Histopathological Analysis of Psoriasis in a Study of 24 Cases
Jagadish Gayathri1, Padma K Shetty2, Jayaprakash K Shetty3
1 Senior Resident, Department of Pathology, K.S.Hegde Medical Academy, Mangalore, Karnataka, India.
2 Professor, Department of Pathology, K.S.Hegde Medical Academy, Mangalore, Karnataka, India.
3 Professor and Head, Department of Pathology, K.S.Hegde Medical Academy, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Padma K Shetty, K.S.Hegde Medical Academy, Nithyananda Post, Deralakatte, Mangalore-575018, Karnataka, India.
E-mail: skpadmakshema@hotmail.com; drgayathri39@gmail.com
Introduction
As for any other organ system, diagnosis of skin disease involves history and examination. An instant diagnosis can be arrived upon by virtue of visibility of the skin taking into account various visual clues such as scaling, colouring, arrangement and the site of distribution of lesions. Although this appears effortless, the pattern of recognition is complicated while factoring in the individual components and analysing them separately.
Aim
To study the varying histopathological findings in cases of psoriasis.
Materials and Methods
Prospective study was conducted for two years. All patients who have been clinically diagnosed/suspected and untreated cases of psoriasis attending the Department of Dermatology were taken for the study. Wedge biopsy was taken under local anaesthesia.
Results
In the present study, the age group of patients ranged between 8-83 years with 17 of them being males and 07 of them being females. The ratio being 2.4:1 and the mean age was 43 years. The most common histopathological finding was elongated rete ridges, suprapapillary thinning and acanthosis within the epidermis. Munroe microabscess, hyperkeratosis and parakeratosis were the other findings noted within the epidermis. Within the dermis the most common finding was aggregates of lymphocytes which varied from mild to marked along with perivascular infiltration of lymphocytes.
Conclusion
Histopathological diagnosis forms the diagnostic tool for the dermatologists to arrive at a conclusion for their differential diagnosis since many skin disorders overlap with clinical presentations of psoriasis. This helps in excluding the differential diagnosis given by the clinician and to arrive at a definite histopathological diagnosis for the betterment of the patient.
Histopathological study, Macules, Papules, Plaques, Scales
Introduction
Skin diseases are not always visible, and there always forms a preconception amongst patients and other physicians that in order to make a diagnosis, inspection is sufficient [1]. The largest organ of our body the skin is extraordinarily vibrant with regard to the diversity and complexity of the protective functions it serves [2]. There are a heterogeneous group of papulosquamous disorders clinically characterised by scaly papules and plaques, with unknown aetiology. Owing to their overlapping clinical presentations leading to misdiagnosis dermatologists perform a biopsy to arrive at a clinical diagnosis [3]. Psoriasis is the most common papulosquamous condition affecting about 1.5-3% and further leading to significant morbidity [4]. The lesions in psoriasis is characterised by a homogenous glossy membrane with silvery white scales within a well defined margin [5]. Several conditions presenting with papules and scaly plaques mimic psoriasis and hence termed as psoriasiform dermatitis. The conditions include seborrheic dermatitis, pityriasis rubra pilaris, allergic dermatitis, atopic dermatitis, nummular dermatitis, lichen simplex chronicus, pityriasis rosea, dermatophytosis, and mycosis fungoides [6,7].
This study was conducted to identify the various histopathological findings in psoriasis since many of the clinical conditions mimic psoriasis as mentioned above and for the appropriate management of therapy to the patient, as well as to compare the clinical diagnosis with the histopathological diagnosis.
Materials and Methods
A prospective study of two years was conducted from September 2015 to September 2017 at a tertiary care centre in the Department of Pathology. The ethical clearance was obtained and the number is INST.EC/EC/055/2015-2016. All patients who have been clinically diagnosed/suspected and untreated cases of psoriasis attending the Department of Dermatology were considered. A consent was taken by the dermatologists before performing biopsy in suspected cases. A wedge biopsy was taken under local anaesthesia. The tissue was immediately fixed in 10% formalin and processed for 24 hours in the tissue processor. The sections were cut to a thickness of 2-3 microns. The sections are brought to water and stained with harris hematoxylin for 2-3 minutes and washed in a running water. Counter staining done with aqueous eosin for 2 minutes and then dehydrated with absolute alcohol which was further followed by mounting the slide for histopathological analysis. Inclusion criteria were the cases suspected with features of psoriasis that is patients presenting with white scales, papules and plaques attending dermatology department. The other conditions micking similar clinical findings included seborrheic dermatitis, pityriasis rubra pilaris, allergic dermatitis, atopic dermatitis, nummular dermatitis, lichen simplex chronicus, pityriasis rosea, dermatophytosis, and mycosis fungoides were also considered. Exclusion criteria were cases those who were Immunocompromised, with infective etiology, patients who have taken treatment for psoriasis, Pregnancy and lactation.
Results
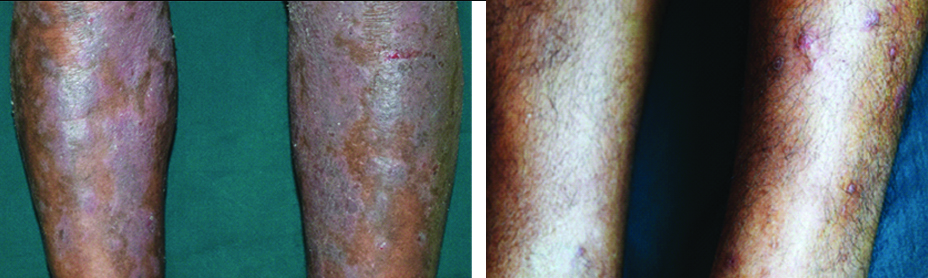
In a study span of two years, 24 cases were diagnosed histopathologically as Psoriasis amongst which 17 (70.83%) cases were found to be in males and 7 (29.2%.) cases were to be in females with a mean age of 43 years. The most common clinical presentation was found to be erythematous plaque in 62.5% cases which was followed by hyperpigmented plaque in 41.6% cases, papules in 25%, scales in 24% cases and macule in 1% [Table/Fig-1,2]. The most common diagnostic histopathological feature in the present study was acanthosis, suprapapillary thinning, elongated rete ridges and parakeratosis. The other epidermal changes noted in our study were hyperkeratosis, Munroe microabscess, spongiosis, Hypogranulosis, melanocytes in the basal layer [Table/Fig-3,4,5 and 6]. Mitotic figures and parafollicular keratin plugging followed by basal vacuolar degeneration and exocytosis in few cases. The predominant dermal changes noted in our study in cases of psoriasis is lymphocytic aggregates varying from moderate to dense, followed by blood vessels in the papillary dermis and perivascular infiltration of lymphocytes, Papillary oedema and Perivascular infiltration of neutrophils. The percent distribution of the above mentioned findings is enlisted in [Table/Fig-7].
Violaceous plaques, papules seen in a case of psoriasis.
A case of psoriasis showing hyperkeratosis, acanthosis, spongiosis (H&E stain; 10 x).

A case of psoriasis showing elongated rete ridges, acanthosis, spongiosis, hypogranulosis (H&E stain; 40x).

A case of psoriasis munroe microabscess, parakeratosis, blood vessels in the papillary dermis (H&E Stain; 40x).

In the epidermis munroe microabscess, parakeratosis, hyperkeratosis, suprapapillary thinning. Papillary dermis with blood vessels and lymphocytes infiltrating around the blood vessels (H&E stain 10x).

Histopathological findings in cases of psoriasis (n=24).
| Sl. No. | Epidermal changes | Number of cases | Percentage |
|---|
| 1. | Hyperkeratosis | 17 | 70.83% |
| 2. | Parakeratosis | 21 | 87.5% |
| 3. | Munroe microabscess | 14 | 58.33% |
| 4. | Suprapapillary thinning | 22 | 91.6% |
| 5. | Elongated rete ridges | 22 | 91.6% |
| 6. | Acanthosis | 22 | 91.6% |
| 7. | Spongiosis | 11 | 45.83% |
| 8. | Basal vacuolar degeneration | 1 | 4.16% |
| 9. | Exocytosis | 1 | 4.16% |
| 10. | Neutrophils forming pustules | 1 | 4.16% |
| 11. | Hypogranulosis | 4 | 16.7% |
| 12. | Melanophages | 3 | 12.5% |
| 13. | Mitotic figures | 2 | 8.3% |
| 14. | Perifollicular keratin plugging | 2 | 8.3% |
| Dermal changes |
| 1. | Lymphocytes | 24 | 100% |
| 2. | Papillary edema | 14 | 58.3% |
| 3. | Papillary dermis showing blood vessels | 19 | 79.2% |
| 4. | Perivascular infiltration of lymphocytes | 14 | 58.3% |
| 5. | Neutrophils | 4 | 16.6% |
| 6. | Eosinophils | 2 | 8.3% |
| 7. | Perivascular infiltration of neutrophils | 5 | 20.83% |
When a correlation was drawn between histopathological and clinical diagnosis given by the dermatologist, 19 (79.16%) patients the histopathological findings confirmed the clinical diagnosis while in 5 cases (15.15%) it differed from the clinical diagnosis. The prognostic findings could not be assessed since the exclusion criteria in our study was patients who were on treatment for psoriasis.
Discussion
An instant diagnosis can be arrived upon by virtue of visibility of the skin taking into account various visual clues such as scaling, colouring, arrangement and the site of distribution of lesions. Although this appears effortless, the pattern of recognition is complicated while factoring in the individual components and analysing them separately [8]. In the present study psoriasis was found more commonly in 41-50 years which was a consistent finding when compared with the study of Bell LM et al., [9]. Males were found most commonly affected, which was also found in the study of Younus M et al., [10]. A grading of histopathological findings of psoriasis on visual analogical scale was done by Moorchung N et al., [11] which included the parameters such as Hyperkeratosis which ranged from mild to marked, Presence or absence of Parakeratosis, Munroe microabscess, suprapillary thining, inflammatory infiltrate, capillary proliferation as in nil to marked. An association between various histopathological parameters was also done. In a similar manner in the current study the histopathological findings were graded in psoriatic patients and the results are as follows, 11 cases with mild hyperkeratosis, 4 with moderate and 2 cases with marked hyperkeratosis. Parakeratosis was present in 21 cases and munroe microabscess was present in 14 cases. Mild suprapapillary thinning was seen in 15 cases and moderate in 7 cases. Mild inflammation in 10 cases, moderate in 9 cases and marked in 5 cases. The association between different parameters was analysed by the likelihood ratio, and suprapapillary thinning carried a strong association with capillary dilation which was a consistent finding as seen in Moorchung N et al., [11]. Inflammatory infiltrate had a strong association with munroe microabscess which was not consistent with their study. Parakeratosis in our study had association with capillary dilation which was not favouring finding with their study.
Munroe microabscess was found to have a significant association with inflammatory infiltrate and capillary proliferation in our study which was a consistent finding. Capillary proliferation was found to have a strong association with suprapapillary thinning, parakeratosis and munroe microabscess which was not a consistent finding with Moorchung N et al., [11]. Thus from the above analysis we can note that capillary proliferation in the papillary dermis is most commonly found along with suprapapillary thinning, parakeratosis and munroe microabscess. In the present study, 84.8% histopathologically diagnosed cases of psoriasis was found concordant with the clinical diagnosis. When compared with other studies i.e., Reddy BR et al., and Chaudhary RG et al., [12,13]. Similarly the comparison of various histopathological findings found in our study with other studies was done which has been enlisted in [Table/Fig-8] [12,14-16]. Majority of the cases was concordant with their histopathological diagnosis, 94.11% and 74% respectively in their studies. The association between the various parameters presented in [Table/Fig-9].
Histopathological changes of psoriasis in comparison to other studies.
| Sl. No. | Epidermal changes | Chavan SD et al., [14] (2014) | Reddy BR et al., [12] (2014) | Kim BY et al., [15] (2015) | Karumbaiah KP et al., [16] (2017) | Present study (2017) |
|---|
| 1. | Hyperkeratosis | 25% | 82.5% | - | 77.2% | 70.83% |
| 2. | Parakeratosis | 15% | 79.5% | 90% | 72% | 87.5% |
| 3. | Munroe microabscess | 75% | 29.4% | 54% | 22.2% | 58.33% |
| 4. | Suprapapillary thinning | 4% | 38.23% | 90% | 40.9% | 91.6% |
| 5. | Elongated rete ridges | - | 73.5% | 93% | - | 91.6% |
| 6. | Acanthosis | 18% | 82.5% | - | 86.36% | 91.6% |
| 7. | Neutrophils forming pustules | 55% | - | 55% | 4.54% | 4.16% |
| 8. | Hypogranulosis | 50% | - | 96% | 22.27% | 16.7% |
| Dermal changes |
| 1. | Lymphocytes | 50% | 94.1% | 99% | 81.81% | 100% |
| 2. | Papillary dermis showing blood vessels | 10% | 88.2% | 93% | 86.36% | 79.2% |
| 3. | Papillary edema | 15% | 58.8% | 37% | 27.27% | 58.3% |
| 4. | Perivascular infiltration of lymphocytes | - | | 99% | - | 58.3%. |
Showing association between various histopathological parameters in psosriasis in our study.
| Parameters | Hyperkeratosis | Supra papillary thinning | Inflammatory infiltrate | Parakeratosis | Munroe Micro abscess | Capillary proliferation |
|---|
| Hyperkeratosis | 1 | 0.547 | 0.868 | 0.752 | 0.212 | 0.887 |
| Supra papillary thinning | 0.547 | 1 | 0.395 | 0.733 | 0.335 | 0.012 |
| Inflammatory infiltrate | 0.868 | 0.395 | 1 | 0.470 | 0.035 | 0.369 |
| Parakeratosis | 0.752 | 0.733 | 0.470 | 1 | 0.273 | 0.171 |
| Munroe microabscess | 0.885 | 0.335 | 0.035 | 0.273 | 1 | 0.027 |
| Capillary proliferation | 0.887 | 0.012 | 0.369 | 0.171 | 0.027 | 1 |
*likelihood ratio taken in our study
Limitation and Future Recommendation of The Study
The limitation found in our study was the less number of sample size diagnosed with psoriasis within a duration of two years. A still more strong association could have been obtained if the sample size was more. Also we obtained a few cases presenting with similar clinical findings as psoriasis but under histopathology not correlating with the features of psoriasis. Hence biopsy is highly recommended for the confirmation of diagnosis. This helps in appropriate management and for betterment of the patient.
Conclusion
Histopathological diagnosis forms the diagnostic tool for the dermatologists to arrive at a conclusion for their differential diagnosis since there are many disorders presenting with similar clinical features as psoriasis as mentioned earlier.
*likelihood ratio taken in our study
[1]. Griffiths Rooks textbook of dermatology 2016 9th edBlackwell publication:4.1 [Google Scholar]
[2]. Costa GD, Bharambe BM, Spectrum of non-infectious erythematous, Papular and squamous lesions of the skinIndian J Dermatol 2010 55:225-28.10.4103/0019-5154.7066621063511 [Google Scholar] [CrossRef] [PubMed]
[3]. Faraz A, Dharamshi HA, Zahir N, Saleem A, Ullah S, Role of skin biopsy in papulosquamous lesions-A comparative studyComp Clin Pathol 2015 24(5):2061-68.10.1007/s00580-015-2061-8 [Google Scholar] [CrossRef]
[4]. Krueger GG, Duvic M, Epidemiology of psoriasis. Clinical issuesJ Invest Dermatol 1994 102:14-18.10.1111/1523-1747.ep123860798006427 [Google Scholar] [CrossRef] [PubMed]
[5]. Camp RD, Rooks textbook of dermatology 1998 6th edOxfordBlackwell Publication [Google Scholar]
[6]. Altman E, Kamino H, Diagnosis Psoriasis or not. What are the cluesSemin Cutan Med Surg 1999 18:25-35.10.1016/S1085-5629(99)80005-4 [Google Scholar] [CrossRef]
[7]. Barr RJ, Young EM Jr, Psoriasiform and related papulosquamous disordersJ Cutan Pathol 1985 12:412-25.10.1111/j.1600-0560.1985.tb00439.x [Google Scholar] [CrossRef]
[8]. Rooks textbook of dermatology7th editionU:Blackwell:5.1-7.1. [Google Scholar]
[9]. Bell LM, Sedlack R, Beard CM, Perry HO, Michet CJ, Kurland LT, Incidence of Psoriasis in Rochester, Minn, 1980-1983Arch Dermatol 1991 127(8):1184-87.10.1001/archderm.1991.016800700840101863076 [Google Scholar] [CrossRef] [PubMed]
[10]. Younas M, ul Haque A, Spectrum of histopathological features in non infectious erythematous and papulosquamousInternational Journal of Pathology 2004 2(1):24-30. [Google Scholar]
[11]. Moorchung N, Khullar JS, Mani NS, Chatterjee M, Vasudevan B, Tripathi T, A study of various histopathological features and their relevance in pathogenesis of psoriasisIndian Journal of Dermatology 2013 58(4):294-98.10.4103/0019-5154.11394823919001 [Google Scholar] [CrossRef] [PubMed]
[12]. Reddy BR, Nalini KM, Histopathological spectrum of non-infectious erythematous, papulo-squamous lesionsAsian Pac. J Health Sci 2014 1(4S):28-34.10.21276/apjhs.2014.1.1s.6 [Google Scholar] [CrossRef]
[13]. Chaudhary RG, Chauhan AP, Makwana VR, Modi KR, Study of Clinico-histopathological correlation of papulosquamous disorders at tertiary care hospitalSch J App Med Sci 2015 3(3B):1154-58. [Google Scholar]
[14]. Chavhan SD, Mahajan SV, Vankudre AJ, A descriptive study on patients of papulosquamous lesion at tertiary care InstituteMVP Journal of Medical Sciences 2014 1(1):30-35.10.15306/mvpjms/2014/v1i1/46888 [Google Scholar] [CrossRef]
[15]. Kim BY, Choi JW, Kim BR, Youn SW, Histopathological findings are associated with the clinical types of psoriasis but not with the corresponding lesional psoriasis severity indexAnn Dermatol 2015 27(1):26-31.10.5021/ad.2015.27.1.2625673928 [Google Scholar] [CrossRef] [PubMed]
[16]. Karumbaiah KP, Anjum A, Mallikarjun M, A Histopathologic Study of Papulosquamous Lesions of SkinIndian Journal of Pathology Research and Practice 2017 6(2):404-09.10.21088/ijprp.2278.148X.62(pt-II)17.11 [Google Scholar] [CrossRef]