Vitiligo is a common, chronic, acquired cutaneous depigmentation disorder inducing loss of melanocytes in the skin and mucosa, having a 0.5% to 2% incidence worldwide, without preference for sex or race. Vitiligo is one of the renowned autoimmune diseases in which depigmentation can evolve throughout life in affected persons, particularly in the case of generalised vitiligo [1]. Clinically, vitiligo usually presents with sharply demarcated, totally amelanotic (milk-white) macules and patches surrounded by normal skin. There are several forms of the disease with different clinical presentation and prognosis. In 2011, Global Issues Consensus Conference (VGICC) was held in Bordeaux in which the most recent classification system was created for vitiligo. According to this classification, vitiligo can be divided into two main types: non-segmental vitiligo and segmental vitiligo [2]. Non-segmental vitiligo can be generalised, acrofacial, universal, mucosal, and mixed (associated with SV) and, rare type’s non-segmental vitiligo includes vitiligo punctata and hypochromic vitiligo. Segmental vitiligo further classified into Uni-, bi-, or plurisegmental, focal and mucosal [2]. The pathogenesis is complex and involves the interaction of multiple factors; however, the exact pathogenesis remains unknown. In the 1950s, the neural theory was hypothesised by Dytoc M and Malhotra N, and after that, a model of Reactive Oxygen Species (ROS), the autoimmune hypothesis and the melanocytorrhagy hypothesis have been postulated [3]. Gauthier Y et al., combined the concepts from other theories mentioned before and postulated “melanocytorrhagy” theory in 2003 which is widely accepted. According to this theory, non-segmental vitiligo occurs due to “melanocytorrhagy” [4]. Melanocytorrhagy is defined as a chronic melanocytes detachment or loss from the basal membrane caused by trauma and other stressors include catecholamines, ROS or autoimmune elements. Melanocytes detachment induces apoptosis resulted in melanocytes death lead to vitiligo [5]. Vitiligo has a dominant impact on self-esteem and social life and the quality of life is also remarkably depreciated in patients with this disease.
Albeit the availability of various interventions to treat the patient with vitiligo, still, no specific treatment has been developed. Even though various treatment modalities, such as topical corticosteroids, topical vitamin D3 derivatives, phototherapy including Psoralen Ultraviolet A (PUVA), Narrowband Ultraviolet B (NB-UVB) and 308-nm excimer laser, melanocyte transplantation, skin grafting and psychological therapy are available, choosing a treatment can sometimes be overwhelming, as various factors including safety, efficacy, minimal invasiveness and cost-efficiency should be comprehensively considered [6]. Recently, a Non-Cultured Epidermal Cell Suspension (NCECS) is emerging as the first line of surgical management of stable vitiligo [7]. Oral medication tofacitinib (Janus kinase (JAK) inhibitor) which is already approved for use in rheumatoid arthritis patients is emerging as newer therapy for vitiligo still robust evidence are not reported to support it’s used in vitiligo [8]. Among these therapeutic strategies, phototherapy is a mainstay of vitiligo treatment with varying rates of efficacy. Phototherapy has numerous advantages over the above mentioned other conventional therapy including safe for long-term use in adults, children, pregnant women, and immune-depressed persons, no increased risk of skin cancer, whereas biologic medications have a risk of organ toxicity and are linked with cancer, phototherapy equipped with safety features. By contemplating these entire factors, phototherapy is the preferred treatment of choice for the physician [9].
In 1997, Westerhof W and Nieuweboer-Krobotova L, firstly introduced narrow-band UVB (NB-UVB), more recent form of phototherapy which comprises a subset of the UVB spectrum centred at 311 nm for the treatment of vitiligo and concluded that 311-nm UVB radiation is as efficient as topical PUVA and has fewer adverse effects such as phototoxicity, itching and xerosis [10]. After that, Njoo MD et al., and Menchini G et al., have recorded the benefit of NB-UVB when given three times a week as monotherapy resulted in minimal side effect and well tolerated in vitiligo patient [11,12]. Recently, an increasing number of reports suggest that various topical agents or ablative methods including antioxidants [13,14], calcineurin inhibitors [15-17], fractional ablative CO2 laser [18-20], combined use of Er: YAG resurfacing and 5-fluorouracil [21], dermabrasion [22], only 5-fluorouracil [23] also vitamin-D3 analogues [24] has produced synergistic effects when combined with phototherapy. And this combination therapy giving better improvement compared to monotherapy of NB-UVB. In literature there was no systematic review available to compile these data and give proper justification for the favourable outcome. In this study, a systemic review of 12 RCTs with a total of 460 patches or patients were summarised and a meta-analysis was carried out to compare the efficacy of combination therapy of 311 nm NB-UVB with topical agents including calcineurin inhibitors, antioxidants, corticosteroids, vitamin-D3 analogues and 5-fluorouracil or lasers versus NB-UVB monotherapy used for prevention or treatment of vitiligo. Meta-analysis was performed to obtain a more reliable conclusion and, provide some guidance for treating vitiligo in clinical settings.
Materials and Methods
This systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (PRISMA). Ethical approval was not required as all included primary data had been previously published with ethical approval.
Search Methods for Identification of Studies
In January 2019, a search of PubMed (from 2000 to 2018), Science direct (from 1995 to 2018) and Cochrane Central Register of Controlled Trials (from 2005 to 2017) were performed. The search terms included the keyword “NB-UVB” or “narrowband ultraviolet B” combined with the Medical Subject Headings (MeSH) “Vitiligo”. The search strategy was “NB-UVB” or “narrowband ultraviolet B” and “Vitiligo”. The reference lists of all relevant articles were searched for additional information.
Inclusion and Exclusion Criteria
The following types of trials were included: (i) studies must be clinical RCTs; (ii) participants were children or adults with a diagnosis of vitiligo regardless of specific age criterion; (iii) they must include NB-UVB monotherapy for one group and the combination of NB-UVB with any topical agents or lasers for another group; (iv) at least 10 subjects or patches in each treatment arm irrespective of drop-out rates; (v) treatment for equal or more than eight weeks or 20 sessions of NB-UVB therapy; (vi) full-text article published in the English language.
The following types of trials were excluded: (i) irrelevant studies including research from other languages than English and abstracts only were discarded from study analysis; (ii) controlled but non-randomised trials; (iii) repeated studies; (iv) without the main outcomes which was desired; and (v) retrospective studies.
Assessment of the Risk of Bias
The quality of the RCTs was determined by two reviewers using the Cochrane Collaboration risk-of-bias tool, which assesses random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. All parameters were categorised as low, unclear, or high risk of bias [25].
Outcome Measures
The primary outcome of interest was the proportion of treatment success, defined as 75% or more repigmentation of each designated patch or the whole lesion in a patient. The results of other measurements (25-50% repigmentation, 50-75% repigmentation) were excluded. The secondary outcome was the proportion of treatment failure, defined as <25% repigmentation of each designated patch or whole lesion in a patient. The primary authors were communicated for further information when necessary.
Data Selection and Extraction
Two reviewers worked independently through all stages of the review, including screening papers for eligibility, examining full-text versions of studies for eligibility and inclusion in the meta-analysis. Any disagreements were resolved through discussion with the third author and reasons for decisions documented. The present authors extracted the following: the study design, the number and description of participants, targeted subtype and duration of vitiligo, type of topical treatments or lasers, details of the NB-UVB treatment protocols, and primary and secondary outcomes.
Data Synthesis
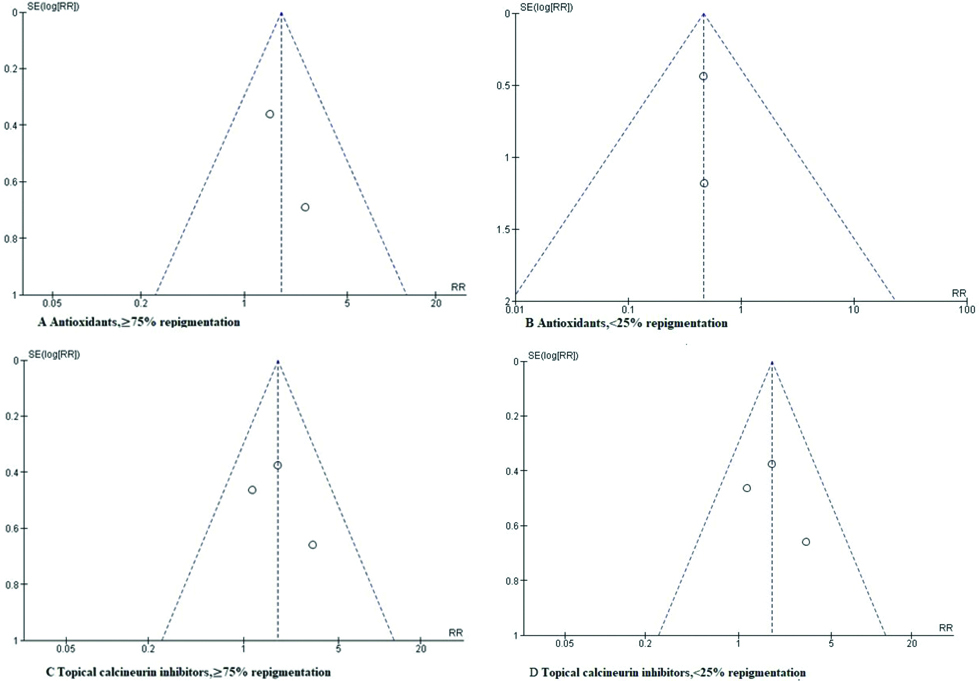
Heterogeneity across studies was evaluated using the chi-square test and Higgins I2 statistic. When substantial heterogeneity was observed (p<0.1 for the chi-square test and an I2 value >50%), a random effects model was applied. Otherwise, a fixed effects model was used. To aid the interpretation, the number needed to treat was calculated on the basis of the pooled RRs. Funnel plots were used to assess publication bias qualitatively. The meta-analyses were performed using Review Manager, Version 5.3 (Nordic Cochrane Center, Copenhagen, Denmark). To ensure the reliability and accuracy of the results, two reviewers populated the data in the statistical software programs independently and got the same results.
Results
Search Results
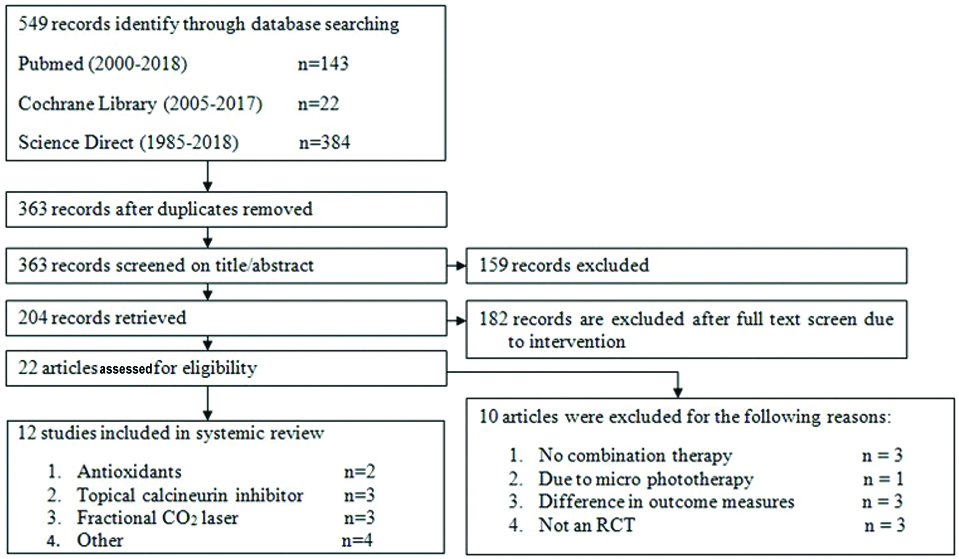
Through systemic bibliographic retrial of the PubMed (n=143), Science direct (n=384) and Cochrane Central Register of Controlled Trials (n=22), total 549 (143+22+384) records screened. After the removal of duplicate records, out of 549, 363 records are retrieved which were screened for title and abstract. After a title and abstract screening, 159 were excluded due to reason that the study does not contain the matter related to this meta-analysis. After these, 204 records are retrieved. Of 204 records, 182 are again excluded after full-text screening due to intervention not associated to study concern. Finally, a total of 22 full-text articles were assessed for eligibility, 10 of which were excluded for the following reasons: 1) no combination therapy (n=3) [26-28]; 2) difference in outcome measures (n=3) [29-31]; 3) due to micro phototherapy (n=1) [32]; and 4) not an RCT (n=3) [33-35]. Finally, 12 studies were included in this meta-analysis [Table/Fig-1]. The twelve included studies were all RCTs, with a total of 460 patches or patients [13-24].
Flow chart of the methodology according to PRISMA guidelines.
Study Characteristics and Quality Assessment
A total of 426 patches or patients were included in the combination therapy of various topical agents or lasers group and, 434 patches or patients were included in the NB-UVB monotherapy group. All studies included participants regardless of age and sex. Among the 12 RCTs, two studies were performed in India, one in Iran, one in Pakistan, one in Korea, one in Thailand, three in Egypt, one in Italy, one in France and one in China. The studies in Iran included the highest number of patients. The [Table/Fig-2] compiles the characteristics of each included trials. A total of 460 patients/patches with vitiligo were included, no matter adult or children. Of all the included RCTs, six studies mentioned a specific randomisation method for treatment allocation. Three were double-blinded study moreover seven were intraindividual comparative trials. The type of topical agent was an antioxidant in two studies [13,14], calcineurin inhibitor in three studies [15-17], fractional CO2 laser in three studies [18-20], and others four containing different topical treatments or laser treatments including, ER:YAG laser ablation and 5-fluorouracil combination, dermabrasion, 5-fluorouracil injection and calcipotriol ointment [21-24]. No ongoing studies were found in the clinical trials government registry.
Characteristics of the selected study in the analysis.
| Study | Country | Study design | Enrolled patients/patches | Location of lesions | Type of vitiligo and fitzpatrick skin type | Mean age (Range) (years) | Mean duration of disease (Range) | Topical or laser treatment | NB-UVB protocol |
|---|
| Antioxidants |
| Dell’Anna ML et al., 2007 [13] | Italy | Randomised, double-blind, placebo-controlled multicentre trial | 35 | NR | Nonsegmental vitiligo, I,II,III,IV,V and VI | 39.9 (range 24-61) | Range 1-10 years | Two tablets of AP per day for 8 weeks before starting phototherapy and 6 months during the UVB treatment. | Twice weekly for 6 month (Waldmann UV-8001 booth, equipped with 48 TL01/100 W Philips fluorescent tubes; Herbert Waldmann GmbH & Co, Villingen-Schwenningen, Germany) |
| Li L et al., 2016 [14] | China | RCT | 50 | NR | Non-segmental and progressive vitiligo | 35 (range 18-53) | NR | A compound betamethasone injection (Schering Pharmaceutical Co., Ltd. In Shanghai)was intramuscularly injected 3 times at one month interval. A commercial ALA (Shandong Qidu Pharmaceutical Co., Ltd., China) was orally taken 300 mg per day for 6 months. | Twice or three times a week for 6 month ((SS03 or SS05, Shanghai Sigma High-tech Co., Ltd., China) |
| Topical calcineurin inhibitors |
| Satyanarayan HS et al., 2013 [15] | India | Randomised intra-individual open comparative trial | 25 | Face, trunk, hands, feet, bony prominence, upper limb and lower limb | Generalised Stable vitiligo, III,IV and V | Range 14-36 | NR | Four weeks prior to start of therapy, Tacrolimus ointment(Topgraf) 0.1% applied once daily at night | Thrice weekly for 6 months (V-care UV therapy unit, Surya 440 ANB) |
| Esfandiarpour I et al., 2009 [16] | Iran | Randomised, double-blind, placebo-controlled study | 68 | Face+neck, trunk, arms, legshands+feet | Generalised, Localised Acrofacial and Segmental | T:25.92±10.31 (range 16-56) C:34.6±15.67 (range 15-72) | T:9.72±7.9 C:11.44±9.32 (years) | Pimecrolimus 1% cream (Elidel; Novartis, UK) or placebo twice daily | Three times per week for 3 months (UV 7001K phototherapy unit, comprising Phillips TL01 311 nm lamps; Waldmann, Germany) |
| Bilal A et al., 2014 [17] | Pakistan | Randomised, double-blind, placebo-controlled trial | 60 | Face and neck | Segmental and nonsegmental | T: 38.92±6.35 C: 37.54±7.04 | NR | Tacrolimus 0.1% ointment or placebo twice daily | Tri-weekly |
| Fractional CO2 laser (10,600 nm) |
| Shin J et al., 2012 [18] | Korea | Prospective, randomised half-body comparative study | 10 | Hand, foot forearm, abdomen, flank, groin, and thigh | Refractory nonsegmental vitiligo, IV | 59.5±10.42 (range 37-74) | 16.75±18.32 (range 2.5-58) years | Two sessions of fractional CO2 laser therapy at a 2-month interval (Lutronic Corporation, Goyang, Korea) | Twice a week for 2 months (UV7001K; Waldmann, Villingen-Schwenningen, Germany) |
| Vachiramon V et al., 2016 [19] | Thailand | Prospective randomised intra individual study | 27 | Both hands | Non-segmental vitiligo, III, IV and V | 51.2±8.5 | 70.58±25.69 months | 10-weekly sessions of fractional CO2 laser therapy at a 2-week interval (Lutronic Corporation, Goyang, Korea) Topical 0.05% Clobetasol propionate cream was applied twice daily throughout study period | Twice weekly for 20 sessions (M-series, Bryan, OH) |
| Doghaim NN et al., 2018 [20] | Egypt | Prospective, controlled comparative study | 32 | Extremities, acral parts, head, neck and trunk | Stable bilateral vitiligo, III, IV and V | 28±5.65 (range 18-35) | 2.72±1.03 (1-5) years | Two sessions of fractional CO2 laser for two months followed by NB-UVB phototherapy (Microxel MX7000, Daeshin Enterprise, Korea) | Three times per week for a maximum of 4 months (Philips TL 100, Hamburg, Germany) |
| Others |
| Anbar TS et al., 2008 [21] | Egypt | Prospective left-right comparative study | 50 | Upper limbs, hands, fingers, lower limbs, feet, trunk | Non-segmental vitiligo | 30.7±9.9 (range 17-54) years | NR | Fidelis XS ER:YAG laser (Fotona Medical Lasers, Ljubljana, Slovenia) Fluorouracil 5% cream applied for two days | Twice weekly for a maximum period of 4 months (eight NB fluorescent tubes (Philips TL 100 W/01) with a spectrum of 310-315 nm and a maximum wavelength of 311 nm installed in a Waldmann UV-1000 unit (Philips B.V and Waldmann GmbH, respectively, Eindhoven, the Netherlands and Schwenningen, Germany). |
| Bayoumi W et al., 2012 [22] | France | Single-centre prospective randomised controlled trial | 16 | Bony prominences and/or extremities. | Nonsegmental vitiligo, II, III and IV | 49 (range 29-72) | NR | Dermabrasion was performed using a 2940-nm erbium laser(Burane; Quantel, Les Ulis, France)Hydrocortisone17-butyrate cream was applied daily for three periods of 3 weeks followed by a 1-week steroid-free interval. | Twice weekly sessions also for 12 weeks. |
| El-Samad Z et al., 2012 [23] | Egypt | Randomised, left-right comparative study. | 60 | Extremities, trunk, facial and acral | Localised stablenon-segmental and acral vitiligo, III and IV | 28±5.65 (range 18-35) | NR | 5-FU solution was prepared under sterile conditions.Injections of about 0.01-0.02(50 mg/mL) mL were applied intradermally in the vitiligo area at 1 cm intervals to a maximum of 250 mg per session (total of 5 mL).This was repeated every 2 weeks for 4 months. | Twice/week sessions for a maximum of 4 months (Philips TL 100, Waldmann UV-100 unit.) |
| Khullar G et al., 2015 [24] | India | Prospective right-left comparative study | 27 | Lower limbs TrunkFace and neck | Vitiligo vulgaris,acrofacial vitiligo,III, IV and V | 24.4±8.6 (range 12-37) | 9.7±4.9 (2-20) years | Calcipotriol ointment (0.005%) was applied twice a day | Thrice a week for 24 weeks (V-care UV therapy unit, Surya 440 ANB, V-care medical systems Pvt Ltd, Bangalore, Karnataka, India) |
Risk of Bias in Included Studies
All of the included studies were described as randomised. The results are summarised in the risk-of-bias graph [Table/Fig-3], which provides an overview of the reviewers’ judgments of each category presented as percentages across all included studies. The [Table/Fig-4] shows the risk-of-bias summary of each risk-of-bias item for each included study.
Risk-of-bias graph. The judgments of each risk-of-bias item are presented as percentages across all included studies.
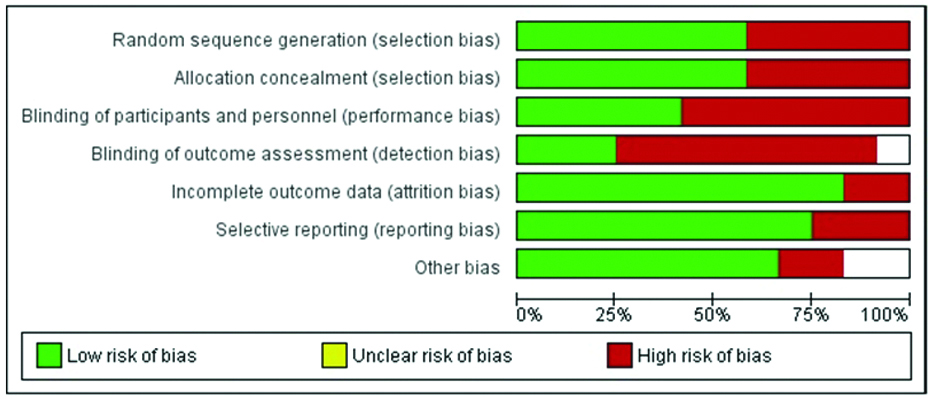
Risk-of-bias summary. The judgments of each risk-of-bias item for each included study.

Effect of Interventions
Antioxidants: One RCT compared the efficacy of NB-UVB and antioxidant pool combination therapy versus NB-UVB monotherapy and another RCT compared the efficacy of NB-UVB, betamethasone and antioxidant combination therapy versus NB-UVB and betamethasone [13,14]. A total of 37 combination therapy and 30 monotherapy cases or patches were included [Table/Fig-5]. Fixed effects pooling of the results showed that combination therapy had a significantly superior effect on the treatment success of vitiligo (2 studies: RR 1.77, 95% CI 0.93 to 3.35; number needed to treat 4.68, 95% CI 2.22 to 41.69) [Table/Fig-6]. Visual inspection of the forest plot and statistical testing demonstrated negligible between-study heterogeneity (I2=0%, p=.08). The combination therapy also significantly reduced treatment failure in vitiligo (two studies: RR 0.46, 95% CI 0.20 to 1.06). The symmetry of the funnel plots indicated no publication bias [Table/Fig-7].
Interventions and clinical outcomes in the studies included in this review.
| Study | Intervention | Analysed patients/lesions N | Clinical outcomes, n (%) |
|---|
| <25% repigmentation | ≥75% repigmentation |
|---|
| Antioxidants |
| Dell’Anna ML et al., 2007 [13] | T: NB-UVB+antioxidant pool(AP) | T:17 patients | T:5 | T:8 |
| C: NB-UVB alone | C:11 patients | C:7 | C:2 |
| Li L et al., 2016 [14] | T: NB-UVB+oral α lipoic Acid+betamethasone injection | T:20 patients | T:1 | T:11 |
| C: NB-UVB+placebo+betamethasone | C:19 patients | C:2 | C:7 |
| Topical calcineurin inhibitors |
| Satyanarayan HS et al., 2013 [15] | T: NB-UVB+topical tacrolimus | T:21 patches | T:2 | T:7 |
| C: NB-UVB alone | C:21 patches | C:2 | C:6 |
| Esfandiarpour I et al., 200 [16] | T:NB-UVB+pimecrolimus | T:75 patches | T:31 | T:8 |
| C:NB-UVB+placebo | C:90 patches | C:39 | C:3 |
| Bilal A et al., 2014 [17] | T: NB-UVB+topical tacrolimus | T:60 patients | T:0 | T:16 |
| C: NB-UVB alone | C:60 patients | C:4 | C:9 |
| Fractional CO2 laser (10,600 nm) |
| Shin J et al., 2012 [18] | T: NB-UVB+fractional CO2 laser | T:10 patients | T:2 | T:0 |
| C: NB-UVB alone | C:10 patients | C:0 | C:0 |
| Vachiramon V et al., 2016 [19] | T: NB-UVB+fractional CO2 laser+topical clobetasol propionate cream | T:26 patches | T:3 | T:2 |
| C: NB-UVB+topical 0.05% clobetasol propionate cream | C:26 patches | C:5 | C:1 |
| Doghaim NN et al., 2018 [20] | T: NB-UVB+fractional CO2 laser | T:32 patients | T:10 | T:8 |
| C:NB-UVB alone | C:32 patients | C:2 | C:0 |
| Others |
| Anbar TS et al., 2008 [21] | T: NB-UVB+ER:YAG laser ablation+5-fluorouracil | T:64 patches | T:14 | T:28 |
| C:NB-UVB alone | C:64 patches | C:50 | C:5 |
| Bayoumi W et al., 2012 [22] | T: NB-UVB+topical steroid+ Dermabrasion | T:16 patients | T:7 | T:2 |
| C: NB-UVB+topical steroid | C:16 patients | C:14 | C:0 |
| El-Samad Z et al., 2012 [23] | T: NB-UVB+5-fluorouracil injection | T:60 patches | T:9 | T:29 |
| C: NB-UVB alone | C:60 patches | C:50 | C:4 |
| Khullar G et al., 2015 [24] | T: NB-UVB+calcipotriol ointment | T:25 patients | T:3 | T:4 |
| C: NB-UVB alone | C:25 patients | C:5 | C:6 |
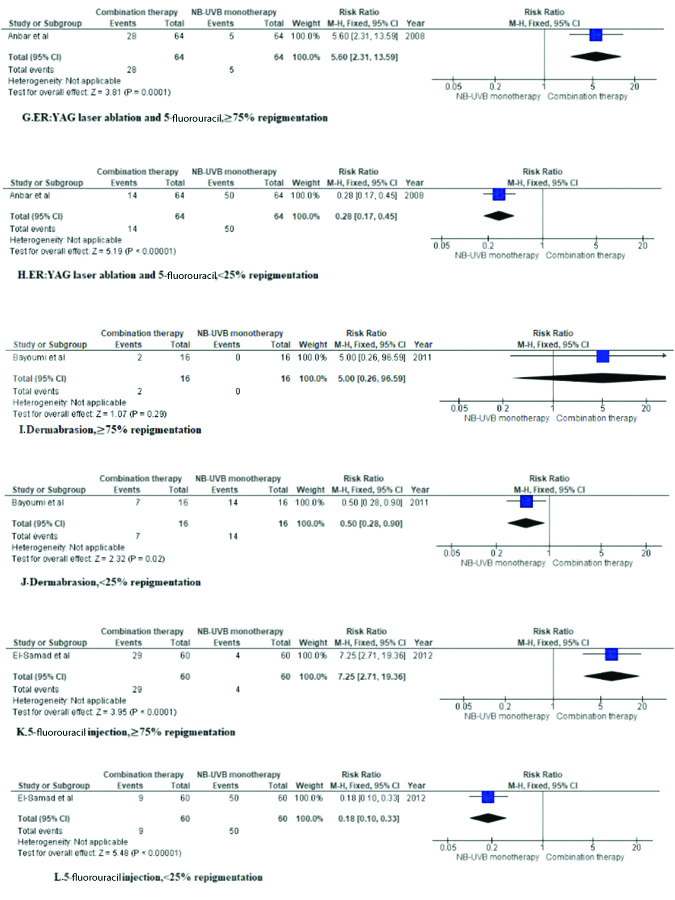
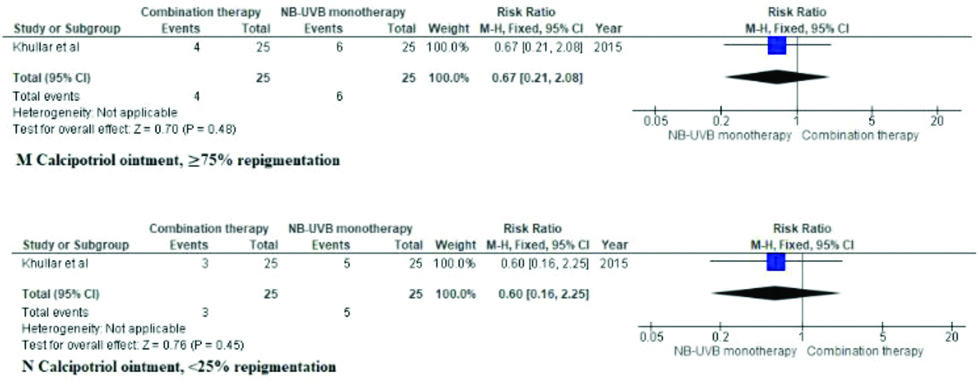
Forest plot indicate efficacy of NB-UVB alone or in combination with topical treatments or lasers for vitiligo. CI, Confidence Interval.

Symmetrical funnel plots of antioxidants and topical calcineurin inhibitors recommended no publication bias.
7a- antioxidants good response; 7b- antioxidants poor response; 7c- TCI good response; 7d- TCI poor response
Topical Calcineurin Inhibitors
Three RCTs compared the efficacy of NB-UVB and topical calcineurin inhibitor combination therapy versus NB-UVB monotherapy [15-17]. The type of calcineurin inhibitor used was tacrolimus in two studies [15,17] and pimecrolimus in one study [16]. A total of 156 combination therapy and 171 monotherapy cases or patches were included [Table/Fig-2]. Fixed effects pooling of the results showed that combination therapy had a significantly superior effect on the treatment success of vitiligo (three studies: RR 1.79, 95% CI 1.06 to 3.01; number needed to treat 10.7, 95% CI 5.85 to 62.49) [Table/Fig-6]. Visual inspection of the forest plot and statistical testing demonstrated negligible between-study heterogeneity (I2=0%, p=0.44). Regarding the secondary outcome, the combination therapy had no significant effect on reducing the treatment failure rate (three studies; RR 0.87, 95% CI 0.61 to 1.23). The funnel plots did not indicate publication bias [Table/Fig-7].
Fractional CO2 Laser
Three RCTs compared the efficacy of NB-UVB and fractional CO2 laser combination therapy versus NB-UVB monotherapy. The success rates of both groups were 0 in one RCT [18-20]. Combination therapy showed a significantly better effect (two studies; RR 7, 95% CI 1.30 to 37.60) compared to monotherapy. Regarding the secondary outcome, the combination therapy had no significant effect on reducing the treatment failure rate (three studies; RR 2.10, 95% CI 0.42 to 10.56).
Other
For ER:YAG laser ablation and 5-fluorouracil also 5-fluorouracil injection studies, fixed effects pooling of the results showed that combination therapy had a significantly superior effect on the treatment success of vitiligo. Dermabrasion study had a minor effect on treatment success. Fixed effects pooling of the calcipotriol results showed that monotherapy had a significantly superior effect on the treatment success of vitiligo. Concerning treatment failure for included study, the combination therapy had no significant effect on reducing the treatment failure except calcipotriol study had little pooling towards combination therapy. As all included study were individual, heterogeneity between-study was not identified. Moreover, all details are visualised in forest plot [Table/Fig-6].
Discussion
Even though nowadays, there are several therapeutic options available including medicine, phototherapy and surgical grafts, the treatment of vitiligo is still the most difficult dermatologic challenges [36,37]. Current therapeutic options for vitiligo are limited by inconsistent and incomplete responses, relapses and side-effects of treatments. Moreover, phototherapeutic options are generally limited by the requirement that long-term treatment takes place on a twice weekly or three times weekly basis over a period varying from several months to years. Njoo MD et al., studied the efficacy and safety of NB-UVB (311 nm) therapy in children with generalised vitiligo and, from the study reported that NB-UVB is one of the most efficacious treatments with an optimum side-effect profile and an average response rate of 62% although 6-12 months of treatment are needed before optimum results are seen [11]. Since then, there have been other studies strengthening the superiority of NB-UVB [38,39]. The mechanism of the action of NB-UVB is still not cleared but, it seems to be an inhibitory effect on cytotoxic T lymphocytes and, conversely, on stimulation of the release of cytokines involved in melanocyte migration and proliferation [40].
For NB-UVB monotherapy, a lot of effort and commitment is demanded and apart from this it required several months to achieve a satisfactory effect. To avoid this consequence combination therapies that could be used along with NB-UVB are fruitful, with an aim to maximise efficacy and cut short the course of this treatment regimen, at least to some extent. NB-UVB and antioxidants, mainly vitamin E and α-lipoic acid, work through following two different mechanisms: (i) regulating immunosuppression and stimulating melanocyte replication and proliferation; and (ii) regulating the antioxidant balance, which is critical in vitiligo. Hence, this could mean that these two modalities are supplementary and synergistic [13]. Calcineurin inhibitors selectively inhibit the intracellular protein calcineurin and consequently suppress tumour necrosis factor-α and interferon-g expression, which is associated with the pathogenesis of vitiligo. In addition, tacrolimus enhances the production of stem cell factor and matrix metalloproteinases 2 and 9 and directly intensifies not only the proliferation of both melanocytes and melanoblasts but the migration of melanocytes as well [41,42]. Even though there are concerns on the risk of carcinogenic mutations when UV exposure and immunosuppressant drugs such as calcineurin inhibitors are applied simultaneously, tacrolimus was actually proved to be protective against UV-induced DNA damage and erythema by inhibiting early-phase inflammatory events [43]. Apart from these, calcineurin inhibitors have also been inferred to increase the tolerability to phototherapy through an immunomodulatory mechanism [44]. The postulated mechanism of ablative methods including fractional CO2 laser in repigmentation of vitiligo includes the secretion of cytokines and various growth factors during wound healing, which might serve as mitogens for melanocytes [17]. Also, reported that improvement in outcome was observed in ER: YAG laser skin ablation, followed by 5-FU application before NBUVB phototherapy compared to short-term NB-UVB therapy for vitiligo treatment. Furthermore, this combination of therapies is more safe and tolerable. On the basis of the study author concluded that the proposed mechanism involving in the mode of repigmentation in vitiligo lesions was either follicular and/or by extension of pigment from the edges, as the study of Cui J et al., [40], who found that the follicular repigmentation may be due to the reactivation of the melanocytes located in the outer root the sheath of the hair follicles inside the lesions and that activation of the contiguous pigmented skin may result in melanocytes migration for 2-3 mm into the depigmented skin. In 2012, dermabrasion led to a significant increase of pigmentation had occurred described by Bayoumi W et al., and they proposed the mechanism involved in this process [22]. The higher biological UV impact due to the dermabrasion is one of the hypotheses that could explain the effect of dermabrasion in increasing the repigmentation in vitiligo. Removal of affected keratinocytes increased penetration of the topical steroids and inducing inflammatory cytokines that might have a propigmenting action are other mechanisms that could have played a role [23]. Vitamin D receptors are expressed on melanocytes, keratinocytes and the immune system cells of the skin [36,45]. Since, vitamin D analogues (calcipotriol), binding its receptor (Vitamin D receptor-VDR), may stimulate melanin production by activating melanocytes and keratinocytes or may have an immuno-modulatory effect by acting on immune cells [24]. On the basis of the mechanisms of action of these treatments’ modality, they might work synergistically to get a better response in repigmentation.
According to this systematic review, combination therapy is superior compared to monotherapy in form of repigmentation except calcipotriol combined with NB-UVB. Among all combination therapy, the combination therapy of NB-UVB and antioxidant further NB-UVB and topical calcineurin inhibitors were more effective than NB-UVB monotherapy (RR 1.77, 95% CI 0.93 to 3.35; 1.79, 95% CI 1.06 to 3.01); this finding is supported by the highest level of evidence in the hierarchy of evidence with a low level of heterogeneity (I2=0%, p =0.08; I2=0%, p=0.44). The results showed that the administration of antioxidant to 4.68 subjects receiving NB-UVB treatment for vitiligo is necessary for one subject to improve (number needed to treat 4.68, 95% CI 2.22-41.69) and administration of topical calcineurin inhibitors to 10.7 subjects receiving NB-UVB treatment for vitiligo is necessary for one subject to improve (number needed to treat 10.7, 95% CI 5.85 to 62.49). The addition of antioxidant or topical calcineurin inhibitors to NB-UVB also reduced the treatment failure rate (<25% repigmentation) (RR 0.46, 95% CI 0.20 to 1.06; RR 0.87, 95% CI 0.61 to 1.23). In other groups, we had an individual study without any group category since the present authors could not perform a meta-analysis yet showed graphically in forest plot for visual representation. Although all RCT showed the significantly better effect of the combination therapy, it is troublesome to conclude that combination therapy of each analogue (topical agents or lasers) and NB-UVB is more effective than NB-UVB monotherapy. Moreover, the combination of each analogue and NB-UVB was not confirmed to be effective in reducing the treatment failure rate compared with NB-UVB monotherapy except calcipotriol failure outcome. Notably, success rate other combination can’t be predicted because the presence of high level heterogenicity (three studies: NB-UVB combined with fractional CO2 laser group) or could not find heterogenicity as single study (four studies: Others group; NB-UVB combined with ER:YAG laser ablation and 5-fluorouracil, NB-UVB combined with topical steroid and dermabrasion, NB-UVB combined with 5-fluorouracil injection, NB-UVB combined with calcipotriol ointment). More clinical trials are needed to decide the efficacy of these combination therapies with NB-UVB and these analogues.
This meta-analysis has certain limitations. First, several trials had been excluded as; they weren’t RCTs, despite the desired outcome [30]. Second, some RCTs were excluded because they didn’t allow the desired outcome [29-31]. Third, there may be therapies that showed no significant difference in efficacy but have meaningful benefits in practice. These benefits may not have been captured because of insufficient sample size or the limitations of the available outcome measures. Fourth, the use of topical corticosteroid in both groups was allowed in this review and, it could be effective in combination with either NB-UVB or NB-UVB and specific analogue (topical agents or laser). In addition, the mean patient age and mean duration of disease were inconsistent among studies and therapies differed in duration and frequency of treatment in these studies. Lastly, some RCTs included in this systematic review conducted without predetermined inclusion and exclusion criteria, and obtained results have several implications on treatment strategies in patients with vitiligo. However, this study attempted to present the best conclusion with limited numbers of RCTs as objectively as possible according to predetermined inclusion and exclusion criteria, and obtained results have several implications on treatment strategies in patients with vitiligo.
Limitation
The study has some limitations which are remarkable. This study is limited only to the selected database source and English-language publications and therefore might have missed some relevant publication. In this study, seven included RCTs did not followed the blinding policy for outcome assessment as the chance of detection bias is there. Three articles have not fulfilled the criteria for reporting high-quality studies.
Conclusion
In summary, this systematic review revealed that adding antioxidant and topical calcineurin inhibitors on NB-UVB yields significantly superior outcomes than NB-UVB monotherapy. Regarding the difficulties in complete recovery of vitiligo, the combination therapies manifest the promising result. More large-scale, high-quality, double-blind RCTs regarding the efficacy of topical agents or lasers plus NB-UVB combination therapy is required.