Patients with incidental bullous lesion of lung occasionally present for non-thoracic surgeries, these patients are at increased risk of potential complications which can arise due to bullae, during perioperative period. Anaesthetic management of these patients planned for a major non-lung volume reduction surgery is challenging as it is rare and requires careful understanding of anatomical and pathophysiological variation of disease. Safe conduct of anaesthesia can be delivered without isolation of the lung or sub-segment in which bulla is involved in these patients so that perioperative respiratory crippling conditions like pneumothorax, emphysema, atelectasis of the surrounding lung parenchyma leading to postoperative respiratory failure can be avoided. Eternal vigilance, monitoring, ventilator strategies are required to avoid possible perioperative complications and a successful outcome, few essential precautionary measures to be taken include vigilant monitoring of patient perioperatively, avoidance of nitrous oxide, low airway pressures, immediate availability of chest drains, periodic auscultation of chest, arterial blood gas analysis. Here, the present authors report a successful perioperative anaesthetic management of a patient with giant bulla in left upper lobe and right upper lobe developed as post tubercular sequelae that underwent inferior partial maxillectomy with neck dissection and reconstruction for carcinoma upper alveolus without isolation of lung.
Case Report
A 42-year-old male diagnosed with right sided carcinoma of upper alveolus was planned for inferior partial maxillectomy with neck dissection and reconstruction. He was a manual labourer, non-smoker-alcoholic, known tobacco chewer for past 25 years with a history of pulmonary tuberculosis, six years back, for which he was treated and declared sputum negative. A chest skiagram was taken soon after admission revealed giant bullae in left upper zone and right upper zone. He gave no history of recurrent respiratory tract infections or spontaneous pneumothorax in recent past.
On examination he was malnourished with BMI of 13.8 kg/m2, air entry was equal bilaterally with harsh breath sounds in bilateral infra-clavicular region, another systemic examination were normal and airway was not difficult except for cancerous lesion of approximately 2 cm×1 cm with erosion at left upper alveolus posterior to 2nd molar teeth.
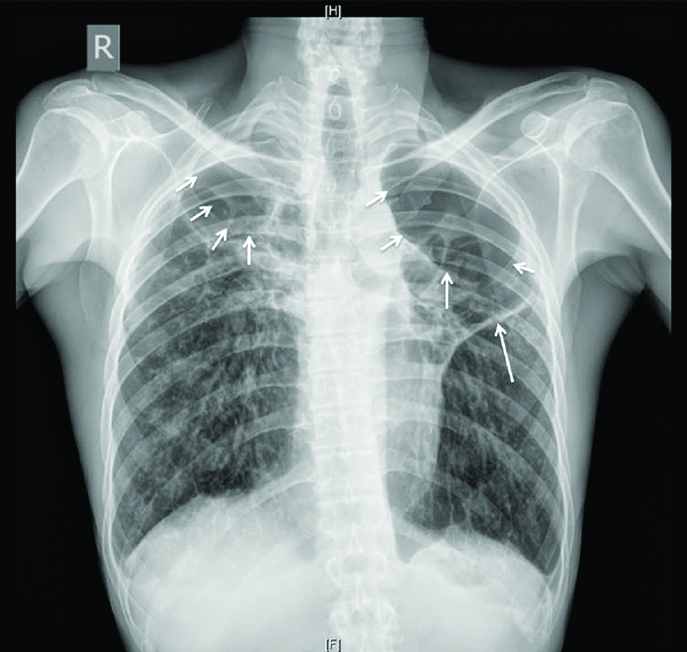
Patient’s complete blood picture was within normal limits, chest radiograph PA view showed a giant bulla over left upper zone and right upper zone with hyperinflation of bilateral lung fields, relatively well-defined area of lucency with rim of outline in bilateral upper zone lung fields with absence of bronco-vascular markings–features suggesting bullous emphysema [Table/Fig-1]. Electrocardiogram (ECG) showed incomplete Right Bundle Branch Block (RBBB), right ventricular hypertrophy for which cardiology opinion was sought to rule out any cardiac complications, a 2-D echocardiography was normal with ejection fraction of 65% and mild pericardial effusion.
Chest radiograph-PA view with hyperinflation of bilateral lung fields with well-defined areas of lucency with absence of broncho-vascular markings (features representing bullous emphysema).
Pulmonology evaluation graded patient as high risk for surgery, with Pulmonary Function Test (PFT) revealing very severe airflow limitation and ineffective cough mechanism, Forced Vital Capacity (FVC) 35% of predicted, Forced Expiratory Volume 1 second (FEV1) 31%, FEV1/FVC ratio of 111% and no significant reversibility with bronchodilators. A High Resolution Computed Tomography (HRCT) was unaffordable for patient. His room air saturation was 92-94% and room Air Arterial Blood Gas (ABG) analysis showed pH- 7.46 pO2- 90 mmHg, pCO2- 48 mmHg, HCO3- 22 meqvL, his functional capacity was fair with a metabolic equivalent of more than 6 and Assess Respiratory Risk in Surgical Patients in Catalonia (ARISCAT) score [1] of 24 points (low risk). He was optimised with chest physiotherapy, incentive spirometry, and nebulisation with ipratropium and salbutamol preoperatively as advised by pulmonologist. However, due to giant bulla further improvement of functional capacity of lung was doubtful.
After explaining perioperative pulmonary complication it was planned to proceed for surgery under general anaesthesia with controlled ventilation. Appropriate concent was obtained from the pateint. Patient was premedicated with Tab.alprazolam 0.5 mg and Tab.pantoprazole 40 mg night before and on day of surgery, received ipratropium-salbutamol nebulization prior to call to Operation Theatre (OT). In OT standard ASA monitors were connected and premedicated with midazolam 1 mg, morphine 4.5 mg intravenously (iv), before conduct of anaesthesia, left radial artery was cannulated in anticipation of serial ABG analysis and also used for perioperative hemodynamic monitoring. Surgeons were alerted for emergency intercostal drainage in case of inadvertent pneumothorax during the course of anaesthesia.
Anaesthesia was induced with fentanyl 80 μg, propofol 80 mg iv and succinylcholine 80 mg after precurarization. Airway was secured with 8.5 cuffed Endotracheal Tube (ETT) orally. ETT cuff was inflated with pressure monitor reading 15 cm H2O which was sufficient to prevent leak around ETT. Anaesthesia was maintained with 50% air in oxygen and Total Intravenous Anaesthesia (TIVA) with propofol (75 mcg/kg/minute), fentanyl (2 mcg/kg/hour) infusion with BIS monitor target of 40-60. Muscle relaxation was maintained with vecuronium bromide at 0.1 mg/kg, anaesthesia workstation was set to deliver a tidal volume of 220 to 250 mL at Peak Inspiratory Pressures (PIP) of 12 cm H2O (pressure controlled ventilation), Plateau Pressure (Pplat) 13 cm H2O and Respiratory Rate (RR) 12 breaths per minute with End Tidal CO2 (EtCO2) maintained around 35-40 mmHg.
As surgery proceeded there was a gradual rise in EtCO2 up to 55-60 mmHg, ABG done showed pH-7.21 pCO2- 64.3 pO2-101 HCO3- 28 necessitating increase of PIP to 15 cmH2O, RR to 15 bpm with a Pplat of 13 cm H2O, this ensured delivery of tidal volume 280-300 mL with EtCO2 of 40-45 mmHg. Surgery was completed uneventfully, fentanyl and propofol infusions were stopped 20 and 5 minutes before end of surgery, total dose of propofol and fentanyl for entire surgical duration of 2 hour 50 minutes was 600 mg and 200 μg respectively. Muscle relaxation was reversed with neostigmine 2.1 mg and glycopyrrolate 0.4 mg iv with retention of ETT as is the practice in the institution, to avoid tracheostomy following airway obstruction in major upper airway surgeries after reversal. A further dose of morphine 3 mg iv was given to suppress cough response and patient shifted to onco-surgical intensive care unit. Oxygen was supplemented overnight, analgesia maintained with infusion fentanyl 20 mcg/hour, morphine 3 mg iv sixth hourly and paracetamol 1000 mg iv eighth hourly.
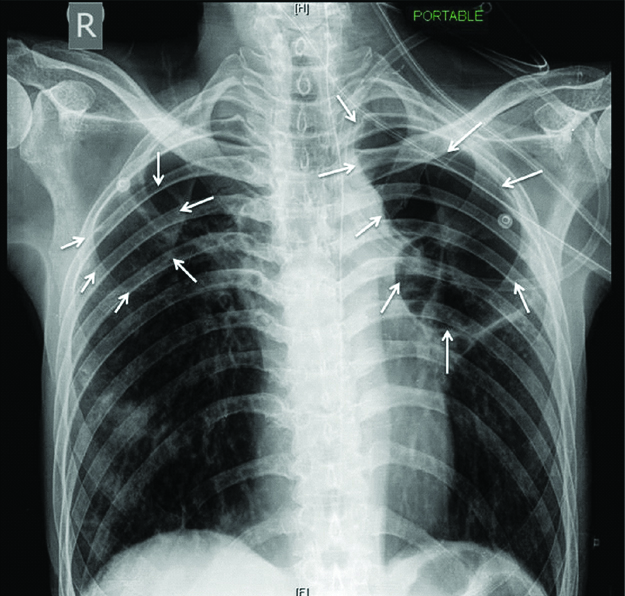
Patient was extubated on postoperative day 1, pre-extubation ABG was similar to preop with pH- 7.32, pCO2- 53, pO2-86, HCO3-26, chest radiograph was taken after extubation which showed no evidence of rupture of bullae or pneumothorax [Table/Fig-2]. The postoperative course was uneventful and he got discharged on postoperative day five without any further complications.
Postoperative bed-side AP chest radiograph after extubation showing hyperinflation of bilateral lung fields with persistence of well-defined lucency in bilateral lung fields suggesting no evidence of any rupture or pneumothorax.
Discussion
Pulmonary bulla, by definition refers to dilated air spaces of more than 2 cm diameter distal to the terminal bronchiole, if bulla occupies more than half of the lung parenchyma it is considered as giant [2]. Literature describes giant bullae as those encompassing more than one-third of lung volume [3]. Patients with giant bullae either unilateral or bilateral usually present for LVRS [4], for which one of various lung isolation techniques can be considered to deliver anaesthesia but patients presenting for non-thoracic surgery like upper airway surgery for carcinoma is rare and their perioperative management requires meticulous attention and planning [5-7].
Symptomatic bullae and their associated complications lead to two complex entities: 1) Further enlargement of bullae during anaesthesia; 2) Emphysema of healthy tissue around it worsening ventilation perfusion. So maintenance of adequate Fraction of Inspired Oxygen (FiO2) to avoid perfusion mismatch with minimal ventilating pressures in perioperative period is one of the primary goals as lung surrounding bullae is more compliant and pressure required to inflate it exceeds the pressure necessary to inflate bullae and hence when exposed to same negative intrapleural pressure, bullae will fill preferentially before normal lung [8]. Hence, chance of tension pneumothorax is high requiring immediate management [4].
While asymptomatic bullae are conservatively managed by reassurance, smoking cessation, avoiding strenuous activities promoting rupture of bullae, periodical chest radiographs and visits to physician as and when required. LVRS is planned when large bullae filling more than 30% of hemi-thorax causing incapacitated dyspnea. The index patient had severely compromised PFT, but fairly enough functional capacity and his ARISCAT score [1] was 24 which aided in planning and proceeding for surgery.
Usual complications anticipated in patients with bullae include infection, spontaneous pneumothorax, haemorrhage due to vascular damage presenting as haemoptysis, persistent hypoxemia despite adequate oxygenation due to alveolar damage, pneumopericardium and death despite initiation of cardiopulmonary bypass [9].
Precautions to be taken while administering anaesthesia include periodic chest auscultation, using larger ETT, using high FiO2 levels or an air: oxygen mixture, vigilant monitoring of ventilator parameters, maintenance of PIP <20 cm H2O, Pplat <30 cm H2O, tidal volume of 5-6 mL/kg, allowing permissive hypercapnia and increased expiratory time to prevent air trapping (I:E ratio 1:4-1:5), good intraoperative analgesia, promoting early and smooth extubation and taking measures to reduce cough and postoperative sore throat. Dutta B and Gangaprasad, reported a successful management of patient with giant pulmonary bulla undergoing laparoscopic cholecystectomy implemented similar ventilatory strategies [5].
Along with above mentioned strategies, it also requires avoidance of: a) Hyperventilation with high tidal volumes; b) Use of nitrous Oxide (N2O) -whichever mode of ventilation, as it causes expansion of air filled cavities; c) PEEP-since elasticity of lung is lost, gases accumulate in alveoli generating auto PEEP, causing dynamic hyperinflation of lung [10].
Postoperative sore throat might lead to frequent coughing which results in undue stress on bullae; the present authors could minimise this by maintaining minimal ETT cuff pressures, avoided N2O and by preferring TIVA over volatile agents as it prevents irritation of airway by suppressing cough reflexes at emergence and also decreases postoperative nausea and vomiting. Theodare B et al., in their case report on successful management of a patient with the communicating bulla coming for nonthoracic surgery gave xylocaine iv (1.5 mg/kg) to facilitate smooth extubation without coughing [2]. In the index case since the present authors retained the ETT, for tolerance, also maintained fentanyl iv infusion, morphine iv at regular intervals which aided in cough suppression and ETT tolerance in the postoperative period.
Alternatively, for ETT tolerance and analgesia, dexmedetomidine infusion (0.2-0.7 mcg/kg/hour) can be used as it reduces coughing on tube, provides sedation and reduces the dose of adjuvant analgesic requirement [11]. In the index patient dexmedetomidine was avoided because of pre-existing RBBB which is a relative contraindication [12]. Apart from that immediate availability of chest drain, meticulous monitoring, ABG to guide ventilation, chest radiograph for detection of any adverse consequences during perioperative period are also important management strategies.
From the case report, the present authors want to highlight the preoperative evaluation, vigilant smooth conduct of anaesthesia, perioperative ventilatory strategies which could be followed for better outcome in patients with bullae of lung coming for non-lung volume reduction surgeries without facilitating isolation of lung and maintenance of ETT in the postoperative period to preserve airway by avoiding tracheostomy following major airway surgeries.
Conclusion
Patients coming for non-thoracic surgery with coincidental finding of giant bullae are not much described in literature, making it rare clinical scenario. Anaesthesiologists should anticipate and be prepared for all possible complications that may arise due to giant bullae, in the perioperative period and for situations demanding retention of ETT during the immediate postoperative period, measures should be taken to avoid straining and coughing on tube, so that inadvertent rupture of bullae can be avoided.
[1]. Canet J, Gallart L, Gomar C, Paluzie G, Vallès J, Castillo J, Prediction of postoperative pulmonary complications in a population-based surgical cohortAnaesthesiology 2010 113(6):1338-50.10.1097/ALN.0b013e3181fc6e0a21045639 [Google Scholar] [CrossRef] [PubMed]
[2]. Theodare B, Nissy VV, Sahajanandan R, Mariappan R, Anaesthetic challenges of a patient with the communicating bulla coming for nonthoracic surgeryAnn Card Anaesth 2018 21:200-02. [Google Scholar]
[3]. Shah NN, Bhargava R, Ahmed Z, Pandey DK, Shameem M, The vanishing lung Lung IndiaCJEM 2007 924:233-34.10.1017/S1481803500015098 [Google Scholar] [CrossRef]
[4]. Brown AI, Anaesthesia for the respiratory crippleProc R Soc Meal 1966 59:522-27.10.1177/003591576605900618 [Google Scholar] [CrossRef]
[5]. Dutta B, Gangaprasad Anaesthetic management of a case of giant pulmonary bulla undergoing laparoscopic cholecystectomyJ Anaesth Clin Res 2012 3:21410.4172/2155-6148.1000214 [Google Scholar] [CrossRef]
[6]. Sahoo RK, Nair AS, Kulkarni V, Mudunuri R, Anaesthetic consideration in a patient with giant bilateral lung bullae with severe respiratory compromiseSaudi J Anaesth 2015 9:493-95.10.4103/1658-354X.16512826543479 [Google Scholar] [CrossRef] [PubMed]
[7]. Iwakura H, Kishimoto T, Takatori T, Koh J, Nakamura Y, Kosaka Y, Anaesthetic management of a patient with Abdominal Aortic Aneurysm (AAA) with giant bullaMasui 1994 43:116-18. [Google Scholar]
[8]. Morgan MD, Edwards CW, Morris J, Matthews HR, Origin and behaviour of emphysematous bullaeThorax 1989 44:533-38.10.1136/thx.44.7.5332505400 [Google Scholar] [CrossRef] [PubMed]
[9]. Greenberg JA, Singhal S, Kaiser LR, Giant bullous lung disease: evaluation, selection, techniques, and outcomesChest Surg Clin N Am 2003 13:631-49.10.1016/S1052-3359(03)00095-4 [Google Scholar] [CrossRef]
[10]. Elayaperumal AK, Jackson RE, Anaesthesia for lung volume reduction surgery and endobronchial valvesBJA Educ 2018 18:193-98.10.1016/j.bjae.2018.04.002 [Google Scholar] [CrossRef]
[11]. Ramakrishnan R, Koshy RC, Rajasree O, Efficacy of Dexmedetomidine for endotracheal tube tolerance, analgesia and sedation- A prospective randomised double blind controlled trialEgyptian Journal of Anaesthesia 2016 32(1):131-36.10.1016/j.egja.2015.09.005 [Google Scholar] [CrossRef]
[12]. Afshani N, Clinical application of dexmedetomidineSouthern African Journal of Anaesthesia and Analgesia 2015 16(3):50-56.10.1080/22201173.2010.10872681 [Google Scholar] [CrossRef]