Dentine hypersensitivity (DH) is a common painful oral condition that can interfere with drinking, eating, tooth brushing and even breathing [1]. Cervical tooth surfaces are the common sites for hypersensitivity in approximately 90% of the patients [2]. The pain resulting from DH can compromise oral hygiene and quality of life in patients [3].
The prevalence of DH ranges from 4.5% to 57% and mostly found in individuals between 20 to 50 years of age, though it can occur at any age [4]. The condition affects a large number of people around the globe. Recent survey based studies have reported the prevalence of DH to be between 12.3% and 57% in America and Europe [5,6]. Scaramucci T et al., reported that the prevalence of DH was 46% in Brazilian population and females had significantly higher prevalence than males [7]. According to the studies from other countries such as India, China and UAE, prevalence of DH appeared to be 20.6% to 34.5% [8-11]. Large variations in the reported prevalence figures are possibly due to the differences in populations, dietary habits, oral hygiene practices and collection of data either using questionnaires or clinical examination [12,13]. Questionnaire studies might present overestimated results of the prevalence as DH is a highly subjective condition and most patients/subjects are more than likely to consider any form of dental pain or discomfort as sensitivity [14]. A recent study in Jordan found that 66.4% of subjects visiting teaching and public dental centers reported to have DH while only 28.7% of the samples were clinically diagnosed with the condition [15]. Taani SD et al., reported DH in 52.6% of adult patients, with female patients more often affected than male in Riyadh, Saudi Arabia [16].
Successful DH management depends on the identification and elimination of aetiological factors, careful clinical examination and differential diagnosis [4]. Although, several self-reported questionnaire and clinical examination studies have been performed in dental practices and university teaching hospitals [16-23]. However, limited data were available about dental students’ understanding of DH aetiology and management in Saudi Arabia. During undergraduate dental programs, students start diagnosing and treating patients under the supervision of faculty members. Therefore, it is expected that students should be equipped with knowledge and skills of different oral conditions before they can embark upon patients. DH is a prevalent condition; hence it is important that dental students should have adequate knowledge of DH, particularly during their clinical training years. Thus, the present study was conducted to assess dental students’ understanding of DH, its aetiology and management.
Materials and Methods
This cross-sectional study was conducted from February 2017 to April 2017. After obtaining ethical approval from the Scientific Research Unit at the College of Dentistry, a total of 218 questionnaires were distributed among undergraduate dental students providing treatment to patients at the Dental Hospital. The study sample was calculated assuming 5% margin of error, 95% confidence level, student population in the college (about 500), and 50% response distribution. These calculations revealed a sample of 218 participants. The power of study was 80% assuming type II error (β) of 20% and using a formula Power=1-β. Both male and female students (N=218) in 4th, 5th and 6th year of undergraduate Bachelor of Dental Surgery (BDS) program were approached. All students who agreed to participate in the survey were enrolled and consent was obtained. The students were provided with the information about the purpose and objective of the study and were encouraged to ask if they had any query about the questionnaire or study. The questionnaire was adapted from previous hypersensitivity studies involving dentists, dental students and/or interns [23-26]. This consisted of both pre-coded and open-ended questions relating to DH among patients visiting the hospital, its relationship to non-dental factors, frequency of patient questions, knowledge of the students, together with aetiological factors, available treatment options and need for an informational handout. The questionnaire was distributed among students in the beginning months of semester and they were asked to return it once completed. No reminder was given to those students who did not return the questionnaire.
Statistical Analysis
Descriptive statistics included percentages and frequencies of students’ responses in addition to data presentation in the form of graphs. Pearson’s chi-square test (Fisher-Exact test as appropriate) was performed to assess differences in male and female students’ response. SPSS (version 22 for Windows, SPSS Inc, USA) was used for statistical analysis. The p-value <0.05 was used for statistical significance.
Results
In this study, 165 of 218 students (99 males; 66 females) returned the completed questionnaires with a response rate of 75.7%. Demographic data of the study is presented in [Table/Fig-1]. The mean age of the study participants was 22±2 years. A vast majority of students (93.9%) treated 1-2 dentate patients per day. One quarter of the participants (24.8%) reported that they had seen one or more patients with DH seen in last 2-4 weeks.
Demographic information of the study participants.
| Variables | Frequency (N/%) |
|---|
| Gender |
| Male | 99 (60) |
| Female | 66 (40) |
| Class |
| Fourth year | 64 (38.8) |
| Fifth year | 59 (35.5) |
| Six year | 42 (25.5) |
| Treated 1-2 dentate patients in the clinic per day | 154 (93.9) |
| Patients with DH seen in last 2-4 weeks | 41 (24.8) |
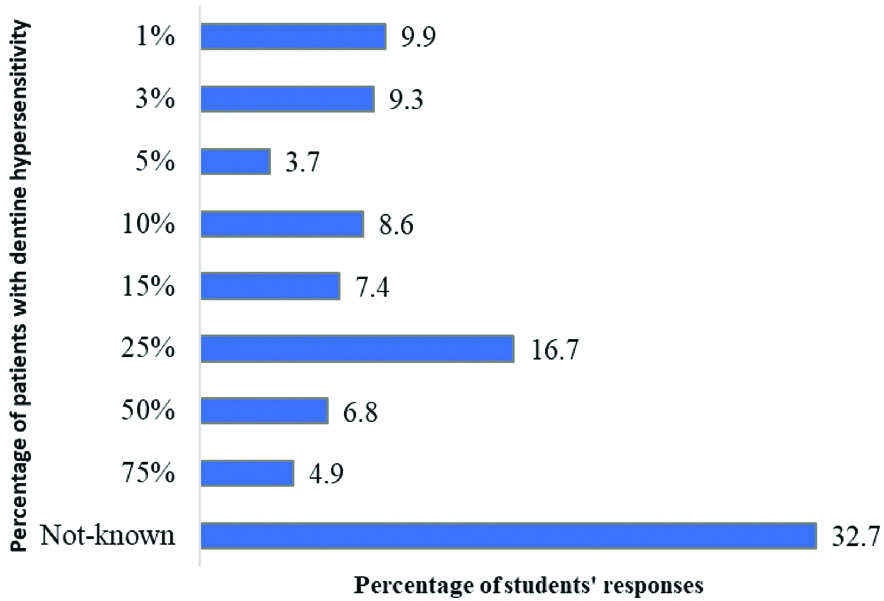
The students’ responses about the percentages of patients with DH seen in the clinic are shows in [Table/Fig-2]. In the study, 9.9% of respondents confirmed seeing 1% of patients DH, 16.7% of students had seen 25% of DH patients and 4.9% of students stated examining 75% of patients with DH [Table/Fig-2].
Dental students’ estimation of dentine hypersensitivity in their patients.
About half the respondents (53.9%) initiated conservation with patient about DH prior to diagnosis and 46.7% students observed the signs of DH during clinical examination. Twenty dental students (12.1) stated that 25% of patients with DH had severe problem and 10 students (6.1%) mentioned that 75% of patients with DH had severe problem. There were 9.7% of students who indicated that patients had complaints of DH for the last 4 week and ≥12 weeks whereas only 1.8% of students reported that the duration of DH complaint was ≤1 week. Majority of students (75.8%) considered that DH had a major impact on the quality of life of patients and 15.7% of respondents believed that this impact was severe [Table/Fig-3].
Students’ responses about DH.
| Variables | Frequency (N/%) |
|---|
| Conversation about DH |
| Yes | 89 (53.9) |
| No | 76 (46.1) |
| Signs of DH |
| Yes | 77 (46.7) |
| No | 88 (53.3) |
| Percentage of DH patients with severe problem |
| 0% | 17 (10.3) |
| 1% | 15 (9.1) |
| 3% | 7 (4.2) |
| 5% | 12 (7.3) |
| 10% | 12 (7.3) |
| 15% | 8 (4.8) |
| 25% | 20 (12.1) |
| 50% | 8 (4.8) |
| 75% | 10 (6.1) |
| Not known | 56 (33.9) |
| Duration of complaint of DH |
| ≤1 week | 3 (1.8) |
| 2 weeks | 12 (7.3) |
| 3 weeks | 3 (1.8) |
| 4 weeks | 16 (9.7) |
| 8 weeks | 10 (6.1) |
| ≥12 weeks | 16 (9.7) |
| Not known | 105 (63.3) |
| Impact of DH on quality of life |
| Yes | 125 (75.8) |
| No | 22 (13.3) |
| Don’t know | 18 (10.9) |
| Severity of impact of DH on quality life |
| Mild | 43 (26.1) |
| Moderate | 96 (58.2) |
| Severe | 26 (15.7) |
Majority of the participants (72%; n=119) reported that the aetiology of DH was unknown. However, only 8% (n=13) related it to the caries. About 66.6% (n=110) did not know about the steps to diagnose patients with DH and 30% (n=49) reported to use thermal tests for diagnosis. In response to a question about other dental conditions to be considered during diagnosis of DH, most of the participants (77%; n=127) provided a wide range of factors such as fractured restorations (77%), dental caries (75%), periodontal disease (68%) and cracked tooth syndrome (56%) etc., [Table/Fig-4]. Twenty two percent (n=36) were confident and 43.8% (n=70) were somewhat confident in correctly diagnosing the DH. There were only 60.6% (n=100) of the participants who replied to a question about currently accepted theory of DH (as this was an open-ended question) and of these only 39% (n=39) correctly identified hydrodynamic theory.
Dental students’ response: factors in the aetiology.
| Factors | No. of responses (%) |
|---|
| Fractured restoration | 127 (76.9) |
| Dental caries | 124 (75.15) |
| Periodontal disease | 112 (67.8) |
| Marginal leakage | 99 (60) |
| Bleaching sensitivity | 97 (58.8) |
| Cracked tooth syndrome | 92 (55.75) |
| Post restorative sensitivity | 91 (55.15) |
| Pulpitis | 87 (52.7) |
| Chipped teeth | 69 (41.8) |
| Palatogingival groove | 22 (13.3) |
Regarding diagnosing patients, only 26% (n=43) replied that they could diagnose patients with DH in clinics. Different proportion of students responded to a list of diagnostic tools that included medical history, dental examination, periodontal assessment, thermal tests, dental radiographs etc., [Table/Fig-5]. Further analysis showed significant differences between male and female students regarding some of the diagnostic tools (p≤0.05; [Table/Fig-5]). The respondents (59.3%) provided a wide range of treatment options/advice which included both at-home and in-office products [Table/Fig-6]. Replies of the participants indicated that most of them (69.7%; n=115) were confident in recommending appropriate at-home desensitising products. Thirty three percent of the participants believed that non-dental problems in daily life attributed to DH whereas 39% were unaware of any relation between the two. About 47.3% (n=78) of the respondents believed that their patients complied with the professional advice regarding management of DH. More than half (55.8%; n=92) agreed that there was a need to provide patients with an educational and preventive leaflet.
Assessment tools reported by the dental students.
| Assessment tools | Male | Female | p-value |
|---|
| Sensitivity reported by the patient (self-reported) | 12 (31.6) | 26 (68.4) | p>0.05 |
| Periodontal assessment (measurement of recession) | 8 (40) | 12 (60) | p>0.05 |
| Medical history | 3 (20) | 12 (18) | p≤0.05* |
| Thermal tests | 2 (15.4) | 11 (84.6) | p>0.05 |
| Dental examination | 11 (47.8) | 12 (52.2) | p>0.05 |
| Periodontal assessment (probing depths) | 5 (41.7) | 7 (58.3) | p>0.05 |
| Dental radiograph | 4 (40) | 6 (60) | p≤0.05* |
| Diet analysis | 2 (33.3) | 4 (66.7) | p>0.05 |
| Others | 11 (39.3) | 17 (60.7) | p>0.05 |
*Fisher-Exact Test
Dental students’ treatment advices/options to their patients.
| Treatment options | No. of responses (%) |
|---|
| At home use of desensitising dentifrice | 30 (18.2) |
| Education on proper tooth brushing techniques | 27 (16.3) |
| In-surgery application of a desensitising agent | 14 (8.5) |
| Restorative treatment | 27 (16.3) |
| Unknown | 67 (40.7) |
Discussion
High response rate in our study was because the students working in the College’s dental hospital were approached by the researchers and as soon as the questionnaires were filled, they were immediately returned. In contrast, previous questionnaire based studies about DH reported a low response rate (44.9 to 64.7%) of the participants [24-26] mainly because those involved general dental practitioners from different areas; in addition to the fact that the lack of knowledge and understanding of the subject might have prevented them to return the replies.
The results demonstrated that self-reported prevalence of DH (24.8%) was similar to the previous European (26.8%) and UK (25%) based studies [6,24] but higher compared to other studies [5,8]. However, it appeared similar to the reported low prevalence figures (8-34%) by some clinical studies [10,17,21,27,28] while others reported much higher prevalence figures of >40% [7,29]. A recent study of DH among students and dental interns found that 76.1% of respondents reported diagnosing patients with DH [23]. The above differences warrant the need to develop a standardised protocol for studies related to dentine hypersensitivity.
In the present study, survey included questions regarding the knowledge of aetiology of DH and its diagnosis. Majority of the students reported the aetiology to be unknown. More than half of the participants were not aware of the steps to diagnose a patient with DH, and approximately 34.2% were not even confident/somewhat confident to correctly diagnose the condition. This finding raises a concern that should be addressed by the educators. In another question related to the other dental conditions to be considered during diagnosis where students were provided with a number of options to choose from, they reported a wide range of factors such as fractured restorations, caries, periodontal disease, cracked tooth syndrome etc., Similarly, a previous study found the dental caries (82.7%), periodontal disease (74.5%), and fractured restoration (63.9%) were the three most common conditions used in the diagnosis of DH [23].
Previous literature had also reported the above-mentioned factors to be related to the DH [6,30,31]. For example, periodontal attachment loss during periodontal treatment could culminate in gingival recession and later to dentine hypersensitivity [6]. Addy M reported that dental caries, cracked tooth, broken restoration and microleakage could lead to hypersensitivity and pain [30]. Canadian Advisory Board on Dentin Hypersensitivity suggests considering dental caries, periodontal disease, fractured restoration, bleaching sensitivity, chipped teeth, and cracked tooth syndrome when diagnosing patients with DH [31].
Furthermore, Suge T et al., reported that hard toothbrush and improper brushing technique could lead to gingival recession and subsequently giving rise to pain [32]. In addition, abrasion, attrition, erosion and abfraction had also been reported to cause wearing of enamel and exposure of underlying dentine resulting in hypersensitivity [33]. However, in the present study, no student reported this as an aetiological factor for DH and most students were also unaware of any relation between non-dental problems and DH.
In the literature, three main theories have been described to explain the initiation and progression of pain during DH. These include direct innervation (neural) theory, odontoblast receptor theory and fluid movement or hydrodynamic theory with the last being the most widely accepted [34]. In the present study, only 39 respondents reported hydrodynamic theory as the currently accepted theory of DH. On the contrary, a study by Afolabi AO et al., reported that 56.8% (n=100) of study participants correctly identified hydrodynamic theory as the most common theory of tooth sensitivity [35].
From the results, it is evident that more than half of the participants reported that up to 25% of patients perceived DH to be a severe problem. The findings are similar to the previously reported severity of the condition with a low-grade pain in 23.7% of the participants [5]. In a previous study, Bekes K et al., reported low quality of life in patients with DH compared to healthy individuals from general population in Germany [3]. A recent study by Idon PI et al., found that patients with DH had significant impact on the oral health related quality of life in Nigeria [36]. In Malaysia, Masud M et al., analysed the data of patients with gingival recession and DH and found the both conditions physically and psychologically affected the quality of life of patients [37]. In the current survey, majority of the students considered that DH had moderate impact on the quality of life of their patients. Similarly, majority of respondents (64.7%) in a previous study reported that the impact of DH on quality of life was moderate, while 20% considered it mild and 15.3% as severe/extremely severe [23]. Goh V et al., showed that DH affected oral health related quality of life of patients receiving supportive periodontal care and the impact of quality of life was associated with the severity of DH [38]. Hence the proper knowledge of aetiology, diagnosis and treatment are important for the management of DH. Although most of the students claimed that their patients frequently asked questions about the condition, only 26% of the students responded to the question on how to diagnose patients with DH in clinics using multiple diagnostic tools. These were also the only students who were able to offer a wide range of treatment options for the management of DH to their patients, similar to those expressed by UK and Dutch practitioners [20,24,26]. The most popular responses in our sample included at-home use of desensitising toothpastes/gels followed by education on atraumatic tooth brushing techniques, restorative treatment and the professional application of desensitising agents. Similar responses were provided by dental students and intern in a previous study where education of proper toothbrushing technique, at home use of a desensitising dentifrice, and provision of restoration treatment were the most common DH management options [23].
It was evident from the participants’ responses that approximately half of the students believed that their patients complied with the professional advice regarding the management of DH which was relatively low compared to a previous UK study [24]. The UK study was based on the responses of a specific group of general dental practitioners working in private practices whereas the current study consisted of dental students based in a dental teaching hospital. Interestingly, dental practitioners had expressed similar desire in previous questionnaire based studies [24,26].
Limitation
The current study was limited to the undergraduate students of one dental college, hence warrants its generalisation.
Future Recommendation
Further multicenter studies are needed based on students from multiple dental colleges at national and international level.
Conclusion
Our results indicated that DH was highly prevalent condition in dental clinics. More than half of the participants considered DH as a severe problem and a majority believed that the impact of DH on the quality life of patients was moderate to severe. However, students lacked the knowledge and confidence to diagnose and manage DH.
*Fisher-Exact Test