Foreign body ingestion is frequently encountered in infants and young children. In recent years, button batteries have become extremely common among household use. As a result of this, there has been an increase in the outcomes related to this button batteries ingestion. Literature reports that there has been a 6.7 fold increase in the major or fatal outcomes associated with button battery ingestion. The complications are attributed to the electric current generated at the negative pole of the battery and the discharge of alkaline electrolytes, leading to liquefaction necrosis and also due to pressure necrosis. Here, authors’ report with two cases of button battery ingestion, of which one case had a fatal outcome and about the measures taken in the second case to avoid major or fatal consequences.
Aorto-oesophageal fistula, Bleeding, Foreign body, Oesophageal burns
Case Report
Case 1
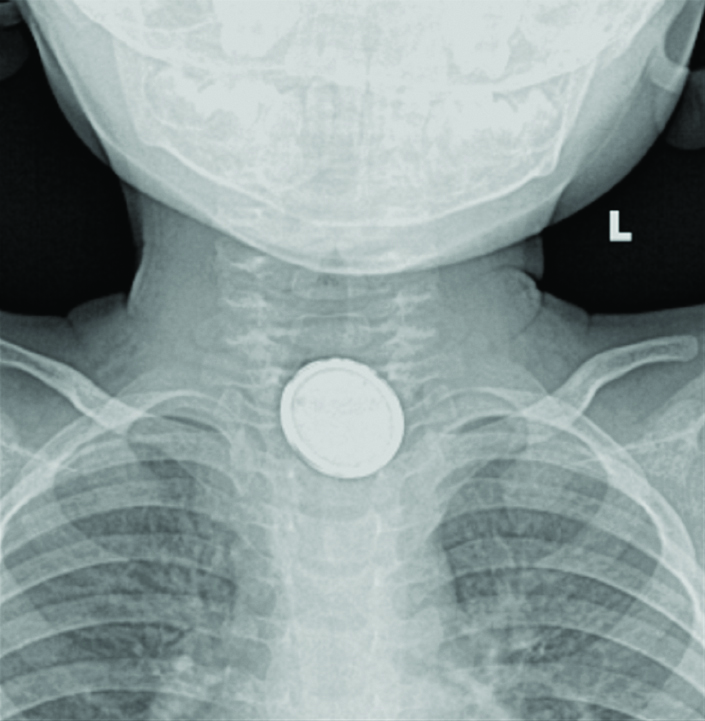
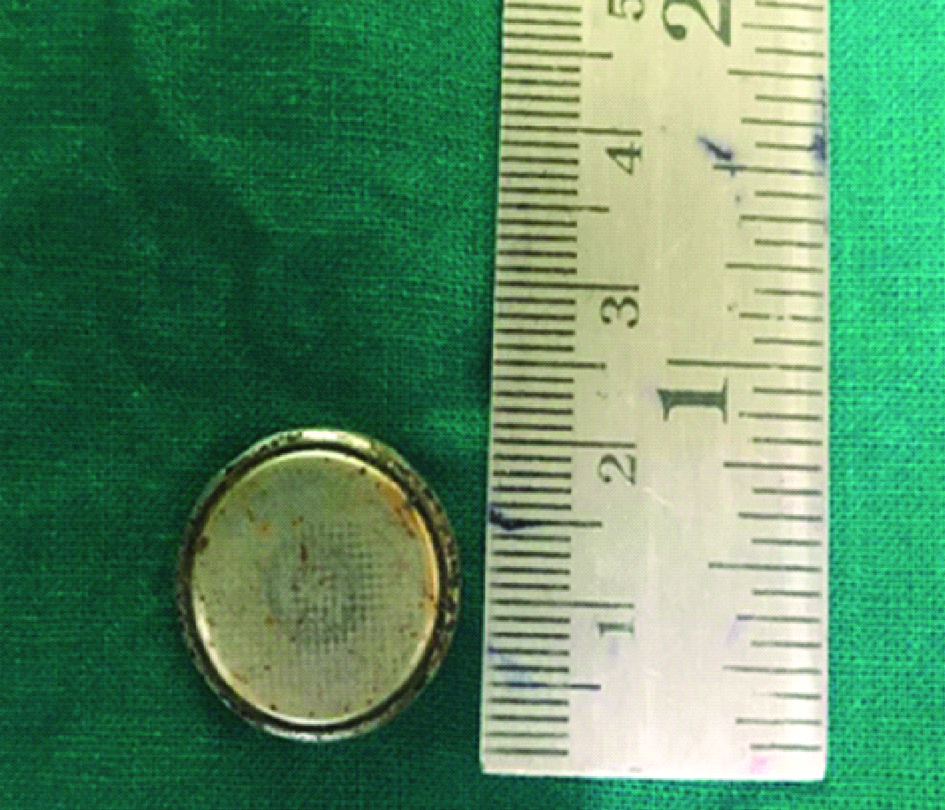
A one-year-old child presented to the emergency outpatient department with reduced appetite, foul-smelling vomitus and alleged history of ingestion of a button battery from a television remote ten days before the hospital visit. ENT examination was normal. Radiography of the neck-anteroposterior view revealed a radio-opaque foreign body with double rim appearance in the cricopharynx with surrounding soft tissue oedema [Table/Fig-1]. The child was immediately taken up for emergency rigid hypopharyngoscopy and foreign body removal under general anaesthesia within two hours of presentation to the hospital. Intraoperatively, a 20 mm, 3V Lithium button battery was identified at the level of the cricopharynx, 16 cm from the upper incisor, covered with slough [Table/Fig-2]. On removal of the foreign body, there was mucosal erosion with no evidence of perforation or bleeding. A nasogastric tube was inserted intra-operatively in view of the mucosal erosion. Immediate to post-operative period the child was kept nil per oral. Nasogastric tube aspirate showed brownish blood stained content, which turned clear in two days. The child was transferred to the Paediatric Intensive Care Unit for observation. On post-operative Day 3, the child developed an episode of seizure associated with minor bleeding from the nose and mouth. Blood investigations revealed hyponatremia and hypocalcaemia. The seizures were attributed to the same and were corrected, and the child showed clinical improvement without further episodes of seizures or bleeding. The child was asymptomatic and hence was started on oral feeds on post-operative Day 6. Child tolerated the oral feeds well. On post-operative Day 8, the child developed an episode of generalised tonic-clonic seizures associated with massive haematemesis, haematochezia and epistaxis leading to hypovolemic shock and cardiac arrest. Spontaneous circulation was achieved with cardiopulmonary resuscitation. However, the child continued to have persistent massive bleeding from the oral cavity, nose and rectum with abdominal distension. An Aorto-oesophageal fistula was suspected. Before intervention for the same, the child succumbed due to massive bleeding.
The radiographic AP view of neck showing the double rim pattern.
The 20 mm Lithium button battery that was removed from the cricopharynx, showing the erosions.
Case 2
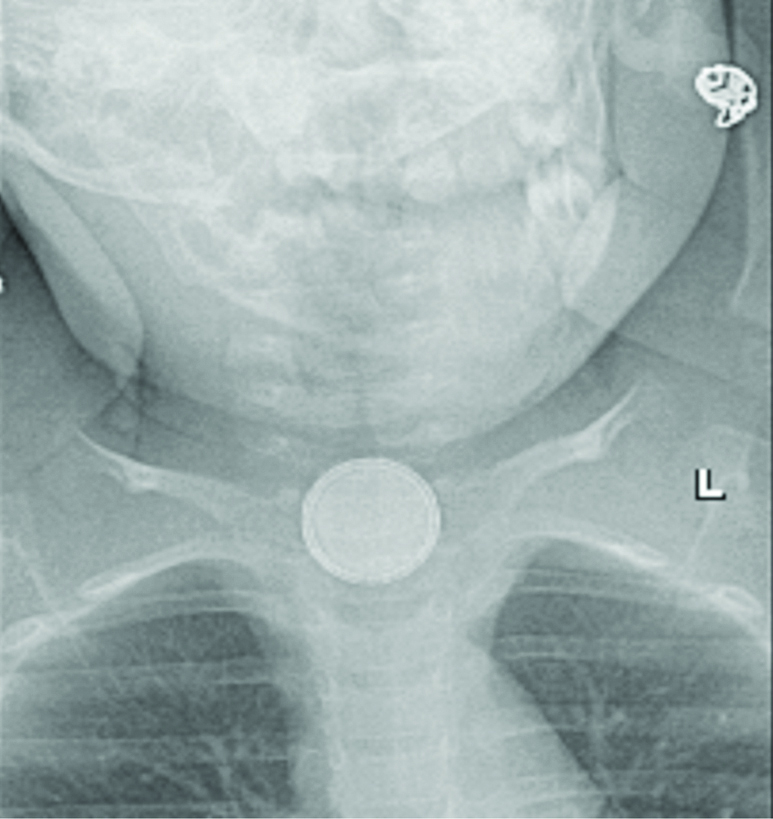
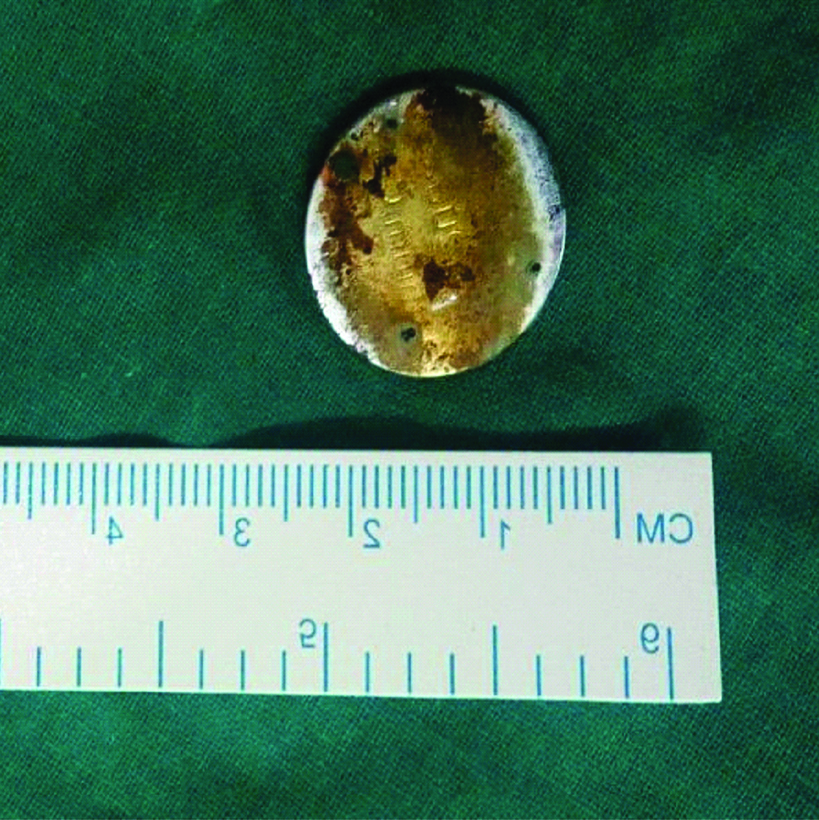
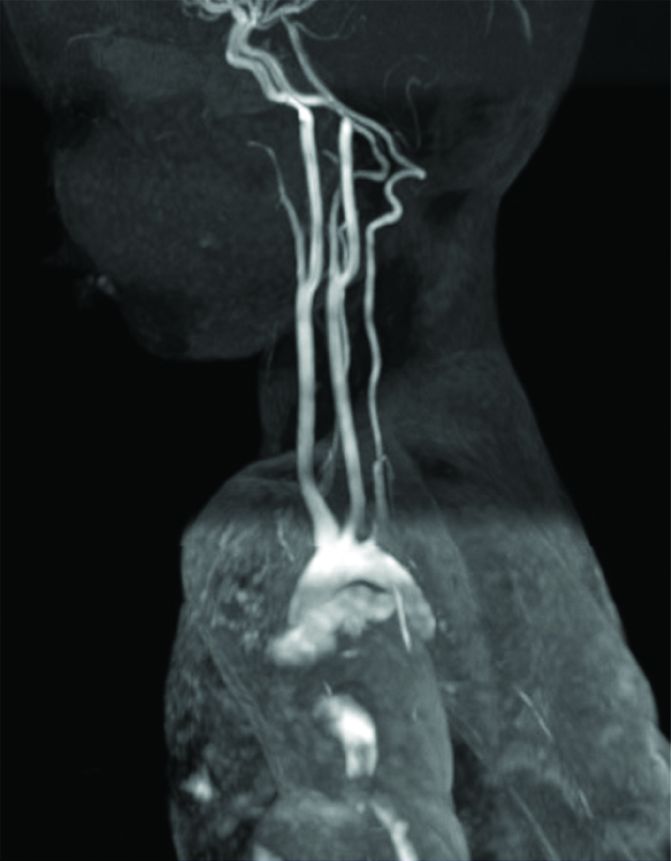
A one-year-old child presented with complaints of two episodes of blood-stained vomitus following ingestion of a button battery from a toy, nine hours before presenting to the hospital. ENT examination was normal. A radiograph of the neck-anteroposterior view revealed a circular radio-opaque foreign body with a double rim appearance, suggestive of a button battery at the level of C3-C4 [Table/Fig-3]. The child was immediately taken up for emergency rigid hypopharyngoscopy and foreign body removal under general anaesthesia within 2 hours of admission to the hospital. Intraoperatively a 20 mm, 3V lithium button battery was removed from the cricopharynx, 15 cm from the upper incisor [Table/Fig-4]. Underlying mucosa showed erosion and blackish discolouration. A nasogastric tube was inserted. The child was transferred to the Paediatric intensive care unit post-operatively. Nasogastric tube aspirate was suggestive of bile-stained fluid only. The child was continued NPO and nil per nasogastric tube post-operatively for eight days. The child was hemodynamically stable. On post-operative Day 8, an MRA of the Head and neck was done to rule out any fistulas between the oesophagus and the great vessels of the neck [Table/Fig-5]. Nasogastric tube feeds were started on Post-operative Day 9. A Gastrograffin study was done on post-operative Day 18 to rule out any oesophageal fistulas or perforations, which were normal [Table/Fig-6]. Hence, child was gradually started on oral feeds on post-operative Day 19 under observation in the intensive care unit. Child tolerated the oral feeds well. Feeds were slowly switched over from liquids to semisolids and then to solids. The child was asymptomatic and taking adequate oral feeds and hence was discharged and advised close follow-up.
The radiography neck anteroposterior view showing the double rim appearace.
The 20 mm Lithium battery that was removed from the cricopharynx.
MR Angiogram showing no evidence of fistula formation with the great vessels of the neck.
Gastrograffin swallow showing no evidence of perforation or stricture.

Discussion
Foreign body ingestion is commonly encountered in infants and young children. Button batteries are circular in shape with a diameter ranging from 7 mm to 20 mm. They are usually made of Lithium, Manganese dioxide, Mercuric oxide, Silver oxide or Zinc. In recent years, button batteries have become extremely common among household use. Accidental ingestion of button batteries is commonly seen in children. As a result of this, there has been an increase in both the minor and major or fatal outcomes related to these button battery ingestion. Literature reports that there has been a 6.7 fold increase in the major or fatal outcomes associated with button battery ingestion (0.066% in 1985-1987 vs. 0.443% in 2007-2009) [1]. The complications are attributed to the electric current produced at the negative pole of the battery and the release of alkaline electrolytes, causing liquefaction necrosis and also due to pressure necrosis [2]. This is a report of two cases of Button battery ingestion, of which one case had a fatal outcome. The second case reports about the measures taken to avoid major or fatal consequences.
National Battery ingestion Hotline data analysis suggests that button battery ingestion is common among children less than six years of age and the source of the batteries are remote controls, toys, watches, alarm clocks, flameless candles [1]. It also shows that there is an increase in the incidence of ingestion of batteries more than 20 mm, especially lithium batteries. The batteries are frequently impacted in the oesophagus in younger children due to the smaller diameter of the oesophagus, especially when the size of the battery is more than 20 mm [3]. These battery ingestions are usually unwitnessed with non-specific symptoms like dysphagia, food refusal, drooling, acute airway obstruction, vomiting, irritability, fever, rashes, abdominal pain, haematemesis and respiratory distress [2,3]. These non-specific symptoms lead to the delay in the diagnosis and the management of these cases [4]. Any battery lodged in the oesophagus can cause burns within 2-2.5 hours of ingestion [2]. Hence, removal within 2 hours can provide injury free removal. This becomes challenging when it comes to the non-verbal paediatric age group. Hence any child with suspected battery ingestion, a radiograph of the neck, chest and abdomen to locate the position of the battery is recommended [1]. The classical “double rim appearance” is seen in the anteroposterior view and a “step off” appearance on the lateral view [2]. Even in cases of coin ingestion, these features have to be looked for to rule out the battery ingestion which has been mistaken for a coin.
A Battery lodged in the oesophagus can erode into the aorta, trachea, lung or mediastinum. The four mechanisms by which injury occurs in button battery ingestion are: 1) Mucosal burn due to the electric current flowing between the positive and negative pole of the battery; 2) Caustic injury due to the leakage of the alkaline contents of the battery; 3) Direct pressure over the mucosa causes compromise in the blood supply and ischaemia leading to pressure necrosis- resulting in fistula and stricture formation; 4) The absorption of the toxic substances leading to systemic heavy metal poisoning especially with mercury and not very common with other metals. It is the negative pole of the battery that releases electrolytic currents that hydrolyse the tissues to produce subsequent effects [1,5]. Hence having an idea about the position of the negative pole of the battery helps to anticipate the subsequent injuries that can occur [6]. This is identified by the narrower negative pole in the lateral view radiograph.
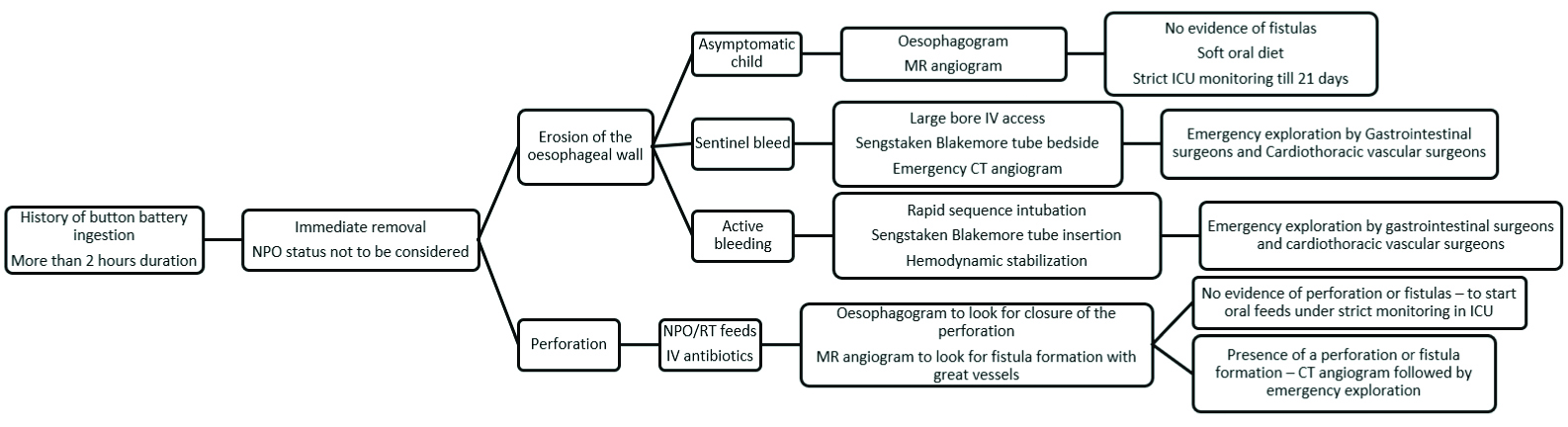
The oesophagus is most at risk as it has weak peristalsis and there are three areas of narrowing at the cricopharyngeal sphincter, where the oesophagus is crossed by the aortic arch and the lower oesophageal sphincter. The recommendation as per the North American Society for Paediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) Endoscopy Committee, for the removal of oesophageal button batteries are within two hours of ingestion [7]. In this crucial period between the time of ingestion and removal of the battery, it has been demonstrated that the use of honey at home and sucralfate in a hospital setting have protective effects both in-vitro and in-vivo, by reducing the hydroxide generation thus neutralising the tissue pH and creating more localised and superficial injuries and decreasing the severity of the outcome [8]. The recommended dosage of honey is 2 teaspoons/10 mL of honey every 10 minutes up to 6 doses [8]. This, however, is not a substitute for delaying the removal of the foreign body. Though numerous blind techniques have been described for removal of oesophageal foreign bodies, rigid oesophagoscopy should be performed to remove button batteries to assess the extent of erosion in the oesophagus at the time of removal, to plan further management. Rigid oesophagoscopy is performed under General Anaesthesia, with muscle relaxants. The scope is passed through the oral cavity, the cricopharynx and into the oesophagus to remove the foreign body. After removal of the foreign body, a check scopy is performed to reassess the site of impaction. The significant time lapse between the ingestion and removal of the foreign body requires proper counselling of the parents regarding the grievous complications that are associated with the condition. Even after removal of the foreign body, the residual alkaline substances present at the site of impaction continue to produce burns. A number of cases of aorto-oesophageal fistula due to button battery ingestion which resulted in exsanguination have been reported in literature. Some of the other major consequences reported in literature following button battery ingestion include oesophagitis, oesophageal perforation, trachea-oesophageal fistula, fistulization into the major vessels leading to catastrophic bleeding, oesophageal stricture, tracheal stenosis, spondylodiscitis, vocal cord palsy, mediastinitis [9-11]. These complications can be anticipated in cases where the battery ingested is more than 20 mm, the child is less than four years of age, ingestion of multiple batteries, unwitnessed ingestions, misdiagnosed cases and delay in the removal of the foreign body [10]. The most common lesion associated with fatal haemorrhage is a battery induced aorto-oesophageal fistula [12]. An aorto-oesophageal fistula has been reported to occur 18 days after removal. Chiari’s triad has described a classical presentation of an aorto-oesophageal fistula as mid-thoracic pain, sentinel arterial haemorrhage and exsanguination after a symptom-free interval [2]. Thus, the chances of developing complications persist up to 18 days after removal of the battery, mandating observation in the intensive care unit. During this period, the child should be strictly kept Nil per Oral with total parenteral nutrition and continuous aspiration of the gastric contents through the nasogastric tube. Any signs of minor bleeding (sentinel bleeding) should be looked for as they are signs of impending catastrophic haemorrhage. Brumbaugh DE et al., suggest that a Sengstaken Blakemore tube would be helpful in cases of active bleed and sentinel bleeds [12]. It can be used to provide a tamponade effect, with a much higher pressure than usual as it is an arterial bleed. However, this should be used only to reduce the bleeding in the transit time to the operating room and also the chances of pressure necrosis with such high tamponade pressure should be borne in mind. So far the best imaging modality to identify such fistulas is an MR angiogram, though it is not the gold standard. A Computed Tomography (CT) angiogram is not useful unless there is active bleeding [12]. An endoscopy can, however, reveal the presence of non-healing ulceration, active bleeding, or pulsatile area. A multidisciplinary team including an Otolaryngologist, Gastroenterologist, Paediatric surgeon, Cardiothoracic surgeon and Critical care in managing such cases to proceed with a thoracotomy and repair of the fistula. Any stricture formation is also identified on endoscopy. It is done 3-6 weeks after the removal of the foreign body [13]. Though there is a steady increase in the rates of battery ingestion and the major consequences associated with them, there is no standard protocol for the management of such cases. Hence, the present authors propose a protocol for button battery ingestion cases, as mentioned in [Table/Fig-7] [1,12].
Protocol for management of button battery ingested foreign body.
Awareness should begin at the level of Industrial manufacturers who should be educated about the environmental hazards of these products and to reduce the production of larger size batteries and switch over to equivalent smaller sizes batteries that easily pass through the GI tract. Manufacture of products with button batteries should have a child-proofing system to secure it from the reach of toddlers and should also be packed in solid individual child resistant packs [4]. Public awareness programs help in educating the parents to be aware of these complications to avoid usage of such products and to keep such products out of the reach of children [9].
Conclusion
With the increase in the usage of button batteries among household, the incidence of fatalities associated with the ingestion of button batteries has also increased. The most common sequelae leading to fatality is aorto-oesophageal fistula causing catastrophic haemorrhage in previously healthy children. This mandates the need for a standard protocol formation for the management of these cases. It is also important that all Primary health care physicians, Paediatricians and emergency practitioners should be aware of this emerging hazard for prompt management.
[1]. Litovitz T, Whitaker N, Clark L, White NC, Marsolek M, Emerging battery ingestion hazard: clinical implicationsPaediatrics 2010 125(6):1168-77.10.1542/peds.2009-303720498173 [Google Scholar] [CrossRef] [PubMed]
[2]. Wright K, Parkins K, Jahn H, Rowlands R, Davies F, Catastrophic haemorrhage from button battery ingestion in children: a growing problemActa Paediatrica 2017 106(9):1391-93.10.1111/apa.1393428795497 [Google Scholar] [CrossRef] [PubMed]
[3]. Slamon NB, Hertzog JH, Penfil SH, Raphaely RC, Pizarro C, Derby CD, An unusual case of button battery-induced traumatic tracheoesophageal fistulaPaediatr Emerg Care 2008 24(5):313-16.10.1097/PEC.0b013e31816ecb9a18496117 [Google Scholar] [CrossRef] [PubMed]
[4]. Lahmar J, Célérier C, Garabédian EN, Couloigner V, Leboulanger N, Denoyelle F, Esophageal lesions following button-battery ingestion in children: Analysis of causes and proposals for preventive measuresEur Ann Otorhinolaryngol Head Neck Dis 2018 135(2):91-94.10.1016/j.anorl.2017.09.00429054752 [Google Scholar] [CrossRef] [PubMed]
[5]. Injuries from Batteries Among Children Aged <13 Years: United States, 1995-2010: Morbidity and Mortality Weekly Report 2012 61(34):661-66. [Google Scholar]
[6]. Yoshikawa T, Asai S, Takekawa Y, Kida A, Ishikawa K, Experimental investigation of battery-induced esophageal burn injury in rabbitsCrit Care Med 1997 25(12):2039-44.10.1097/00003246-199712000-000229403755 [Google Scholar] [CrossRef] [PubMed]
[7]. Lee JH, Foreign body ingestion In childrenClin Endosc 2018 51(2):129-36.10.5946/ce.2018.03929618175 [Google Scholar] [CrossRef] [PubMed]
[8]. Anfang RR, Jatana KR, Linn RL, Roades K, Fry J, Jacobs IN, pH-neutralizing esophageal irrigations as a novel mitigation strategy for button battery injuryLaryngoscope 2019 129(1):49-57.10.1002/lary.2731229889306 [Google Scholar] [CrossRef] [PubMed]
[9]. Yardeni D, Yardeni H, Coran AG, Golladay ES, Severe esophageal damage due to button battery ingestion: can it be prevented?Paediatr Surg Int 2004 20(7):496-501.10.1007/s00383-004-1223-615221361 [Google Scholar] [CrossRef] [PubMed]
[10]. Wallace B, Landman MP, Prager J, Friedlander J, Kulungowski AM, Button battery ingestion complicationsJ Paediatr Surg Case Rep 2017 19:01-03.10.1016/j.epsc.2016.12.009 [Google Scholar] [CrossRef]
[11]. Russell RT, Cohen M, Billmire DF, Tracheoesophageal fistula following button battery ingestion: Successful non-operative managementJ Paediatr Surg 2013 48(2):441-44.10.1016/j.jpedsurg.2012.11.04023414882 [Google Scholar] [CrossRef] [PubMed]
[12]. Brumbaugh DE, Colson SB, Sandoval JA, Karrer FM, Bealer JF, Litovitz T, Management of button battery-induced hemorrhage in childrenJ Paediatr Gastroenterol Nutr 2011 52(5):585-89.10.1097/MPG.0b013e3181f9891621502830 [Google Scholar] [CrossRef] [PubMed]
[13]. Mortensen A, Hansen NF, Schiødt OM, Fatal aortoesophageal fistula caused by button battery ingestion in a 1-year-old childAm J Emerg Med 2010 28(8):984.e5-984.e6.10.1016/j.ajem.2010.01.00720825843 [Google Scholar] [CrossRef] [PubMed]