Teaching Points: Appropriate Evaluation of Ascitic Fluid in an Acutely Ill Cirrhotic Patient
Laila Khan1, William G Simpson2
1 Senior Resident, Department of Family Medicine, Northeastern Health System, Tahlequah, Oklahoma, USA.
2 Adjunct Clinical Assistant Professor, Department of Internal Medicine, Northeastern Health System, Tahlequah, Oklahoma, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. William G Simpson, PO Box 500, Tahlequah, Oklahoma-74464, USA.
E-mail: wsimpson@nhs-ok.org
Spontaneous Bacterial Peritonitis (SBP) is a serious and dangerous complication of cirrhosis with portal hypertension. Prompt diagnosis mandates paracentesis with appropriate handling and evaluation of ascitic fluid obtained. A 37-year-old female with cirrhosis and portal hypertension, with a history of SBP, presented with abdominal pain and encephalopathy. With medical management, the encephalopathy cleared and the patient was able to return home. The presented clinical scenario provides valuable teaching insight into the need to appropriately evaluate such a patient with the mandate to diagnose spontaneous peritonitis promptly. Timely evaluation and appropriate management offers clinicians an opportunity to reduce morbidity and mortality in patients with advanced liver disease.
Ascites, Cirrhosis, Spontaneous bacterial peritonitis
Case Report
A 37-year-old female, with history of decompensated cirrhosis secondary to chronic hepatitis C infection and alcohol abuse, presented with confusion and abdominal pain that had progressively worsened over the preceding 36 hours. The patient had a history of recurrent ascites which was refractory, Spontaneous Bacterial Peritonitis (SBP) and hepatic encephalopathy. Her family reported recent non-compliance with scheduled paracentesis and medications including lactulose, rifaxaman and diuretics.
In the Emergency Department, the patient was combative and aggressive towards the staff. The patient was sedated due to concern of self-injury and injury to others as well as her interference with medical care. As a result, the patient became hypoxic and hypercarbic, and was unable to protect her airway, prompting intubation followed by admission to the Intensive Care Unit. Examination at admission demonstrated spider angiomata and palmar erythema. The abdomen was tensely distended with a fluid wave, and a large chronic umbilical hernia was intact.
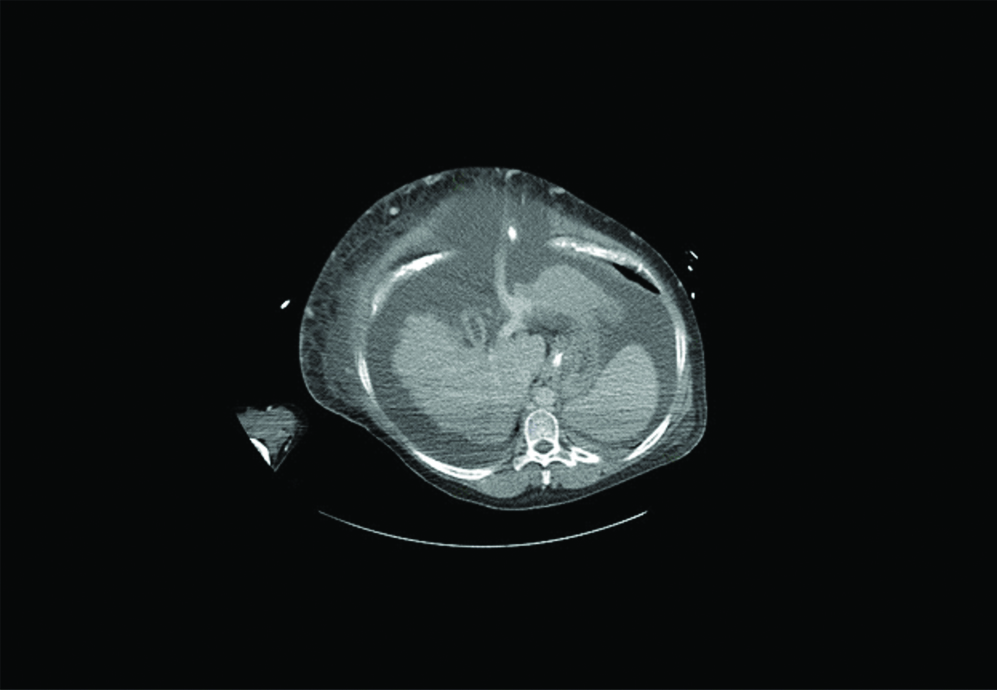
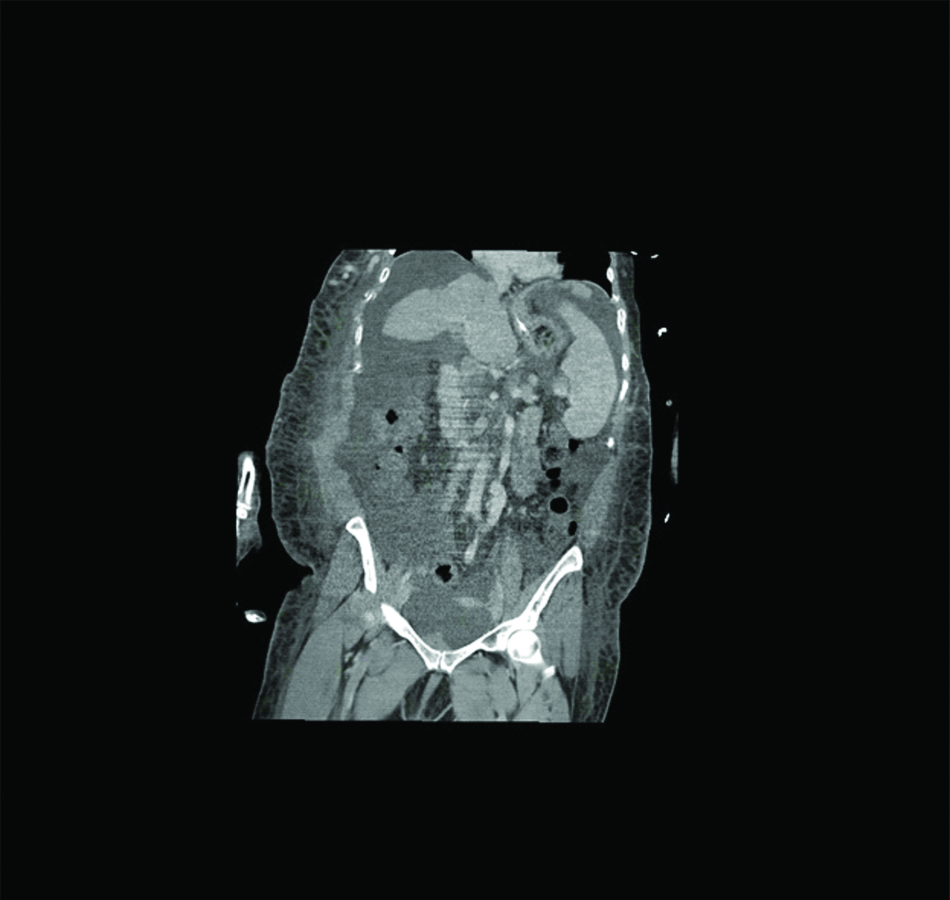
Laboratory evaluation revealed serum ammonia 380.9 μmol/L, AST 52 u/L, ALT 31 u/L, alkaline phosphatase 135 u/L, and total bilirubin 3.6 mg/dL. Serum sodium was 130 mmol/L, blood urea nitrogen 14 mg/dL, creatinine 0.8 mg/dL. The INR was 1.92. Computed tomography of the abdomen and pelvis was consistent with cirrhosis and portal hypertension with a large volume of ascites present [Table/Fig-1,2]. Notably no fluid collections, inflammatory changes or free air were present. Soon after arrival in the ICU a diagnostic paracentesis was performed. Sampled fluid revealed 45 WBC/mm3 with an absolute neutrophil count of 3, and albumin 0.2 g/dL (serum ascites albumin gradient 2.5 g/dL). A volume of fluid was transported to the laboratory where a gram stain revealed no organisms or leukocytes, and blood culture bottles were inoculated. Cultures were sterile.
Computed tomography axial image at presentation demonstrating a small nodular liver with large volume ascites. Also, noted in a large umbilical hernia containing ascitic fluid and a large caliber recanalized umbilical artery.
Computed tomography coronal image at presentation demonstrating a small nodular liver and large volume ascites.
The patient received lactulose therapy, at first by nasogastric tube and later orally, which resulted in marked improvement of her mentation. Over the first 48 hours of hospitalisation, the patient’s mental status became more lucid and extubation was possible. On sixth hospital day, the patient was discharged at her baseline with reinstitution of her medicines and reinforcement of the need for compliance.
Discussion
The development of portal hypertension in patients with cirrhosis is associated with a cascade of physiologic aberrations that may result in the pathologic accumulation of fluid in the peritoneal cavity. Ascites develops within 10 years in approximately 70% of patients with cirrhosis [1]. Translocation of gut bacteria may play a role in the development of ascites, refractory ascites and infection of this accumulated peritoneal fluid. SBP is diagnosed when aspirated ascitic fluid demonstrates an absolute neutrophil count >250 cells/mm3 or is culture positive [2,3]. Typically, this is a mono-microbial infection involving organisms common in the gut, as contrasted to polymicrobial infections resulting from an intraperitoneal abscess or perforated viscus. While SBP may present with abdominal pain and/or fever in a patient with ascites, many cirrhotic patients present with more subtle manifestations including altered mental status or worsening hepatic encephalopathy, hypothermia, worsening renal insufficiency, hypotension, gastrointestinal bleeding or an ileus. Some patients may manifest no symptoms at all. SBP is the most common bacterial infection diagnosed in patients with cirrhosis and is associated with a poor prognosis [3]. Undesirable outcomes including acute kidney injury (54%), acute-on-chronic liver failure (60%) and death (40%) are frequent following SBP. Diagnosis of SBP requires diagnostic paracentesis, and clinical diagnosis with empiric antibiotic therapy is not appropriate [4].
Prompt recognition and institution of appropriate management of SBP requires diagnostic paracentesis, which should be performed at presentation with ascites, at the time of any hospital admission of a cirrhotic with ascites, and at the time of any significant change in clinical status while such a patient is hospitalised. The appropriate timing of paracentesis must be coupled with an understanding of the appropriate studies to be performed on the acquired fluid sample. The choice of tests ordered depends on the clinical setting in which paracentesis is performed. All samples should have a cell count and differential performed and should be cultured. Calculation of the absolute neutrophil count can be accomplished rapidly and allows early institution of antimicrobial therapy and albumin infusion when appropriate. As SBP is a mono-microbial infection with a low concentration of organisms, similar to that of blood during bacteremia, the yield is significantly increased if fluid is inoculated into blood culture bottles directly at the bedside [2-4]. Runyon B et al., demonstrated a significant fall in culture positivity if samples were transported to the laboratory where the fluid was inoculated into blood culture bottles versus those inoculated immediately at the bedside [5]. Total protein and albumin levels are appropriate in the initial evaluation of ascites.
A gram stain is commonly performed inappropriately in the evaluation of patients with ascites, as was the case in the patient reported. The low concentration of bacteria in infected ascitic fluid results in the very low yield of gram staining in SBP, and the yield is not increased by centrifugation of the specimen [6]. This contrasts with secondary peritonitis where the infection is polymicrobial and the bacterial density is dramatically higher. Akriviadis E et al., did not include gram stain in a clinical algorithm which discerned secondary peritonitis with 100% sensitivity versus SBP [7]. A suspicion of secondary peritonitis is better evaluated with imaging (CT scan) than through peritoneal fluid analysis [4]. Particularly in patients with an established diagnosis of cirrhosis and portal hypertension resulting in ascites, the extremely low yield of routine ascitic fluid gram stain does not justify the time or cost of performance of the test. Importantly, a negative gram stain should in no way delay appropriate culture inoculation, the diagnosis of SBP or the initiation of therapy. An understanding of the pathophysiology and clinical consequences of SBP result in a clear understanding of the appropriate evaluation of a cirrhotic patient, and support the general avoidance of routine gram staining of fluid collected at diagnostic paracentesis. Bedside inoculation of an adequate volume of fluid into blood culture bottles significantly increases yield and has become the current standard of care.
Conclusion
A patient with cirrhosis and ascites who presents with a decompensation of hepatic encephalopathy was presented in the article, to review several important aspects of acute management. The presence of SBP needs to be defined promptly to allow initiation of therapy. Diagnostic paracentesis is safe and should be performed soon after presentation. Ascitic fluid gram stain is of low yield and should only be ordered if secondary peritonitis is a concern. Rather, cell count and differential allow establishment of a diagnosis. Prompt inoculation of fluid into blood culture bottles at the bedside offers the best opportunity to identify the infecting organism.
[1]. Adebayo D, Neong S, Wong F, Refractory ascites in liver cirrhosisAm J Gastroenterol 2019 114(1):40-47.10.1038/s41395-018-0185-629973706 [Google Scholar] [CrossRef] [PubMed]
[2]. Runyon B, Management of adult patients with ascites due to cirrhosis: Update 2012Hepatology 2013 57(4):01-26.10.1002/hep.2635923463403 [Google Scholar] [CrossRef] [PubMed]
[3]. Marciano S, Diaz J, Dirchwolf M, Gadano A, Spontaneous bacterial peritonitis in patients with cirrhosis: Incidence, outcomes, and treatment strategiesHepat Med 2019 11:13-22.10.2147/HMER.S16425030666172 [Google Scholar] [CrossRef] [PubMed]
[4]. European Association for the Study of the LiverEASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosisJ Hepatol 2010 53(3):397-417.10.1016/j.jhep.2010.05.00420633946 [Google Scholar] [CrossRef] [PubMed]
[5]. Runyon B, Antillon M, Akriviadia E, McHutchinson J, Bedside inoculation of blood culture bottles with ascitic fluid is superior to delayed inoculation in the detection of spontaneous bacterial peritonitisJ Clin Microbiol 1990 28(12):2811-12.10.1128/JCM.28.12.2811-2812.19902280015 [Google Scholar] [CrossRef] [PubMed]
[6]. Runyon B, Canawati H, Akriviadis E, Optimization of ascitic fluid culture techniqueGastroenterology 1988 95(5):1351-55.10.1016/0016-5085(88)90372-1 [Google Scholar] [CrossRef]
[7]. Akriviadis E, Runyon B, Utility of an algorithm in differentiating spontaneous from secondary bacterial peritonitisGastroenterology 1990 98(1):127-33.10.1016/0016-5085(90)91300-U [Google Scholar] [CrossRef]