Myositis Ossificans Masquerading as Soft Tissue Giant Cell Tumour in Fine Needle Aspiration Cytology- A Case Report with Brief Review
J Priyadharisini1, Pammy Sinha2, Khowsalya Subrajaa3
1 Assistant Professor, Department of Pathology, Sri Lakshmi Narayana Institute of Medical Sciences, Affliated to Bharath University, Puducherry, India.
2 Professor, Department of Pathology, Sri Lakshmi Narayana Institute of Medical Sciences, Affliated to Bharath University, Puducherry, India.
3 Assistant Professor, Department of Pathology, Sree Balaji Medical College and Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. J Priyadharisini, No. 11, Govt Boys School, Street Muthialpet, Puducherry-605003, India.
E-mail: priyadharsini158@gmail.com
Myositis ossificans (MO) is a reactive condition that is sometimes mistaken microscopically for extraosseous osteosarcoma. Cytological features of MO are quite confusing because of various patterns of presentation in fine needle aspiration smears due to differences in phases of MO and thereby poses a diagnostic challenge to cytopathologist. Hence clinico-radiological correlation along with histopathology is useful for definitive diagnosis. As per the literature search, none of the cases of MO presented cytologically with extensive giant cells component leading to the diagnosis of Giant cell tumour of soft tissue. This case report aims to explore diagnostic dilemma in cytomorphology of MO which we experienced recently and rarity of occurrence of non-traumatic MO.
Biopsy, Histopathology, Zonation
Case Report
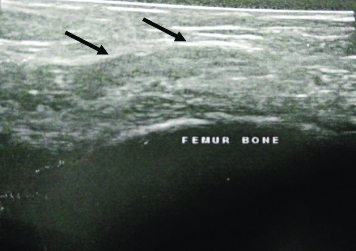
A 25-year-old female presented with four months history of palpable painful right upper thigh mass. She denied a history of trauma in the recent past, except for normal vaginal delivery six months back. On examination, there was a 5 cm firm-tender mass in the medial aspect of right thigh with a minimal limited range of motion. Ultrasonography revealed heterogenous intramuscular lesion measuring 3.3×1.4 cm with evidence of focal calcific specks in right thigh not involving underlying femur bone, suggested the possibility of a calcified intramuscular lipoma [Table/Fig-1].
Ultrasonography revealing extraosseous soft tissue mass lesion with focal calcified areas (Arrow marks).
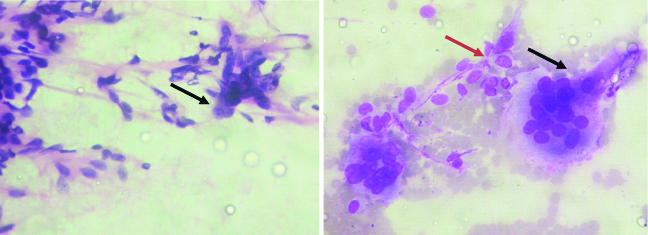
Fine Needle Aspiration Cytology (FNAC) of the lesion showed predominantly numerous osteoclastic type of giant cells, scattered mononuclear cells which were plump as well as spindle-shaped at places with occasional osteoblasts (recognised by its round to oval cell with eccentrically placed round nucleus and abundant cytoplasm) and haemorrhage, which suggested the possibility of the giant cell tumour of soft tissue. No evidence of adipocytes/calcification/osteoid and cytological atypia noted [Table/Fig-2,3].
FNAC shows many spindle cells, osteoblast and entangled osteoclasts (Pap & Giemsa, 20x) [Arrow marks-Red (Osteoblasts), Black-Osteoclast].
Ultrasonography and FNAC diagnosis in this case were discordant which reinforced the treating surgeon to further proceed for the conventional gold standard diagnostic histopathology method. This scenario indicates the potential pitfall of cytological diagnosis of Myositis Ossificans (MO) as well as the varied radiological presentation of it according to the age of the same lesion and implies the significance of histopathology diagnosis. The case was then posted for surgery. Intraoperatively, noted a well-circumscribed ovoid intramuscular gritty mass lesion measuring 3.5×1.5 cm within adductor magnus muscle. The lesion was removed surgically.
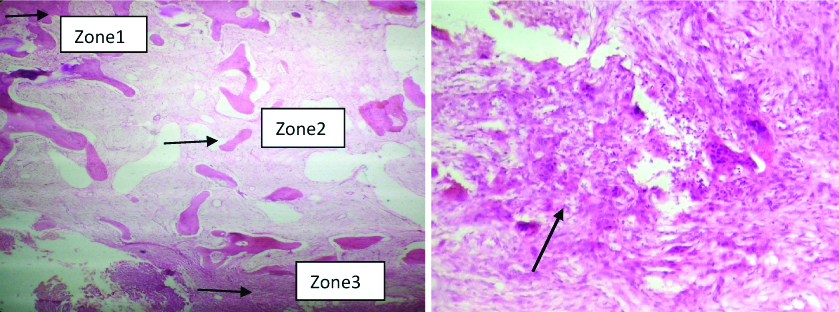
Histopathological examination revealed zonal architecture showing peripheral mature bone merging with woven bone lined by osteoblast and osteoclasts with central zone composed of proliferating vascular fibroblastic tissue with haemorrhage and extensive giant cells. No cytological atypia/malignant osteoid seen, which confirmed the diagnosis of MO and ruled out extra-skeletal osteosarcoma [Table/Fig-4,5]. Though MO is a self-limiting condition, surgical removal is the treatment of choice if symptomatic. Post operatively she was supported with a course of analgesics, antibiotic and anti-inflammatory drugs. Postoperative follow-up period (six months) was uneventful. Patient was asymptomatic and exhibited full range of motion of the limb.
Histopathology sections show Zonation pattern (arrow), central reactive zone with numerous giant cells (H&E-20x,40x).
Discussion
MO is one of the benign self-limiting mass which typically arises within large muscles of extremities. This occurs mainly following local trauma but can also be an incidental finding. It is most commonly seen in adolescent and young individuals. It generally affects flexor muscles of upper extremities and quadriceps, hamstring muscles of lower extremities [1]. The most accepted hypothesis of traumatic MO was that Bone Morphogenic Protein (BMP) signal from injury site induces perivascular mesenchymal cells to differentiate into osteoblast and chondroblast creating an appropriate environment for MO formation. Repetitive small mechanical pressure, ischemia, and inflammation are said to be the causes of non-traumatic MO which is rare and could be the probable cause (as our patient had a recent history of normal vaginal delivery) in our case [2]. MO is one of the difficult diagnosis by clinical, radiological methods as well as by cytological smears.
Differential diagnosis of any soft tissue mass (intramuscular) with calcification radiologically includes both benign and malignant aetiologies such as Dystrophic calcification following parasitic infestation (cysticercosis), following chemotherapy/radiotherapy of any soft tissue tumour, Intramuscular calcified lipoma, Injection granuloma, MO, and Extra-skeletal osteosarcoma which do have overlapping clinical findings [3,4]. Radiological misinterpretation, in this case, could be probably due to the early phase of MO which might not depict classical zonal phenomenon.
Cytological differential diagnosis of any soft tissue mesenchymal tumours that are rich in giant cells includes Nodular tenosynovitis (lacks typical spindle stromal cells with scattered giant cells, lymphocytes, macrophages and increased fibroblasts), Giant cell tumour of soft tissue (two population of cells including numerous elongated stromal cells with many osteoclastic type of giant cells, both of which showing similar nuclear morphology), Pigmented villonodular synovitis (haemosiderin laden multinucleated giant cells), Nodular fasciitis (polymorphic appearance with sheets of immature fibroblasts, inflammatory cells in myxoid background), Giant cell malignant fibrous histiocytoma/ Giant cell leiomyosarcoma (large deep-seated lesions with obvious nuclear atypia or mitosis/necrosis and Extra-skeletal osteosarcoma (atypical spindle cells with matrix material of osteoid) [5,6].
Despite numerous possible differential diagnoses, in this case, lack of history of trauma, as well as cytology showing extensive osteoclastic giant cells with background of spindle cells, were slightly misleading us to the diagnosis of giant cell tumour of soft tissue. Although rich giant cells in this case of MO in cytology could be explained as it might be aspirated from the reactive cellular central zone composed of extensive giant cells surrounding area of haemorrhage as noted in histopathology tissue sections [7].
Aspiration cytological findings of MO are not well documented but include variable cellular components such as plump mononuclear mesenchymal cells with oval nuclei accompanied by osteoblasts, fibroblasts, multinucleated giant cells, and rarely metachromatic amorphous stroma/osteoid. Dodd LG et al., found that the fibroblasts/myofibroblasts, osteoblasts and the amorphous stromal background are the commonest findings in FNAC of MO [6], however Villasenor EE et al., stated that the cytological findings of MO includes immature mesenchymal cells, osteoblasts, fibroblasts, and osteoclast-like cells giant cells [8].
The different cellular composition reflects different histologic components of a lesion. Each one of these cellular components can be a source of error in the cytologic diagnosis of MO. This greater variety of differential diagnosis increases the importance of careful analysis of aspiration smears for appropriate diagnosis.
Histologic hallmark of MO is the classical zonal phenomenon which includes mature bone at the periphery of the lesion (zone 1), woven bone in intermediate zone (zone 2) and vascular fibroblastic tissue (zone 3) mimicking nodular fasciitis in the central zone. As the lesion matures it forms cortical bone with mature fatty marrow at the periphery. Most important differential diagnosis histologically is extra-skeletal osteosarcoma, which can be differentiated from MO by following; osteoid deposition in MO is uniform and much broader than osteosarcoma, presence of reactive fibrous areas give clues to the benign nature of the MO and extra-skeletal osteosarcoma lacks or shows reverse zonation [9].
To authors knowledge, none of the cases reported in the literature, of MO presented as giant cell-rich lesion in FNAC which led to potential misdiagnosis in the present case. However, histopathological confirmation of benign or malignant nature of the lesion is required for guiding the further clinical management.
Conclusion
MO is a difficult diagnosis in cytology. Though cytology is a screening test to exclude malignancy in this scenario, a definite diagnosis is supplemented by histopathology. Hence, a complete knowledge about differential diagnosis, clinico-radiological correlation with confirmative histopathology serves a reasonable purpose for the patient for the future prognosis.
[1]. Mahale YJ, Vyawahare CS, Dravid NV, Upase A, Rathi R, A rare case of non traumatic myositis ossificans circumscriptaJ Orthop Case Rep 2015 5(3):15-17. [Google Scholar]
[2]. Li WT, Horng SY, Chien HF, Abdominis rectus intramuscular myositis ossificans: A rare case report and literature reviewFormosan Journal of Surgery 2016 49(1):20-26.10.1016/j.fjs.2015.06.004 [Google Scholar] [CrossRef]
[3]. Tyminiski M, Sirkie H, Case Report; Calcified thigh massJ Am Osteopath Coll Radiol 2013 2(4):29-31. [Google Scholar]
[4]. Banks KP, Bui-Mansfield LT, Chew FS, A compartmental approach to the radiographic evaluation of soft-tissue calcificationsSemin Roentgenol 2005 40(4):391-407.10.1053/j.ro.2005.01.02116218555 [Google Scholar] [CrossRef] [PubMed]
[5]. Asotra S, Sharm S, Giant cell tumour of soft tissue; cytological diagnosis of a caseJ Cytol 2009 26(1):33-35.10.4103/0970-9371.5486621938147 [Google Scholar] [CrossRef] [PubMed]
[6]. Dodd LG, Martinez S, Fine-needle aspiration cytology of pseudosarcomatous lesions of soft tissueDiagn Cytopathol 2001 24(1):28-35.10.1002/1097-0339(200101)24:1<28::AID-DC1004>3.0.CO;2-G [Google Scholar] [CrossRef]
[7]. Kishanprasad HL, Lobo L, Shetty JK, Impana BD, Giant cells in soft tissue tumours! Is it a clue to diagnosis or cytologists mystery? An unusual case reportJ Can Res Ther 2018 14(2):444-46. [Google Scholar]
[8]. Villasenor EE, Adilla ED, Martinez GR, Scrape cytology of myositis ossificans; Report of a case and analysis of cytology findings described previouslyDiagn Cytopathol 2008 36(1):50-53.10.1002/dc.2075218064693 [Google Scholar] [CrossRef] [PubMed]
[9]. Wimmer D, Myositis ossificansPathologyOutlines.comwebsite. http://www.pathologyoutlines.com/topic/softtissuemyositis.html. Accessed April 13th, 2019 [Google Scholar]