The shoulder joint is considered to be the most mobile joint in the human body. It is better referred to as the shoulder complex, as a number of articulations are necessary to place the humerus in space. The important joints are the glenohumeral, sternoclavicular, acromioclavicular joint and scapula thoracic articulations [1]. The shoulder complex acts in a coordinated manner to give the smoothest and greatest range of movement possible to the upper limb. The movement available to the Glenohumeral (GH) alone cannot account for the full elevation (abduction and flexion) of humerus. The rest of the range is supported by the scapula on the thorax through its sternoclavicular and acromioclavicular connection [2].
Frozen shoulder is a common shoulder problem between 40 to 60 years. It is reported to affect 2 to 5% of the general population [3], increasing to 10-38% in patients with diabetes and thyroid disease [4]. Women are more affected than the men with the involvement of the dominant side more [5].
It is an unknown aetiological condition characterised by a significant restriction of active and passive shoulder movement without any known intrinsic shoulder disorder [6]. This condition is characterised by thickening of the synovial capsule, contracted soft tissues and adhesion to the biceps tendon and/or obliteration of the axillary fold secondary to adhesion which results in an insidious and progressive loss of active and passive mobility in the GH joint due to joint contracture [7].
Scapulohumeral Rhythm (SHR) is defined as the movement relationship between the humerus and the scapula during both shoulder flexion and shoulder abduction. During shoulder abduction, there is 120 degrees of movement that occurs at the GH joint, while 60 degrees occurs at the scapulothoracic joint, creating a 2 to 1 ratio (2:1). This movement is known as the SHR of shoulder abduction. The same SHR occurs both during shoulder flexion and shoulder abduction [2]. However, the most important factors are the timing and coordination of the shoulder muscles and how they control the SHR. Alteration of this normal scapulohumeral movement pattern results in shoulder injuries, pain and impingement.
Reverse SHR makes the scapula move more than the humerus. The significance of the SHR is obvious with the frozen shoulder. The GH joint capsule adheres to itself in this condition and does not permit full movement. If this happens, the SHR will be very obviously disturbed. Any attempt at abduction usually requires significant substitution [8].
Multiple interventions for the treatment of frozen shoulder such as corticosteroid injections, surgery, patient education, cryotherapy, modalities (SWD, TENS, UST), moist heat, joint mobilisation, stretching, strengthening exercises have been described in order to restore function by reducing inflammation and pain and thus allowing the restoration of normal shoulder mechanics [9].
Joint mobilisation techniques improve normal shoulder capsule extensibility and stretch tight soft tissues thus reducing pain and increasing the range of movement and shoulder function. Scapula mobilisation can break adhesion and release muscles, thereby increasing scapular movements. Improving shoulder movement may also be linked to increased scapular movements [10].
Scapular mobilisation is recommended to regain normal extensibility of the shoulder, but there are only few studies [9-11] addressing the scapular mobilisation in the treatment of frozen shoulder. So the aim of the study was to evaluate the effectiveness of scapular mobilisation in the management of frozen shoulder.
Materials and Methods
The present study was a randomised controlled trial which was conducted in the outpatient Department of Physical Medicine and Rehabilitation (PMR), RMMC&H, Annamalai University, Tamil Nadu, India, during September, October and November 2018. The study was approved by the institutional Research Committee (PMR/DRC-5/2018).
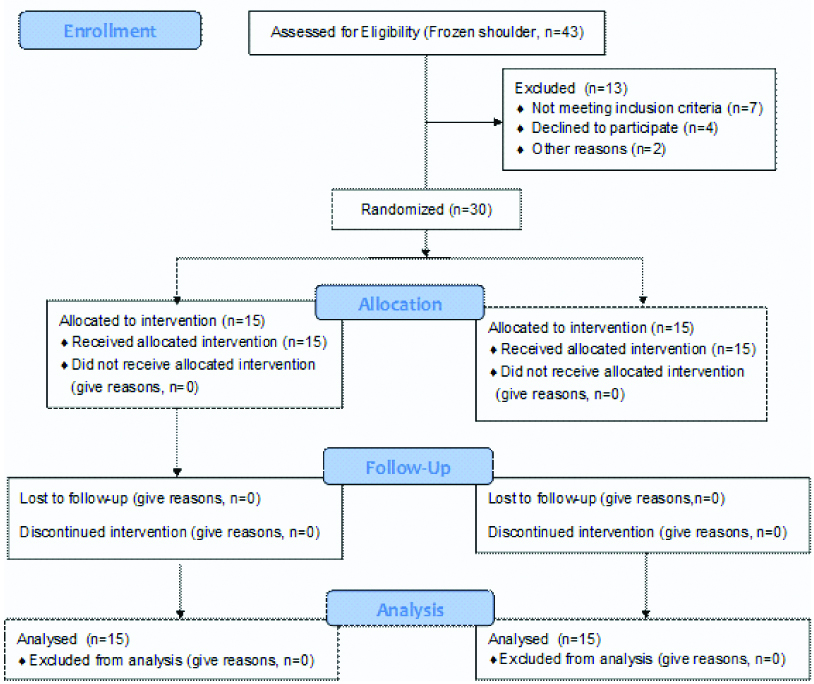
The sample size was selected by convenient sampling method during the stipulated period. Forty three patients with primary frozen shoulder aged 40 to 60 were selected, among them 13 patients were excluded and therefore the study sample was 30 patients. Consent was obtained from the patients.
The inclusion criteria for the study were: (1) duration of condition between 3 to12 months; (2) limited active and passive movement of the shoulder joint; (3) unilateral involvement; (4) both male and female; (5) absence of radiological evidence for GH joint arthritis; (6) capsular pattern of motion restrictions.
The exclusion criteria were: (1) local corticosteroid injection into the affected shoulder over the last three months; (2) previous shoulder surgery; (3) neurological disorders with muscle weakness in the shoulder joint.
Study Procedure
After screening for selection criteria, patients were informed about the purpose, study method and informed consent obtained for participation individually. Demographic data were collected. Subjects were randomly allocated into two groups i.e., odd number were in Group A and even number were in Group B [Table/Fig-1]. Group A (N=15) patients received wax therapy, capsular stretching, scapular mobilisation and home exercises. Group B (N=15) patients received wax therapy, capsular stretching and home exercises. Pre and post treatment score, primarily on pain intensity and shoulder ROM were measured by NPRS and universal goniometer respectively. Functional disability was assessed by the shoulder constant score [12,13] as secondary outcome measures. Pre and post treatment evaluation were compared and statistically analysed. Post assessment evaluation was done at the end of second week. The total duration of treatment was 10 days, frequency was one session/day, and the patient were allowed to continue their regular medication (analgesics) as prescribed by the physician.
CONSORT flow diagram of participants.
Outcome Measures
A. Primary Outcome Measures
1. NPRS: The NPRS is a reliable and effective pain measurement outcome. The straight line was drawn on the evaluation sheet with two end points ‘0’ and ‘10’ from left to right. The end marked with ‘0’ indicates no pain, while the other end marked with ‘10’ indicates severe pain. Patients were asked to mark a point on the line that corresponds to the amount of pain they perceived during the evaluation [14].
2. Shoulder ROM: A universal goniometry was used to measure the ROM in the plane of the scapula.
2.1 Shoulder abduction: Patient positioned in sitting with the humerus in adduction and external rotation. The axis were located in the acromion process of the shoulder. The stationary bar was parallel to the trunk and the movable bar was parallel to the humerus. The active ROM was recorded.
2.2 Shoulder External Rotation (ER): A patient sits with the humerus in abduction at 90°. The elbow bent at 90° and the forearm was pronated. The axis were located in the Olecranon process of the elbow. The stationary bar and movable bars were parallel to forearm. The active ROM was recorded.
B. Secondary Outcome Measures
Shoulder constant score: The constant score is a widely used shoulder-specific scoring system which is aimed exclusively at a numerical description of the quality of the shoulder function. From a perfect score of 100, it reserves 35 points for subjective evaluation reported by the patient, including pain and the ability to carry out basic activities of daily living and 65 points for objective measurement. For the latter, 40 points are allocated to ROM and 25 points are allocated to strength. The higher the score, the higher the quality of function [12,13].
Treatment Procedure
The treatment procedure were given for five days a week for two weeks. The total duration of treatment was 10 days, the frequency was one session/day [15]. Both groups received wax therapy (15 minutes) before joint mobilisation and the patients were taught home exercises at the end of the mobilisation.
Capsular stretching technique: Capsular stretching (Anterior capsule, Posterior capsule and Inferior capsule) was given for 5 repetitions, holding each stretch for 30 seconds [16,17].
Scapular mobilisation: Scapula mobilisation was given 2 sets of repetitions with a rest interval of 30 seconds between sets [9-11, 18-21].
Scapular superior glide: The patient lies on the unaffected side, the therapist places index finger of one hand under the medial scapular border of the affected side, the other hand grasps the superior border of the scapula. The scapula is superiorly moved for superior glide [Table/Fig-2].

Scapular inferior glide: The therapist makes the patient to lie comfortably on the unaffected side. Then the therapist places the index finger of one hand below the medial scapular border of the affected side and the other hand grasps the upper border of the scapula. The scapula is moved inferiorly [Table/Fig-3].

Capular upward rotation: The scapular upward rotation is done with the patient lying on the unaffected side, the therapist places the index finger of one hand under the medial border of the scapula and the other hand grasps the upper border of the scapula and rotates upwards [Table/Fig-4].
Scapular upward rotation.

Scapular downward rotation: The scapular downward rotation is carried out with the patient lying on the unaffected side, the therapist places index finger of one hand under the medial border of the scapula and the other hand grasps the superior border of the scapula and then rotates downwards [Table/Fig-5].
Scapular downward rotation.

Scapular distraction: The patient is in a side lying position, arm at side. Ulnar fingers below the medial scapular border and distracts the scapula from the thorax [Table/Fig-6].

Statistical Analysis
Statistical analyses of the study were conducted using the “Statistical Package for Social Sciences” (SPSS) Version 21. To analyse the pre and post treatment NPRS score, non parametric test (Wilcoxon signed rank test) was selected as the variable is discrete. To analyse NPRS between groups the non parametric (Mann-Whitney ‘u’ test) was selected. To analyse other outcome measures in the same group, parametric tests were selected and analysed by paired sample t-test and between group comparison was measured by Independent sample t-test. The level of significance was set at α= 0.05. The data was presented in tabular form.
Results
The mean age of the study population was 51.73 years with the corresponding standard deviation of 7.70 in Group A, while for group B it was 51.40 (7.37) years. The other baseline characters of group A and group B is shown in [Table/Fig-7].
Baseline characteristics of the group A and group B.
| Characteristics | Group A | Group B | p-value |
|---|
| Age (years) | 51.73 (Mean) | 7.70 (SD) | 51.40 (Mean) | 7.37 (SD) | 0.10 |
| Sex | n | % | n | % | 0.13 |
| Male | 8 | 53.3 | 11 | 73.3 |
| Female | 7 | 46.7 | 4 | 26.7 |
| Side of Involvement | n | % | n | % | 0.12 |
| Right | 9 | 60 | 8 | 53.3 |
| Left | 6 | 40 | 7 | 46.7 |
| Duration of ailment, months | n | % | n | % | 0.15 |
| 3-6 | 7 | 46.7 | 2 | 13.3 |
| 6-9 | 4 | 26.7 | 6 | 40.0 |
| >9 | 4 | 26.7 | 7 | 46.7 |
n: Number; SD: Standard deviation; %: Percentage
There was a significant difference in the NPRS after treatment in both the groups. The degree of improvement was significantly higher in group A (M=4.07±1.03) than in group B (M=1.87±0.64). Therefore, treatment A was significantly better than treatment B in reducing pain of the frozen shoulder [Table/Fig-8].
| NPRS | Group A | Group B | Pre post difference |
|---|
| Pre | Post | Pre | Post | A | B |
|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
|---|
| 8.00 | 0.75 | 3.93 | 0.88 | 6.67 | 1.17 | 4.80 | 1.32 | 4.07 | 1.03 | 1.87 | 0.64 |
| Z | 3.44 | 3.50 | 4.39 |
| p | 0.001 | 0.001 | 0.001 |
Z: Mann-Whitney U test statistics; M=Mean
Active shoulder abduction ROM significantly improved after treatment in both the groups. The magnitude of improvement was significantly higher in group A (45±17.22) than in group B (20±8.02) [Table/Fig-9].
Active shoulder abduction, external rotation ROM and constant score comparison.
| Measurement | A | B | Pre post difference |
|---|
| Pre | Post | Z | p-value | Pre | Post | Z | p-value | A | B | Z | p-value |
|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
|---|
| Active shoulder abduction | 100.33 | 12.31 | 145.33 | 15.98 | 3.42 | 0.001 | 99.67 | 15.86 | 119.67 | 16.85 | 3.44 | 0.001 | 45.00 | 17.22 | 20.00 | 8.02 | 3.51 | 0.001 |
| Active external rotation | 43 | 13.20 | 71.67 | 12.19 | 3.42 | 0.001 | 50.33 | 12.31 | 63.33 | 10.96 | 3.34 | 0.001 | 28.67 | 9.54 | 13.00 | 6.21 | 4.08 | 0.001 |
| Constant score | 48.69 | 9.38 | 78.13 | 5.99 | 17.69 | 0.001 | 48.81 | 10.18 | 67.16 | 9.97 | 15.13 | 0.001 | 29.44 | 6.44 | 18.35 | 4.69 | 5.39 | 0.001 |
There was significant improvement in shoulder external rotation ROM following treatment in both the groups. In comparison group A had significantly higher improvement (M=28.67±9.54) than in group B (M=13.00±6.21) and p=0.001.
The constant score significantly improved following treatment in both the groups. The degree of improvement was again significantly higher in group A (M=29.44±6.44) than in group B (M=18.35±4.69).
Discussion
Scapular mobilisation was found to be comparatively better than conventional treatment in pain improvement, increased shoulder abduction and external rotation ROM and constant scores. The result of this study is in accordance with the study of Kumar M et al., scapular mobilisation was carried out according to Maitland mobilizatation in that study [9]. It produces the effects of tissue stretching and also leads to the rearrangement of connective tissue, extracellular matrix and collagen tissues, so that tissue remodelling can increase tensile loading.
Biomechanically [2] the coracohumeral ligament is supposed to limit external rotation ROM. The rotator interval and the superior GH ligament, which have greater resistance to external rotation, are other potential factors limiting external rotation. Shoulder abduction is restricted by inferior capsule. The internal rotation loss pattern is consistent with capsular tightness in the posterior band of the inferior GH ligament complex, which limits internal rotation ROM.
The chronic frozen shoulder is characterised by an adherent axillary recess, coracohumeral ligament thickness, adhesion formation in the rotator intervals and contracted soft tissues can lead to the kinematic alteration of the scapulohumeral and scapulothoracic joint. This results in restricted capsular pattern i.e. external rotation and abduction were more restricted, and internal rotation and flexion were less restricted [8]. The scapulothoracic joint consists of muscles and not synovial joints. Scapular mobilisation can break adhesions and release these muscles, thereby increasing scapular movement. The improved movement of the shoulder could also be linked to increased scapular movement. The effects of joint mobilisation include elimination of capsular restrictions and adhesive breakage, tissue distraction and normal movement, and articular cartilage lubrication.
GH and scapulothoracic joints are recognised in the closed kinetic chain. We assume that GH joint mobilisation improves shoulder movement and normalises the SHR. Scapular mobilisation should improve shoulder movements, improving the functional status of the shoulder if scapular and shoulder movements are improved [10].
Joint mobilisation techniques also have neurophysiological effects based on peripheral mechanoreceptor stimulation and nociceptor inhibition, according to Surenkok O et al., [11]. These mechanoreceptors are mostly present around the synovial joints. Scapular mobilisation can be linked to the muscle structures instead of the synovial joint, which is rich in mechanoreceptors. In the present study, after scapular mobilisation, NPRS scores improved. We therefore suggest that scapular mobilisation can be linked to muscle structures instead of the synovial joint, which is rich in mechanoreceptors.
The outcome of this study is consistent with the previous study of Wells PE et al., [22], who stated that Scapular mobilisation consisted of the application of superior and inferior gliding, rotation and distraction to the scapula. The patterns were chosen because of decreases in the abnormal biomechanics of scapular upward rotation, superior tilt, posterior tilt and external rotation.
In this present study, shoulder functional disability was evaluated with the shoulder constant score. This includes pain, shoulder ROM, shoulder function and strength. The current study showed that the functional status of the shoulder improves when scapular and shoulder movements are improved. Lin JJ et al., found that scapular kinematics in patients with shoulder dysfunction would be important to reflect functional disabilities [23]. Our findings are particularly notable because scapular mobilisation can help reduce functional disabilities in patients with frozen shoulder.
Joint mobilisation is one of the effective interventions for treating frozen shoulder. So many studies have given great importance to the mobilisation of GH joint. However, only limited literature supported for scapular mobilisation. Scapular mobilisation can break adhesions and release these muscles and thus increase scapular motion, which reduces pain, increases ROM and shoulder function.
Limitation
The studied sample size is considerably small. To further validate this innovative therapeutic technique for frozen shoulder, it may be necessary to increase the number of participants.
Conclusion
The result of the study concludes that both treatment approches are effective in reducing pain, improving ROM, and functional disability in patients with frozen shoulder. However, the patients who received the scapular mobilisation had significantly higher improvement than the control group.
n: Number; SD: Standard deviation; %: Percentage
Z: Mann-Whitney U test statistics; M=Mean