CVT is one of the infrequent causes of stroke with enormously varied clinical presentations, predisposing factors, radiological findings and outcomes. The diagnosis of CVT is always a clinical dilemma for the treating physician because of its myriad presentation. It’s incidence during pregnancy and puerperium is reported to be 11.6 per 100,000 deliveries per year, accounting for 6-64% of pregnancy-related strokes in developed countries [1]. However, in developing countries like India, due to lack of any population-based study or nationwide multicentric studies, the exact incidence of CVT is still not clear and have been reported to be as high as 450 per 100,000 deliveries per year [2].
It occurs more commonly in cases of pre-eclampsia, sepsis and/or when certain prothrombotic conditions are present. There is a greater risk of CVT during the third trimester of pregnancy and in the first four postpartum weeks. It most often involves the superior sagittal sinus but may occur anywhere in the cerebral venous circulation. MRI combined with MRV is the best diagnostic methods. With the advent of these newer and more sophisticated imaging techniques and increasing awareness of this entity, the incidence of this disease has increased and the prognosis has improved. The aim of this study was to assess the demographic profile, frequency of different clinical features, risk factors and prognostic outcome in patients diagnosed as CVT in Andaman and Nicobar Islands, India.
Materials and Methods
This was a hospital based prospective observational study conducted in the Department of Obstetrics & Gynaecology and the Department of Medicine of the only tertiary hospital of Andaman & Nicobar Islands, from January 2015 to December 2016. Ethical clearance was taken from the institutional ethics committee.
All cases of cerebrovascular accidents were followed and only those cases diagnosed as CVT on the basis of CT, MRI and MRV were included in the study after written informed consent. The cases where imaging could not be done and those who were not pregnant or puerperal, were excluded. At the end of each month, the medical records of all obstetric admission cases in maternity ward, medicine ward and medical intensive care unit were screened so as not to miss any case.
A detailed history of symptomatology along with their demographic profile, presence of high-risk factors, previous history of thromboembolism, family history of hyper-coagulable states, delivery details and post-partum period was taken. Clinical examination was done and blood invesigations like complete haemogram, co-agulation profile, liver and renal function tests were done. Cases were included and followed, if, on NCCT (non-contrast CT), there was spontaneous hyperdensity of a cortical vein or dural sinus while on CECT, empty delta sign and empty lateral sinus sign were seen. On MRI, the inclusion criteria were hyperintense signal on T1 and isointense to hyperintense signal on T2 sequences and on MRV, abnormal defect or rupture of the sinus. The MRI T1 and T2 weighted scans were done in axial, sagittal and coronal slices on 1.5 Tesla machine.
All diagnosed cases were followed till their stay in hospital and three months later to see for recovery and any residual signs and recanalization. Treatment modality consisted of anticoagulation with body weight adjusted low molecular weight heparin followed by warfarin, anti-oedema measures and supportive therapy. Antiepileptic medication was instituted when required. Data was then tabulated and statistically analysed by using SPSS software version 21.
Results
Out of total of 4,767 deliveries in the study period, we found six cases of puerperal CVT and none were during pregnancy. The incidence of CVT during puerperium, was 125.8 per 100,000 deliveries. Interestingly, there was neither any case of CVT in non-pregnant females nor in males during the study period. The mean age of women presenting with CVT was 23.6±3.204 years ranging between 20-28 years. A 50% of the study cases (3/6) were primipara. Three cases had vaginal delivery while the remaining three cases delivered by caesarean section. Five out of 6 cases delivered live babies and one delivered a dead macerated baby. [Table/Fig-1] shows the demographic profile of cases and their outcome at three months post-insult. None of the present cases was obese or overweight or had history of use of oral contraceptive pills prior to pregnancy. Only one case had pre-eclampsia superimposed on chronic hypertension in the current pregnancy. The most common presenting symptom was headache (6/6, 100%) followed by seizures (4/6, 66.6%) and then hemiparesis. One case presented with diplopia and one with blindness which reversed following treatment [Table/Fig-2]. The most common area of infarct was superior sagittal sinus (6/6, 100%) [Table/Fig-3].
Profile of cases diagnosed as CVT.
| Cases | Age (Years) | Parity | Mode of delivery | Fetal outcome | Maternal outcome |
|---|
| 1 | 24 | P4001 | Vaginal | Dead | Recovered |
| 2 | 20 | P1001 | LSCS | Live | Recovered |
| 3 | 28 | P1001 | LSCS | Live | Recovered |
| 4 | 20 | P1001 | LSCS | Live | Died |
| 5 | 26 | P2002 | Vaginal | Live | Recovered |
| 6 | 24 | P2002 | Vaginal | Live | Recovered |
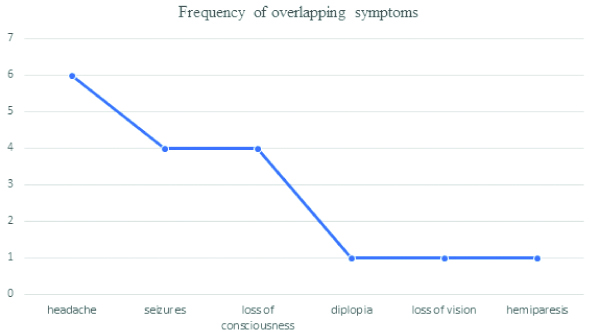
Clinical presentation and areas of infarct in cases diagnosed as CVT.
| Cases | Onset of symptoms | Presentation | Site of infarct |
|---|
| 1 | Day 8 | Headache, sleeplessness, diplopia, hemiparesis | Anterior cerebral venous thrombosis involving superior sagittal sinus and lateral sinus [Table/Fig-4,5]. |
| 2 | Day 7 | Headache, seizure | Superior sagittal sinus with right temporal, parietal and occipital and left parietal area. |
| 3 | Day 8 | Headache, seizure | Superior sagittal sinus involving Bilateral basal ganglia and occipital lobe infarct. |
| 4 | Day 7 | Headache, seizure | Superior sagittal sinus. |
| 5 | Day 10 | Headache, loss of vision | Superior sagittal sinus involving bilateral parietal lobe, bilateral subcortical region in occipital lobe, right centrum semiovale and right temporal lobe. |
| 6 | Day10 | Seizure, headache | Superior sagittal sinus and internal juglar vein. |
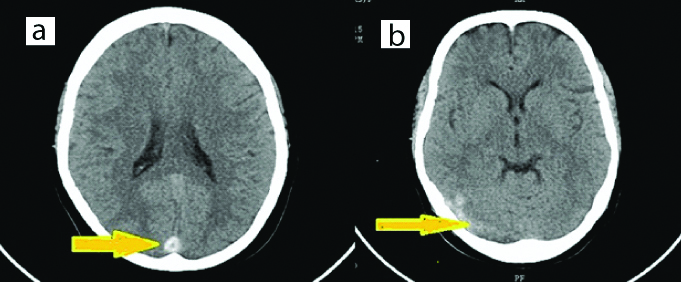
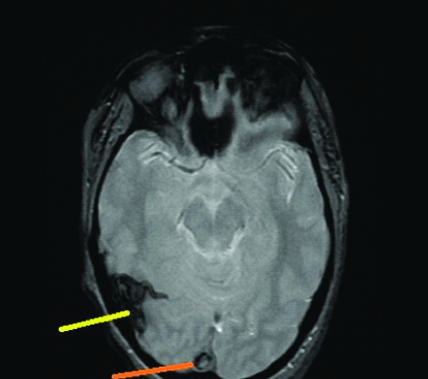
On imaging, the characteristic linear cord sign on CT could be seen only in one case [Table/Fig-4]. We could well appreciate the superior sagittal sinus thrombosis and lateral sinus thrombosis on non-contrast CT scan in [Table/Fig-4] and in MRI in [Table/Fig-5]. The average period between the onset of symptoms and consultation was 1.8 days. Five out of six patients received anti-coagulant therapy with low molecular weight heparin followed by maintenance on warfarin. One patient died before treatment could be initiated. Mortality at discharge was 16.6% (1/6) and nil at 3 months. During follow-up at 3 months, complete recovery was seen in all the cases who were alive.
a) Non-contrast Computed Tomogram (CT) showing hyperdense linear cord sign (yellow arrow), involving the superior sagittal sinus; b) Non-contrast computed tomogram (CT) showing hyperdense lateral sinus involvement (yellow arrow).
Magnetic Resonance Imaging (MRI) showing hyperintense lateral sinus (yellow arrow) and superior sagittal sinus (orange arrow).
Discussion
Cerebral venous thrombosis is not as common as arterial thrombosis. However, if diagnosed timely, has a good prognosis and recovery. The incidence of CVT in our hospital was higher (125.8/100,000 deliveries) than the reported incidence in developed countries but lower than that in developing countries (450 and 202/100,000 deliveries) [2-5].
Additionally, Andaman and Nicobar Islands are a group of islands located 1400 km from the mainland India. There is only one tertiary referral hospital situated in the capital city of Port Blair. Access to health care is a major issue in this island. It is not a very big problem for people residing in Port Blair or nearby areas but for those residing in remote islands, if such complications occur in pregnancy or puerperium, connectivity is a major problem. Cases have to be ferried by helicopters in such emergent conditions.
CVT is a challenging condition because of its varied clinical presentation usually beginning with severe headache and may lead to seizures, neurological deficit and even death. The results of the International study on cerebral vein and dural sinus thrombosis, revealed that the commonly affected site is the transverse sinus, followed by superior sagittal sinus and straight sinus [5]. Whereas a reasonably good number of studies claim superior sagittal sinus as the common site of involvement [6,7]. Our study also documented the similar findings.
Evaluation of the patients with venous thrombosis becomes fairly easier if one has a sound background knowledge of the venous system anatomy since most of the symptoms associated with the condition co-relates to the area of thrombosis [8]. For example, involvement of superior sagittal sinus may lead to headache, increased Intracranial pressure (ICP) and papilloedema. Lateral sinus thrombosis may be associated with fever, ear discharge, ear pain and headache. Cortical involvement may present with hemianopia, contralateral weakness and aphasia. Jugular foramen syndrome or cranial nerve palsies may occur if there is involvement of jugular bulb and cavernous sinus thrombosis respectively [8]. The headache of CVT is usually progressive, atypical and does not respond to analgesics and may develop over the several days, leading to an average time between symptom onset and diagnosis of seven days or more. In our study, most of the patients were referred to the hospital within 48 hours of symptom onset. However, the time taken to reach the diagnosis was variable depending upon the clinical presentation. Approximately 16% patients with CVT have thrombosis of the deep cerebral venous system (internal cerebral vein, vein of Galen and straight sinus) which can lead to thalamic or basal ganglia infarction [6] as it was seen in two of our cases. These patients may present with alteration in the level of consciousness without focal neurological findings. In many patients, thrombosis may occur in more than one sinus. In our study, superior sagittal sinus was involved in all the cases along with other sinuses.
In patients where CVT is suspected or diagnosed, besides starting the treatment, a complete work-up is recommended to know the cause for this condition. This includes history of use of contraceptives, any underlying inflammatory disease or infectious process and investigations like complete blood count, prothrombin time, activated partial thromboplastin time, tests for protein C, protein S, or antithrombin III, anti-phospholipid antibody syndrome, prothrombin G20210A mutation and factor V Leiden mutation [6].
Eclampsia and CVT can be confused with each other especially when they develop in the background of pre-eclampsia [9]. One of our cases (case 6) suffered from convulsive episodes during the postpartum period which led to the initiation of treatment for eclampsia as she also had signs of pre-eclampsia before delivery. However, even after initiation of anti-eclamptic treatment, the convulsions continued and she had increasing somnolence. Radiological examinations later disclosed the diagnosis of CVT. Hence in such settings when seizures continue despite medications, one must think beyond Eclampsia. CVT usually presents either late in pregnancy or puerperium but cases have been reported as early as eight weeks [10]. Most of the studies from Indian subcontinent have reported a higher incidence of CVT during puerperium as compared to pregnancy [7,11]. Our study also supports the similar results. However, studies from United States report more or less similar proportion during pregnancy and puerperium [5,12]. Higher risk during puerperium can be attributed to some age-old rituals of depriving the delivered woman of adequate diet, salt and water for few days following delivery. Besides these, hyper-coagulability plays an important role in the development of CVT during pregnancy and puerperium. Additionally, hypovolemia secondary to post-partum haemorrhage, trauma during delivery and venous stasis due to traditional practices of prolonged bed rest may further add to the prothrombotic tendency during pregnancy. The hypercoagulability and venous occlusion of cerebral veins lead to cytotoxic and vasogenic oedema and further infarction while occlusion of major sinuses leads to intracranial hypertension [13].
In 30% cases, no underlying aetiology can be identified [14]. In the present study, one case had pre-eclampsia, three cases had caesarean sections and one case had bad obstetric history with intra-uterine foetal demise in the current pregnancy (case 1).
All cases were screened for common prothrombotic conditions after six weeks of delivery and the results were negative.
There is paucity of data on long term outcome of obstetric CVT including recurrence during subsequent pregnancy. We could search only one study that reported that there is no substantial risk of CVT during subsequent pregnancy in women who had CVT in past whether obstetric or not. None of their patients developed CVT over a mean follow-up of 10 years [15].
A high degree of clinical suspicion is required to diagnose CVT and for confirmation, imaging is must. The imaging findings can be direct when there is direct visualisation of thrombus in the sinuses and indirect when there are ischemic changes due to the venous outflow disturbances. CT is usually the first, and in a country like ours, the only investigation performed in the emergency setting. In about one-third of cases, one can observe the direct signs of CVT on contrast tomography like cord sign, dense triangle sign or empty delta sign. The cord sign on CECT is the visualisation of the hyperdense thrombosed cortical vein; Dense triangle sign on non-contrast CT (NCCT) is the visualisation of a fresh thrombus in the posterior part of the sagittal sinus whereas empty delta sign is seen as as non-filling of the confluence of sinuses after contrast injection [8,13].
Currently, the gold standard investigation in the diagnosis of CVT is to combine MRI and MRV for visualising the thrombosed vessel [12,13]. The MRI alone is limited by flow artifacts that can lead to false positives and the absence of hyperintense signal on T1 and T2-weighted images at the onset of acute thrombosis. But if we combine MRV with MRI, the sensitivity definitely increases.
According to the guidelines of the European Federation of Neurological Societies, the first line treatment for cerebral venous and dural sinus thrombosis is anti-thrombotic treatment. The rationale for use of anti-thrombotic treatment is to favour spontaneous thrombus resolution and to recanalize the occluded vein or sinus, to avoid thrombus propagation, to treat underlying prothrombotic condition and to prevent complications such as pulmonary thrombo-embolism [16,17]. Treatment is usually started with body-weight-adjusted subcutaneous Low-Molecular-Weight Heparin (LMWH), until the patient stabilises. Once the acute phase is over, warfarin is usually started overlapping with LMWH to prevent recurrence and thrombosis in other parts of the body. The aim is to maintain an International Normalised Ratio (INR) between 2.0-3.0. In the present study five out of six cases received LMWH subcutaneously and responded within mean duration of 24-48 hours. In one case which presented with post-partum seizures, patient expired before treatment could be initiated. There is paucity of data on current recommendations on the safety and efficacy of thrombolytic therapy, either local or systemic, in patients of CVT. Even the RCTs (Randomised controlled trials) do not provide enough evidence in this context [12].
All cases were followed at three months post-event to check for recanalization. The overall mortality in CVT was found to be 3%-15% [5,11,18]. Coutinho JM et al., recognised complete recovery in 81% of women, dependency or death in 12%, and mortality in 6% of women with CVT [18]. Similar results were observed in two other prospective studies [19,20]. In our study also, 83.3% (5/6) patients had total recovery and mortality was 16.6% (1/6). Subsequent pregnancies are safe, but use of prophylactic LMWH should be considered throughout pregnancy and puerperium [21].
Limitation
Few prothrombotic conditions requiring mutation analysis could not be evaluated due to the remoteness of our place from the mainland. This was one of the limitations of our study.
Conclusion
CVT is more common during the puerperium than in the antenatal period. However, despite having such a myriad presentation and an acute onset, it has an excellent recovery when promptly diagnosed and treated.