Materials and Methods
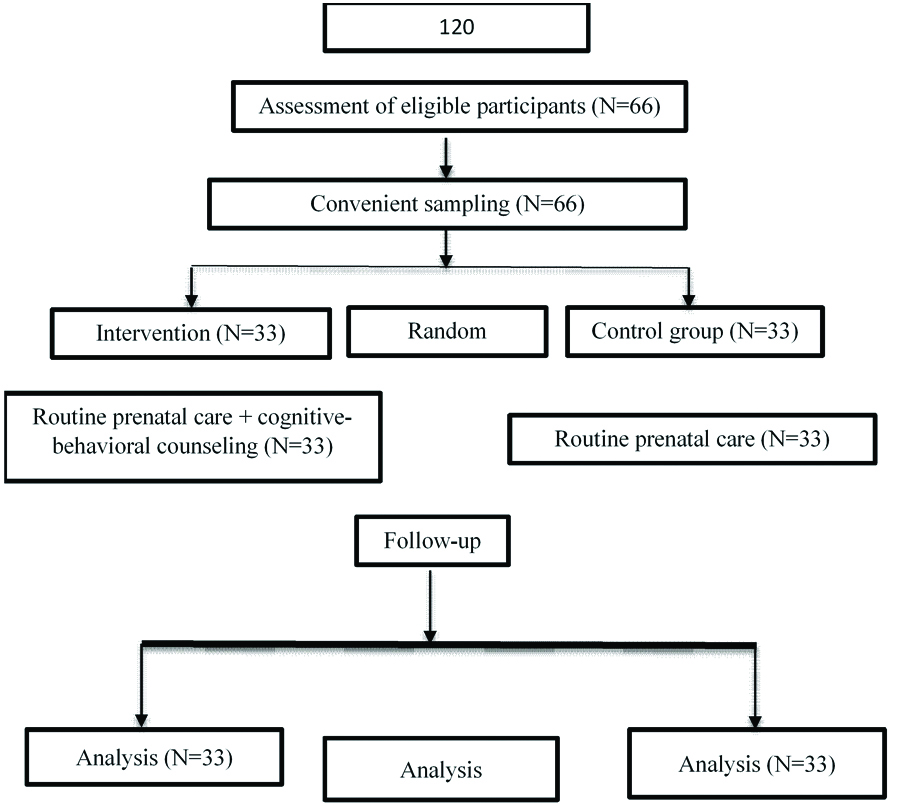
This randomised controlled clinical trial study was performed from February to June 2017, in health centres of Sanandaj, Iran. The sample size was chosen based on Hui AL et al., study [22] and based on the characteristic of gestational weight gain, therefore, using an 90% power and an alpha of 0.05. This required 33 participants in each group to achieve overall statistical significance. Sixty-six pregnant women who met the inclusion criteria were randomly assigned to intervention (n=33) and control (n=33) groups. In this study, simple randomization method was used for random allocation. The inclusion criteria for this study included age over 19, gestational age of 20-24 weeks, education level higher than primary school, wanted pregnancy, no disease or complications associated with pregnancy (pre-eclampsia, gestational diabetes, history of a child born with IUGR, etc.,), singleton pregnancy, no current mental illness, no known fetal disorder, no history of addiction, not using sedatives and not taking neurological drugs, having a BMI in the range of lean, normal, overweight and obese.
Exclusion criteria were abortion, labour or hospitalisation during the study period, and absence in ≥2 sessions. The research was done in the health centres in Sanandaj. Counselling sessions were held by the first author (student of Master’s degree in midwifery counselling) and under the supervision of the third author in coordination with members of the intervention group in one of Sanandaj health centres not visited by members of the control group. The control group received routine pregnancy services and care. In addition to routine care, the intervention group received 8 group counselling sessions of 60 to 90 minutes in groups of 11-12 participants with cognitive behavioural approach through discussion, question and answer, free connotation and education every other week. During these meetings, the focus was on cognitive restructuring, transformation and correction of distorted thoughts, and teaching cognitive-behavioural exercises and techniques. After participants were randomly assigned to the groups, they completed demographic characteristics questionnaire.
In this study, maternal weight gain per week was calculated with her BMI, so before the intervention, the mother was weighed and her BMI was calculated. Mothers’ weight was measured by the researcher using a calibrated Seca scale (made in Germany) and their height was measured by the height metre of the same scale without shoes. The measurements were performed twice, and then their mean was considered. Participants were weighed with light clothes and without shoes, and the weight in kilograms was divided by height in meters to determine their BMI. Women with BMI <18.5 were considered lean, those with 18.5≤BMI<24.9 normal, those with 25<BMI<29.9 overweight, and those with BMI ≥30 were considered obese.
To determine the standard weight range for each BMI category, the maximum recommended weight gain per week (0.5 kg/week for the lean group, 0.4 kg/week for the normal weight group, 0.3 kg/week for overweight group, 0.2 kg/week for obese group) [8] was multiplied in the number of weeks of intervention (12 weeks including, 8 weeks intervention and 4 weeks follow-up) so that the standard weighing for each subgroup was obtained for each BMI subgroup (For example standard weighing for the lean group was calculated this way: 0.5×12=6 kg and values above this was considered as over standard weighing and values below this was considered as below standard) [23]. Immediately and one month after the intervention, weight of both groups were measured again.
The content and structure of the sessions were as follows: in the first session participants were introduced and the program was described for them (establishing a therapeutic relationship). In the second session, entitled “Stress Management” the irrational thoughts and beliefs about stressors were evaluated and challenged and stress management techniques were taught. In the third session, entitled “Sports”, the irrational thoughts and beliefs about exercise during pregnancy were evaluated, challenged and discussed and suitable exercise for pregnancy was taught. In the fourth and fifth sessions, entitled “nutrition”, the irrational thoughts and beliefs about nutrition were evaluated, challenged and correct nutrition during pregnancy was taught. In the sixth session, entitled “sleep and rest”, their self-induced thoughts and cognitive disturbances (examining cognition deficits related to sleep and insomnia) were discussed. The seventh session, entitled “Gaining support and existence skills”, the irrational thoughts and beliefs about support and existence skills were evaluated (Distinguishing expectations from tasks). In the eighth session a summing up and summary of the lessons learned were held.
Participants were informed of the study objectives and were assured that they could leave the study at any time. Informed consent forms were obtained from all participants and they were assured that their information would remain confidential. Also, the study was conducted by the code IR.KUMS.REC.1395.763, confirmed by the Ethics Committee of Kermanshah University of Medical Sciences, Kermanshah, Iran, and registered in IRCT by the code IRCT2017041014333N72. All the details of selecting, excluding and analysis are given in CONSORT flow chart [Table/Fig-1].
Statistical Analysis
Independent t-test was used to compare weight gain scores before the intervention between two groups. The repeated measures were used to compare weight gain scores before, immediately after and one month after the intervention, in the intervention and control groups.
Mann-Whitney test was applied to compare BMI before, immediately after and one month after the intervention between two groups.
Results
The results of this study showed that before intervention, the groups were not significantly different in terms of educational level, place of residence, income level, number of pregnancies, mother’s occupational status, and BMI [Table/Fig-2]. Results showed that the intervention and control groups had a similar BMI before the intervention and there was no significant difference between the two groups (p=0.883). Also, independent t-test results showed that: There was no significant difference in mean weight of mothers before, Immediately and one month after the intervention, between two groups [Table/Fig-3]. To investigate BMI between intervention and control groups before intervention, chi-square test was used, the results of which showed that the intervention and the control groups had similar BMI before the intervention and there was no significant difference between the two groups (p=0.883) [Table/Fig-4].
Demographic characteristics of pregnant women.
| Variable | Intervention group N=33 | Control group N=33 | Test type |
|---|
| Mother’s age | 26.78±4.91 | 30.09±6.87 | Independent t test, p=0.028 |
| Gestational age | 22.18±1.44 | 20.69±1.13 | Mann Whitney, p=0.001 |
| Body mass index | 26.45±3.89 | 26.51±4.81 | Independent t test, p=0.963 |
| Mother’s educational level | Diploma and Under Diploma | 24 (72.7) | 27 (81.8) | Yates correction, p=0.387 |
| University | 9 (27.3) | 6 (18.2) |
| Mother’s employment status | Housewife | 30 (90.9) | 28 (84.8) | Exact fisher, p=0.354 |
| Employed | 3 (9.1) | 5 (15.2) |
| Income | Less than 10 million IRR | 20 (60.6) | 18 (54.5) | Yates correction, p=0.402 |
| More than 10 million IRR | 13 (39.4) | 15 (45.5) |
| Gravida | 1 | 23 (69.7) | 21 (63.6) | Yates correction, p=0.397 |
| ≥2 | 10 (30.3) | 12 (36.4) |
| Place of residence | Urban | 28 (84.8) | 26 (78.8) | Yates correction, p=0.375 |
| Rural | 5 (15.2) | 7 (21.2) |
| Husband’s education | Diploma and Under Diploma | 14 (42.4) | 19 (42.4) | Yates correction, p=0.162 |
| University | 19 (57.6) | 28 (84.8) |
| Husband’s job | Employed | 27 (81.8) | 28 (84.8) | Yates correction, p=0.162 |
| Others | 6 (18.2) | 5 (15.2) |
The pregnant women weight in the intervention and control groups before and after the intervention.
| Variable/Time | Before intervention | Immediately after intervention | One month after the intervention | Statistical index (p-value, Chi-square) |
|---|
| X±SD (Mean rank) | X±SD (Mean rank) | X±SD (Mean rank) |
|---|
| Weight | Intervention | 69.3±9.8 (33.18) | 74.2±9.47 (31.18) | 75±9.53 (30.73) | p-value=0.001 |
| Control | 68.7±11.58 (33.82) | 73.05±11.51 (35.82) | 75.03±11.35 (36.27) | p-value=0.001 |
| Statistical index | p-value=0.824 | p-value=0.905 | p-value=0.989 | |
The frequency of body mass index categories in pregnant women in the intervention and control groups before the intervention.
| Group | Body mass index | | Frequency | | Percent | |
|---|
| Before intervention | p-value | Immediately after intervention | p-value | One month after the intervention | p-value |
|---|
| Control | | Frequency | Percent | 0.946 | Frequency | Percent | 0.464 | Frequency | Percent | 0.948 |
| Lean | 1 | 3.1 | 0 | 0 | 0 | 0 |
| Obese | 3 | 9.1 | 9 | 27.3 | 12 | 36.4 |
| Overweight | 14 | 42.4 | 14 | 42.5 | 13 | 39.4 |
| Normal | 15 | 45.5 | 10 | 30.4 | 8 | 24.3 |
| Total | 33 | 100 | 33 | 100 | 33 | 100 |
| Intervention | Lean | 2 | 6.1 | 0 | 0 | 0 | 0 |
| Obese | 3 | 9.1 | 7 | 3/21 | 13 | 39.4 |
| Overweight | 13 | 39.4 | 19 | 6/57 | 13 | 39.4 |
| Normal | 15 | 45.5 | 7 | 3/21 | 7 | 21.3 |
| Total | 33 | 100 | 33 | 100 | 33 | 100 |
The standard weighing scale based on BMI in the intervention and control groups immediately after the intervention is shown in [Table/Fig-5] and one month after the intervention is shown in [Table/Fig-6]. According to [Table/Fig-5], the chi-square test showed that immediately after the intervention, the intervention and control groups were identical in terms of weight range and there was no significant difference between the two groups (p=0.278). Also, the results of the chi-square test showed that within one month after the intervention, the intervention and control groups were similar in terms of weight gain and there was no significant difference between the two groups (p=0.184).
Weight range based on body mass index in participants immediately after intervention.
| Group | Weight range | Frequency | Percent | Statistical index (z) | p-value |
|---|
| Control | Below standard | 5 | 15.2 | -1.084 | 0.278 |
| Standard | 8 | 24.2 |
| Higher than standard | 20 | 60.6 |
| Total | 33 | 100 |
| Intervention | Below standard | 6 | 18.2 |
| Standard | 12 | 36.4 |
| Higher than standard | 15 | 45.5 |
| Total | 33 | 100 |
Weight range based on BMI in participants one month after intervention.
| Group | Weight range | Frequency | Percent | Statistical index (z) | p-value |
|---|
| Control | Below standard | 5 | 15.2 | -1.084 | 0.278 |
| Standard | 8 | 24.2 |
| Higher than standard | 20 | 60.6 |
| Total | 33 | 100 |
| Intervention | Below standard | 6 | 18.2 |
| Standard | 12 | 36.4 |
| Higher than standard | 15 | 45.5 |
| Total | 33 | 100 |
Discussion
In this study, the effect of cognitive-behavioural counselling on weight gain of pregnant women was evaluated, and the results indicated no statistically significant difference between intervention and control groups immediately after the intervention and one month after intervention. However, in the intervention group, a higher number of women had a standard weight range after intervention. These results may be due to the small size of the studied population and limited sample size.
On the other hand, education of nutrition and physical activity, given to all pregnant mothers by health care providers and midwives of the health centres according to the Ministry of Health’s guidelines, have led to increased awareness of all pregnant women in the control group and this issue may have reduced the impact on intervention.
In the intervention group, 42.4% of the subjects and in the control group 69.7% weighed above the standard range. In the study of Althuizen E et al., four face-to-face counselling intervention, did not affect excessive weight gain during pregnancy [23]. Guelinckx I et al., stated that lifestyle intervention based on a brochure or on active education did not affect gestational weight gain in obese pregnant women [24]. According to Ronnberg A et al., the low-cost intervention programme did not reduce the percentage of women gaining weight above the Institute of Medicine recommendations (IMO) on gestational weight gain [25].
Contrary to the present results, some studies have shown that counselling have positive effects on weight gain of pregnant women during pregnancy [22,26,27]. Asbee SM et al., stated that a dietary and lifestyle counselling did reduce excessive weight gain during Pregnancy [21]. According to Gesell SB, “a community-based cognitive-behavioural lifestyle intervention during pregnancy was feasible in a hard-to-reach, high-risk population of low-income Latina women, and showed efficacy in preventing excessive gestational weight gain” [28]. Study of Hui AL et al., showed that “the lifestyle intervention program decreased gestational weight gain in pregnant women, with normal pre-pregnancy BMI but not above normal” [22]. According to Peaceman AM et al., behavioural lifestyle interventions focusing primarily on diet and physical activity among women with overweight and obesity resulted in a significantly lower proportion of women with excess gestational weight gain [29]. Although the present study and other studies mentioned above have been designed to encourage pregnant women to have weight gain within the IMO but they got different results which are possibly related to the response of the pregnant women to counselling. Also, the methodology of study can affect the results. In the Hui AL et al., study [22], a food choice map software which has been proved to be a valid tool for assessing dietary intake was used [30] and participants received a logbook on their exercise activities as a motivator for exercise and participants who attended less than three times at the group exercise or did not complete the logbook were excluded. In this study exercise intervention was a combination of exercise at home and group exercise.
Limitation
The study was limited to short-term follow-up, using a self-report tool and sample size, which may influence the generalisation of the results.
Conclusion
The results of the study indicated no effect of cognitive-behavioural counselling on weight gain of pregnant women. Therefore, it is suggested that studies should be done for weight gain of pregnent womens.