption (APE) is considered as the most important indication for the treatment of gingival smile [2]. APE is diagnosed when there is an excessive gingival display with short clinical crowns and healthy periodontal tissues. There should also be an ideal length and normal muscular efficiency of the upper lip, no vertical skeletal defects, and no dentoalveolar deformities [3].
Based on the amount of gingival tissue, this condition is classified as type 1 when there is an excess amount of gingival tissue between the free gingival margin and the mucogingival junction and as type 2 when there is a standard amount of keratinized gingiva. It was then classified into two subtypes depending on the relation between the alveolar Bone crest (ABC) and the Cemento-enamel junction (CEJ). Subtype A is when the distance between BC and CEJ is approximately 1.5 mm. Subtype B is when the BC is at or coronal to the CEJ, and in this case, there is no sufficient distance for the normal Biological width (BW) [4].
Aesthetic crown lengthening (ECL) is still one of the most common surgical treatments of APE [5]. It has become necessary to compare its different surgical techniques and to evaluate the related complications to demonstrate the most effective technique that gives the required outcomes with maximum patient satisfaction [6].
Gingival tissue coronal rebound is one of the most noted post-operative complications of traditionally used techniques. The surgical techniques that include flap reflection cause more coronal displacement of the gingival margin [7]. The osseous resection during traditional ECL is performed using various hand or rotary instruments, which may cause numerous injuries like thermal or physical damage to bone and severe trauma to the periodontal tissues, blood vessels, or even nerves, especially when there is limited or difficult access to the surgical area [8]. This traditional surgery requires a long duration to perform all procedures including flap reflection and surgical suturing, which causes more pain and bleeding [9].
It has been suggested that minimally invasive techniques should be performed in ECL as specialists aim to reduce pain, discomfort, surgery duration, and to accelerate healing [10]. The flapless technique is considered to be a promising alternative approach and is a suture-less, atraumatic, and invasive technique that has been shown to increase patient satisfaction and comfort [11]. Piezosurgery was also proposed as a minimally invasive surgical procedure [12].
Piezoelectric bone surgery provides high precision in bone resection, high tactile sensibility, and a selective cut of mineralized tissue while sparing soft tissue. This technology uses a cavitation effect where bubbles are created from the liquid of the physiological serum, which leads to internal explosions and generates shock waves that cause microscopic coagulation [13].
The literature does not offer a lot of information about the differences between Flapless (FL) and Open-flap (OF) approaches in ECL. Therefore, this is the first study which aimed to compare the clinical results of a (FL) approach and (OF) approach in ECL for the treatment of gingival smile up to 3 months after piezoelectric bone surgery.
Materials and Methods
This study was a prospective, split-mouth, controlled clinical study comparing both open flap and flapless techniques for aesthetic crown lengthening. The ethical approval for this study was obtained from The Graduate Studies and Scientific Research Council of Damascus University (approval number/2063). The study sample was calculated using G.power program. A sample size of total 16 patients was determined, with a confidence level of 85% and an alpha value of 0.05. Patients were selected from those referred to the Department of Periodontology, Faculty of Dentistry, Damascus University. Patients were interviewed for possible participation in this study based on the diagnosis of APE 1B and a treatment plan that included the need for ECL. The diagnosis was confirmed through clinical and radiographic examination. A sufficient explanation was given to the patients regarding the study, and they were asked to provide their written consent for their participation in the study. The study was started in May 2018 and was completed in November 2018. Data entry of all information and statistical analysis were performed in December 2018.
The study inclusion criteria were patients with a gummy smile due to APE (Type 1B) in at least three maxillary teeth (central incisors, lateral incisors, canines, or premolars) per half contralateral quadrant; thin to moderate thickness bone pattern; ≥20 years; and no clinical attachment loss. Exclusion criteria were as follows: pregnant or lactating mothers, smokers, use of an orthodontic appliance, any previous periodontal surgery in the same area, prostheses on treated teeth, taking antibiotics or anti-inflammatory therapies during the last two months, or systemic health cases affecting the healing of tissues (diabetes).
At a pre-surgical appointment, 2-mm clear co-polyester plastic probing stents were made in order to standardise the location during measurements. The measurement stent was grooved vertically at the mesiofacial, facial, and distofacial surfaces of each study tooth as reference points. The performance of oral hygiene procedures was confirmed for all patients.
The right quadrant was distributed at random to receive OF or FL techniques by a computer-generated table. Afterward, the contra-lateral left quadrant was allocated to the other group. Both therapies were performed during one appointment by the same operator under local anaesthesia.
Open Flap Technique (Control Group)
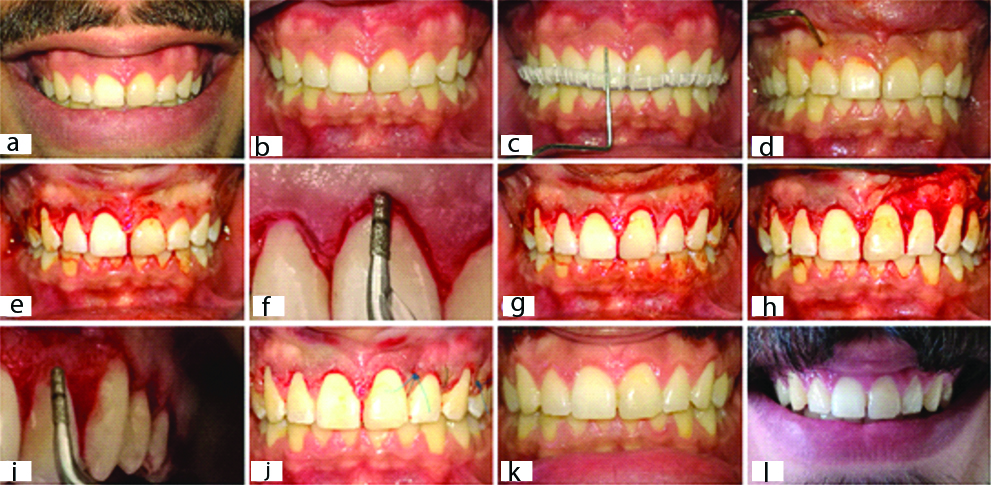
The gingivectomy was surgically performed with a scalpel blade 15C. This was followed by an intra-sulcular incision, removal of the strip of outlined marginal gingiva [Table/Fig-1] and elevation of a mucoperiosteal flap. Then, the CE3 surgical tip [Table/Fig-2], which is manufactured by Satelec® and designed to operate with Piezotome®, was used for ostectomy and osteoplasty until a 3-mm distance was achieved between the bone crest and the gingival margin. The Gracey-curette #5-6 (Medesy srl, Maniago PN, Italy) was used to carry out the root planing of the exposed root surfaces. The flap was sutured at the base of the papilla with interrupted 5-0 non-resorbable nylon sutures [14].
(a) pre-surgical excessive gingival display; (b) pre-surgical short clinical crowns due to APE; (c) recording clinical measurements using UNC-15 probe and the stent; (d) marking the bleeding points with the periodontal probe; (e) gingivectomy on the FL side; (f) osteotomy using CE3 tip on the FL side without flap reflection; (g) gingivectomy on the OF side; (h) flap reflection on the OF side; (i) osteotomy using CE3 tip on the OF side; (j) surgical suturing on the OF side only; (k) the increase in clinical crown length 3 months post surgery; (l) patient’s smile 3 months after the surgery.
CE3 Diamond-coated cylindrical tip designed for delicate osteotomies with laser mark placed at 3 mm.

Flapless Technique (Test Group)
On the other side, the gingivectomy and the intra-sulcular incisions and gingival tissue removal were performed as described above for the control group. The osteotomy and osteoplasty were done using the same CE3 tip via incisions without flap elevation. The root surfaces were also carefully planned via incisions. The required distance of 3 mm between the BC and the gingival margin was checked by inserting a periodontal probe into the incision. Sutures were not performed [Table/Fig-1].
At the end of the procedures, all patients were prescribed a non-steroidal anti-inflammatory analgesic and twice daily 0.12% chlorhexidine digluconate rinses for two weeks. Sutures were removed seven days postoperatively, and a plaque control regimen was instituted.
Clinical Evaluation
Measurements were obtained preoperatively, immediately after surgery, and seven days and three months postoperatively. Using the probing stent, the following baseline measurements were taken for each site at baseline and three months postsurgery: Plaque index (PI); Bleeding on probing (BOP); Probing depth (PD), that is, the distance between the Gingival margin (GM) and the bottom of the gingival sulcus; relative CAL (rCAL), that is, the distance from a fixed landmark in the stent to the bottom of the gingival sulcus [15].
The relative Bone level (rBL), which is the distance between a fixed landmark in the stent and the BC, was recorded before and immediately after the surgery [11]. It was clinically measured using UNC-15 manual probe (Medesy srl, Maniago PN, Italy).
Relative Gingival Margin (rGM) is the distance from a fixed landmark in the stent to the most cervical point of the GM. Keratinized gingiva height (KGH) is the distance from the margin of free gingiva to the mucogingival line. rGM and KGH were assessed at baseline, seven days, and three months after the surgery [11].
Procedure Duration
The duration of each surgical method was calculated separately, beginning immediately after the injection of local anaesthesia in the OF group or the FL technique group.
A week after surgery, the patients were asked to identify, based on a 100-mm horizontal line (visual analog scale; VAS), their satisfaction with the overall treatment including discomfort, swelling, redness and aesthetics. After 3 months of therapy, patients were asked to identify their satisfaction about improvements in the aesthetic appearance on each side separately using another VAS questionnaire. VAS for satisfaction is a horizontal line of 100-mm long, with 0 at the beginning equals to “no satisfaction” and 100 at the end equals to “extreme satisfaction”.
Another VAS questionnaire was given to the patients to demonstrate their perception of pain 24 hours and 48 hours after the procedures on each side separately. The VAS scores were recorded on a 100-mm horizontal line, with 0 equals to “no pain” and 100 equals to “very severe pain”.
All questionnaires were administered by the same professional, and all clinical measurements were taken using a UNC-15 manual probe by the same operator.
Cone beam Computed Tomography (CBCT)
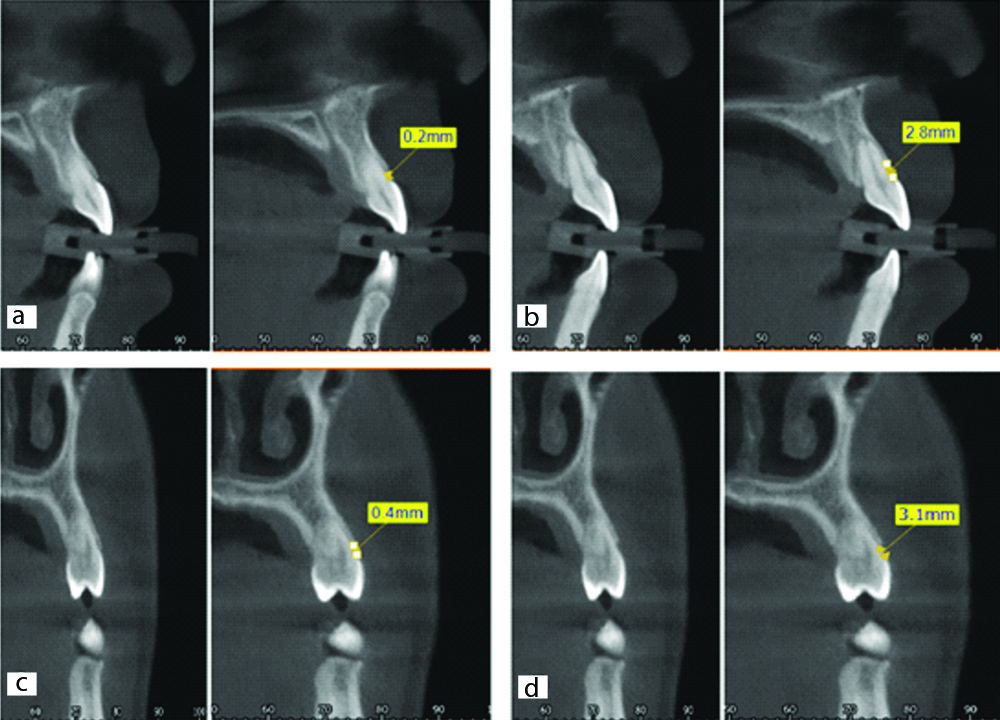
At baseline and 3 months post-surgery, the CBCT scans were taken, and the images (sections 1.0 mm apart) were acquired using suitable software. The following biological width, that is, the CEJ-to-BC distance (CEJ-BC) and the Supracrestal gingival height (SGH), meaning the GM-to-BC distance (GM-BC), were obtained in the buccal aspect of the middle image section of each tooth [Table/Fig-3].
(a) pre-surgical CBCT shows a distance of 0.2 mm between CEJ and BC which confirms the diagnosis of APE type 1B; (b) the second CBCT shows the increase in CEJ-BC distance 3 months post surgery caused by the osteotomy procedure during flapless ECL surgery; (c) CEJ- BC distance was 0.4 mm pre-surgery; (d) 3 months after open flap osteotomy using Piezosurgery, CEJ-BC increased to 3.1 mm.
Statistical Analysis
Differences in clinical indices (PI, GI, BOP, PD, rCAL, rBL, rGM and KGH), radiographic parameters (CEJ-BC and SGH), procedure duration, VAS scale for pain and VAS scale for patient satisfaction within a group at each time point were examined using paired t-test, and differences in the same parameters between OF and FL groups were examined using independent t-test. The level of significance was set at 0.05. The software used was SPSS 19.0 (SPSS, Inc., Chicago, USA)
Results
Sixteen patients (11 females, 5 males), aged 24.4±3.5 years (range: 21-35 years) were recruited at the beginning of the study. A total of 32 sites were treated by OF or FL ECL. No subjects were lost during a 3-month follow-up, and all of them were included in the statistical analyses. No post-surgical complications were observed. Regarding patients’ characteristics at baseline, the prevalence of females was observed to be higher among the research sample (68.75%).
A statistically higher mean surgical time was observed in the OF group (25.38±5.44 minutes) than in the FL group (15.94±4.25 minutes) (p<0.05).
The immediate post-surgical mean of rBL was increased significantly compared with baseline for both treatments (p<0.05), without differences between groups (p>0.05) [Table/Fig-4]. The mean of the GI measurements was higher in the OF group than in the FL group at 3 months (p<0.05). In addition, the mean measurement of GI decreased at 3 months for the FL group compared with baseline (p<0.05). Furthermore, the mean of the BOP measurements was higher in the OF group than in the FL group at 3 months (p<0.05). There were no differences between OF and FL for PI at any follow-up visit (p>0.05).
Mean (±SD) Levels of the clinical parameters.
| Parameters | Group | OF | FL |
|---|
| PI | Baseline | 0.08±0.09 | 0.08±0.10 |
| 3 months | 0.05±0.09 | 0.03±0.05 |
| BOP | baseline | 0.09±0.08 | 0.08±0.07 |
| 3 months | 0.17±0.14 | 0.05±0.04* |
| GI | baseline | 0.054±0.09 | 0.036±0.05 |
| 3 months | 0.061±0.08 | 0.004±0.02*† |
| PD | baseline | 2.58±0.38 | 2.58±0.41 |
| 3 months | 1.20±0.12† | 1.17±0.13† |
| rCAL | baseline | 5.43±0.75 | 5.41±0.76 |
| 3 months | 6.18±0.69† | 6.24±0.69† |
| rBL | baseline | 7.35±0.74 | 7.35±0.71 |
| Immediately after | 9.28±0.73** | 9.26±0.77** |
| rGM | baseline | 2.89±0.48 | 2.83±0.48 |
| 7 days | 4.87±0.63† | 4.80±0.67† |
| 3 months | 4.64±0.61†‡ | 4.64±0.67†‡ |
| KGH | baseline | 5.91±0.76 | 5.98±0.85 |
| 7 days | 3.94±0.78† | 3.95±0.93† |
| 3 months | 4.13±0.80†‡ | 4.07±1.01†‡ |
PI: Plaque index; BOP: Bleeding on probing; GI: Gingival index; PD: Probing depth; rCAL: relative Clinical attachment level; rBL: relative Bone level; rGM: relative Gingival margin; KGH: Keratinized gingival high
*Significant differences between OF and FL groups at 3 months post surgery by independent samples t-test (p<0.05)
†Significant differences between baseline and 3 months within a group by paired samples t-test (p<0.05)
‡Significant differences between 7 days and 3 months within a group by paired samples t-test (p<0.05)
**Significant differences between baseline and immediately after surgery within a group by paired samples t-test (p<0.05)
There was a statically significant decrease in PD and rCAL from baseline to 3 months for both treatments (p<0.05), without differences between groups at any point time (p>0.05) [Table/Fig-4].
At each time point, there was a significant increase in rGM compared to baseline for both treatments (p<0.05), but the mean of the measurements at 3 months were significantly less than the 7-day-post-surgical values in the OF and FL groups (p<0.05). There were no differences between OF and FL for rGM at any time point (p>0.05) [Table/Fig-4].
The KGH means were reduced significantly at all time points compared with baseline for both treatments (p<0.05), but the means of the measurements at 3 months were significantly more than the 7-day-post-surgical values in the OF and FL groups (p<0.05). There were no differences between groups at any time point (p>0.05).
The decrease in the SGH mean after 3 months was noted to be significant for each group compared to the pre-surgical baseline (p<0.05), without differences between groups at any time point (p>0.05). The CEJ-BC means were significantly increased compared with baseline for both treatments (p<0.05). There were no differences between groups at any time point (p>0.05) [Table/Fig-5].
Mean (±SD) Levels of the radiographic parameters.
| Parameters | Time point | OF | FL |
|---|
| CEJ-BC | Baseline | 0.298±0.11 | 0.288±0.11 |
| 3 months | 2.097±0.15† | 2.094±0.13† |
| SGH | Baseline | 4.00±0.49 | 4.02±0.49 |
| 3 months | 3.06±0.30† | 3.08±0.35† |
CEJ-BC, Cemento-enamel junction to bone crest (biological width); SGH: Supracrestal gingival height
†Significant differences between baseline and 3 months within a group by paired samples t-test (p<0.05)
Based on a VAS, it was observed that the extent of pain experienced after surgery was statistically higher in the OF group compared with the FL group (p<0.05) at any time point. The results showed a significant decrease in mean pain values after 48 hours compared to 24 hours in both groups (p<0.05) [Table/Fig-6].
Means (±SD) of evaluated VAS parameters related to pain for all cases.
| Parameter | Time point | OF | FL |
|---|
| Pain | 24 hours | 31.31±10.18 | 9.00±6.73* |
| 48 hours | 13.19±11.14† | 2.31±2.96**† |
*Significant differences between OF and FL groups at 24 hours post surgery by independent samples t-test (p<0.05)
**Significant differences between OF and FL groups at 48 hours post surgery by independent samples t-test (p<0.05)
†Significant differences between 24 hours and 48 hours within a group by paired samples t-test (p<0.05)
Regarding the results of the VAS, a statistically higher mean patient satisfaction was observed in the FL group compared to OF at the first post-operative week (p<0.05).
After 3 months of therapy, an improvement in both groups was detected. The increase in patient satisfaction was statistically significant in the OF group compared with the 7 days (p<0.05), and there was no difference between the two groups at 3 months (p<0.05) [Table/Fig-7].
Means (±SD) of evaluated VAS parameters related to patient satisfaction.
| FL | OF | Time point | Parameter |
|---|
| 82.63±9.97* | 66.50±11.70 | 7 days | Patient satisfaction |
| 82.81±8.02 | 80.06±8.23† | 3 months |
*Significant differences between OF and FL groups at 7 days post surgery by independent samples t-test (p<0.05)
†Significant differences between 7 days and 3 months within a group by paired samples t-test (p<0.05)
Discussion
Inappropriate smile can be a complicated condition and even a real psychological problem for some people, especially those who suffer from an unaesthetic gingival smile [16]. Although the increasing demand for improving aesthetics is becoming an important part of the current practice of periodontal surgery, the medical literature related to the treatment of the gingival smile is still insufficient, incoherent, and not supported by the necessary statistical analysis [1]. APE treatment should aim to reduce excessive gingival appearance and achieve full exposure of the anatomical crown while re-establishing a suitable distance for the biological width [17].
The average age of the patients in the present study was 24.4±3.5 years, which is in accordance with many similar studies [1,5,18]. This is explained by the fact that the excessive appearance of the gingiva decreases with age, and the cosmetic needs are higher among young people. The prevalence of females in this study sample was similar to a review of the literature that showed that this condition is more common among females, and the major proportion of surgically treated cases was also among females. This may be clarified by the superior aesthetic needs of females, especially with regard to an attractive smile [5].
CBCT radiographs provide an accurate measurement of the distances between CEJ and BC and can accurately identify the length of the anatomical crown, which are considered to be the basic measurements needed for the surgical treatment of these cases [Table/Fig-3] [19].
The findings from this 3-month prospective controlled study revealed that both surgical approaches are effective in ECL. Using piezosurgery, the two techniques allowed bone reduction in an apical direction. Using a piezosurgery tip helped to successfully perform bone resection. The results showed significant increases in rBL means immediately after surgery for both the OF and FL sites. This high adequacy of piezosurgery in osteotomy has been also demonstrated through the significant increases in the CEJ-BC mean values for the OF and FL sides. We were able to establish a new biological width, 3 months after surgery in the both groups. These results demonstrate that we obtained sufficient distance for the ideal biological width measurement, which should be at least 2 mm consisting of 0.97 mm for the epithelial attachment and 1.07 mm for the connective tissue attachment [7].
The stability of the gingival margin during the healing period after ECL is unpredictable, and there was an agreement that essential tissue rebound following the ECL is often associated with thick gingival biotype and the short distance between the flap’s margin and the BC [20]. The results demonstrated a significant increase in the rGM and rCAL levels and significant decrease in the PD and KGH measurements over time compared with the baseline, which means that both of the OF and FL techniques created a significant decrease in the excessive gingival tissue. The author were able to obtain immediate improvements in the length of the clinical crown immediately after the surgery by 1.97 mm and 1.98 mm for FL and OF, respectively. These gains in length of the clinical crown continued in the two groups after 3 months. By comparing the average values at baseline and 3 months after the surgery, the final average increase in the length of the clinical crown was 1.81 mm in the FL group and 1.75 mm in the OF group. The tissue rebound phenomenon occurs as a result of the periodontal tissues’ attempt to reshape its previous dimensions during the healing and maturation periods. The dimensions of the supracrestal gingival complex should be 2.73 mm [7]. In the present study, the mean SGH values 3 months after the surgery were close to the normal dimensions. We observed a minimal tissue rebound in both groups. This rebound was slightly higher in the OF group but without significant statistical difference as compared to the FL group. In addition, traumatic surgical techniques involving osteotomy and flap reflection have been found to cause more gingival tissue rebound [7]. The tissue rebound in this study can be explained by the fact that all patients had thick gingival biotype according to the inclusion criteria, and this thick tissue biotype generally shows more tissue regrowth than thin tissue biotype [21].
The sites treated with FL showed mean BOP and GI values that were less than the OF-treated sites. The minimal difference noted in this study could be due to tissue trauma and increased recovery time after flap reflection and surgical suturing, which are required in the OF sites. These clinical results are in agreement with a previous investigation that demonstrated that the FL approach allows faster healing and less tissue inflammation compared with the OF approach [11]. These results could also be explained by the patient’s ability to resume an oral hygiene procedure faster in FL sites compared with OF sites. Nevertheless, results showed low mean values of PI over a 3-month healing period.
The mean surgical time was lower for the FL sides than for the OF sides. Using piezosurgery reduces the rate of bleeding by 25-30% because it does not cause damage to the blood vessels, which ensures clear vision during the surgery [8]. In addition, the FL approach eliminates the need for flap reflection and surgical suturing. Accelerated surgical procedures ultimately leads to less post-surgical swelling and oedema [6].
The patients included in this study showed low mean values of pain in general for the OF and FL sides. The FL approach showed significantly less pain in values compared with the OF approach. The flap reflecting causes the periosteum to split and affects the blood circulation of the underlying bone tissue, while the FL technique maintains the contact of the periosteum with the alveolar bone. The surgical suturing and increased time associated with the OF procedure could cause more oedema and haematoma after the surgery, thus causing more pain [22].
The patient’s satisfaction results in this study showed a difference between the groups. More patients who received an FL approach showed higher satisfaction when compared to those who received an OF approach. Swelling is one of the most burdensome impacts on the patient after surgery. Several factors affect the occurrence of this swelling, most importantly the surgical flap reflection, the duration of the surgery, and the surgical suturing [6]. All of these previous factors, in addition to the accelerated healing in FL sites, may clarify why FL showed more favourable results when compared with OF.
The minimally invasive surgical method used in this study reduced the surgical time in the chair, reduced the amount of trauma caused by the surgery, and accelerated the healing process with increased patient comfort. Piezosurgery offers a truly promising alternative method and showed significant benefits compared to traditional instruments of bone resection in ECL. However, the specific indications of this procedure- for example, an adequate amount of keratinized gingival tissue and a thin to moderate thickness of buccal alveolar bone-must be respected to achieve aesthetic and stable results. Flapless technique has a number of disadvantages, including the inability of the surgeon to see the anatomical and biological structures. It is also a very sensitive technique, requiring training and experience. The osteotomy on the buccal surfaces and linear angles may be difficult to perform without causing damage to the overlaying soft tissue [23]. Furthermore, this technique is performed for specific clinical cases in which the gingival biotype is least thick or medium in thickness, without a thick bony pattern because the thick bony pattern requires a complete detection of the surgical area by flap reflection [3].
Limitation
The limitation of this study was the short follow-up period, as the amount of gingival rebound increases over a period longer than 6 months.
Future Recommendations
Further long-term studies are needed to evaluate the relationship between the gingival margin level changes and different surgical methods and approaches.
Conclusion
Based on the present study, both of the flapless and the open flap approaches are effective in aesthetic crown lengthening using Piezosurgery. FL surgery for ECL showed similar clinical results to the OF technique up to 3 months. Furthermore, flapless surgery is a minimally invasive, easy, and predictable procedure with significant clinical advantages such as no surgical sutures, less bleeding, less pain, and shorter healing time.
PI: Plaque index; BOP: Bleeding on probing; GI: Gingival index; PD: Probing depth; rCAL: relative Clinical attachment level; rBL: relative Bone level; rGM: relative Gingival margin; KGH: Keratinized gingival high
*Significant differences between OF and FL groups at 3 months post surgery by independent samples t-test (p<0.05)
†Significant differences between baseline and 3 months within a group by paired samples t-test (p<0.05)
‡Significant differences between 7 days and 3 months within a group by paired samples t-test (p<0.05)
**Significant differences between baseline and immediately after surgery within a group by paired samples t-test (p<0.05)
CEJ-BC, Cemento-enamel junction to bone crest (biological width); SGH: Supracrestal gingival height
†Significant differences between baseline and 3 months within a group by paired samples t-test (p<0.05)
*Significant differences between OF and FL groups at 24 hours post surgery by independent samples t-test (p<0.05)
**Significant differences between OF and FL groups at 48 hours post surgery by independent samples t-test (p<0.05)
†Significant differences between 24 hours and 48 hours within a group by paired samples t-test (p<0.05)
*Significant differences between OF and FL groups at 7 days post surgery by independent samples t-test (p<0.05)
†Significant differences between 7 days and 3 months within a group by paired samples t-test (p<0.05)