In the literature, generally five different methods have been reported for localising the maxillary IMC in sagittal direction on a single OPG. These are: (a) the superimposition of the IMC crown on the root or neck of the adjacent incisor [9,10]; (b) sector determination [11,12]; (c) magnification [9-11,13-17]; (d) vertical level or the position of the IMC crown [11,14,15,17]; and (e) angulation [10,18] (the angle between the occlusal plane and IMC axis).
Investigation of the superimposition of the IMC crown with the adjacent tooth root on OPGs was suggested by Ericson S and Kurol J, and this method was studied for early prediction and the treatment of palatally erupting maxillary canines [19,20]. Thereafter, Wolf JE and Mattila K, deduced that the IMC crown that overlaps with the root of the central incisor could be accepted as palatally localised [9]. Jung YH et al., evaluated five different sectors on OPGs and the sagittal location of IMCs was reported according to the sector in which the tip of the canine crown was located [12,19].
The magnification method is based on the physical rule that an object that is closer to the film cassette but farther away from the source of radiation has a smaller image on OPGs [9-11,13-17]. Due to the negative angle of the main beam of the radiation source relative to the object and film cassette while creating the image on panoramic radiographs, all the objects located in the palatal region have a higher image projection than the objects located labially on OPGs [14]. Therefore, a palatally located tooth has a vertically higher image position and increased crown width according to these rules [11,14,17].
Katsnelson A et al., stated that palatally located IMCs could not have a steep position because the palatal bone is thinner in the sagittal dimension; thus, palatally located canines lie horizontally at the palate [18]. According to this angulation method, the authors suggested that the angle between the palatally localised IMC and occlusal plane be smaller than 65°.
Materials and Methods
This study was approved by the Clinical Research Ethics Committee of Suleyman Demirel University, Isparta, Turkey (2012-KAEK-38.28.9.2016/150). It was conducted in Suleyman Demirel University, Faculty of Dentistry, Department of Orthodontics. The materials of this study consisted of the OPG-CBCT records of 69 individuals with unilateral or bilateral IMCs, who were seeking overall routine orthodontic treatment at Suleyman Demirel University, Faculty of Dentistry between the years 2014 and 2016. An experimental research design was performed to measure the validity and reliability of prediction methods. Twenty-five volunteer dentists predicted the sagittal locations of 85 IMC’s using five different prediction methods on OPGs. The inclusion criteria of the individuals with unilateral or bilateral IMCs that were included for radiographic evaluation were: (a) the presence of both a panoramic radiograph and CBCT with acceptable diagnostic quality; (b) 15 years of age or older; (c) permanent dentition; (d) systematic healthiness; (e) no rotations or mid-alveolus locations for IMCs; (f) no missing teeth at the anterior maxilla; and (g) no syndrome and/or no cleft lip and palate. To eliminate bias, a single-blind and randomised study was designed.
The radiographic records of 53 cases with unilateral canine impaction and 16 cases with bilateral canine impaction (85 IMCs in total) were included in this study. Panoramic radiographs were acquired from a digital panoramic device (PaX-400C®; Vatech Co., Ltd., Gyeonggi-Do, Korea). The images were exported as .JPEG files. CBCT scans of each patient were taken with ProMax3D Mid® (Planmeca Oy, Helsinki, Finland) (160x90 mm FOV; 0.4 mm voxel size; 90 kVp, 10 mA; 14 sec scanning time). All data sets were exported as DICOM (Digital Imaging and Communications in Medicine standard) files. The main criteria for taking CBCT, after the routine radiographic and cephalometric examination, was to determine the position of IMC for orthodontic treatment planning. The pairs of OPG and CBCT records of each individual were listed in alphabetical order according to surname {e.g., surname1 (OPG-CBCT), surname2 (OPG-CBCT),...}. While the OPGs were prepared in a computer-based .JPEG format for evaluation, the OPGs were randomised (Random Integer Generator, www.random.org/integers/) and then the IMCs were numbered [Table/Fig-1].
Evaluated OPG samples in this study.
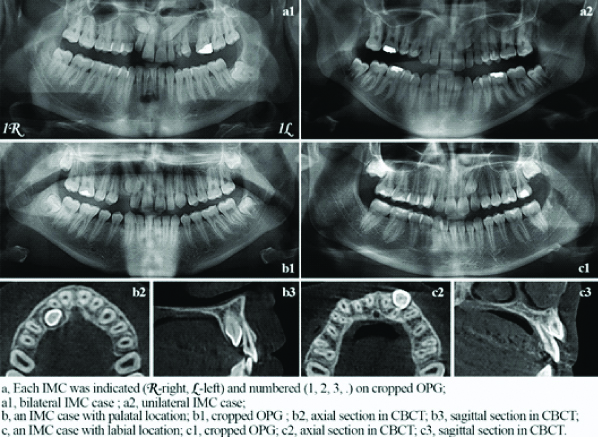
Before evaluation with the prediction methods by 25 volunteer dentists, the true locations as “palatal” or labial” of each IMC was determined as Jung YH et al., by an oral radiologist (17 years of clinical and teaching experience) with CBCT [Table/Fig-1] and recorded [12]. Each IMC was evaluated by an orthodontist (20 years of clinical and teaching experience) with each predicting method with computer-aided measurement using computerised measurement software (Planmeca Romexis 3.2.0.R, Helsinki, Finland). For precise results, each measurement or evaluation was performed three times and the average value was accepted. Then, frequency distributions of IMCs were determined [Table/Fig-2].
Frequency distributions of impacted maxillary canines.
| Characteristics | N | Valid percent (%) |
|---|
| Unilateral-bilateral | Unilateral | 53 | 62.4 |
| Bilateral | 32 | 37.6 |
| Vertical position | Apical | 30 | 35.3 |
| Middle | 45 | 52.9 |
| Coronal | 10 | 11.8 |
| Superimposition | Superposition (+) | 46 | 54.1 |
| Superposition (-) | 39 | 45.9 |
| Sector position | 1.0 | 9 | 10.6 |
| 2.0 | 13 | 15.3 |
| 3.0 | 15 | 17.6 |
| 4.0 | 29 | 34.1 |
| 5.0 | 19 | 22.4 |
| Magnification | Magnification (+) | 61 | 71.8 |
| Magnification (-) | 24 | 28.2 |
| Angle classification (α) | α <65° | 66 | 77.6 |
| α >65° | 19 | 22.4 |
| True position assessed by CBCT | Palatial | 67 | 78.82 |
| Labial | 18 | 21.18 |
| Total | Total | 85 | 100.0 |
N: Number; α: Angle between IMC axis and occlusal plane; (+): positive; (-): negative; (%): percent
In this study, IMC location was predicted using five different prediction methods on OPGs by 25 volunteer dentists [Table/Fig-3]. The prediction methods used in this study were: a) the superimposition of the canine crown and root of the central incisor [9]; b) sector determination [12]; c) magnification [14]; d) angulation [18] and the combined method (decision-making by evaluating the four methods together) [Table/Fig-4]. Vertical level or the position of the IMC crown method was used as an adjunct to the magnification method [14].
Descriptive analysis of results of dentists in area of expertise and postgraduate experience.
| Area of expertise | N | Experience in dentistry (year) |
|---|
| Oral diagnosis and radiology | 5 | 5.50 |
| Orthodontics | 20 | 6.05 |
| Total | 25 | 5.92 |
N: Number
Methods for predicting the sagittal position of IMC as palatal or labial on OPG.

In superimposition method, if the IMC crown overlaps with the root or cervical part of the central incisor on OPGs, it can be assumed that this tooth is positioned palatally [9]. In sector determination method, location of canine cusp tip is evaluated on OPGs [12]. If the canine cusp tip corresponds to the deciduous canine (Sector 1), or corresponds to the distal aspect to the midline of the lateral incisor (Sector 2), or corresponds to the midline of the lateral incisor to the distal aspect of the central incisor (Sector 3) according to the sector location, the IMC is more likely located labially. If the canine cusp tip corresponds to, the distal aspect to the midline of the central incisor (Sector 4), the IMC is more likely mid- located in alveolus. If the canine cusp tip corresponds to the midline of the central incisor and to the midline of the maxillary arch (Sector 5), the IMC is more likely located palatally. In magnification method [14], the widest mesiodistal dimension of IMC crown is measured (a). At the same quadrant, the widest mesiodistal dimension of the central incisor crown is measured (c). Then the ratio of the widest mesiodistal dimension of the IMC to that of central incisor is defined as the Canine-Incisor Index (CII) (a/c). Vertical position of IMC crown was assessed relative to the adjacent erupted incisor, which was arbitrarily divided into three zones. The apical zone included the apical third of the root, and the middle zone consisted of the middle third of the root; the remainder of the root was classified as the coronal zone. If the crown of impacted canine positions in the middle third (M) or in the coronal third (C) of incisor root, the CII ranges between 1.15-1.7 for palatally impacted teeth. For buccally displaced teeth, the CII ranges between 0.78-1.11. In the angulation method [18], a horizontal line is drawn from the mesio-buccal cusp tip of the right and left maxillary first molars and the angle is measured between this horizontal line and long axis of the IMC. The inclination of the IMC (α) as measured lateral to the midline, is recorded in degrees. The angle greater than 65° shows labial location. The angle smaller than 65° shows palatal location. The combined method reflects the final prediction result of the volunteer by evaluating the four methods together [Table/Fig-4]. After the end of the prediction session, the prediction results were statistically compared with the true locations determined by CBCT. The five prediction methods were explained at the beginning and a written guide was given [Table/Fig-4]. The OPGs were evaluated separately by each volunteer and the computer, the darkroom environment conditions were set to be similar. The evaluation was requested to be performed in a maximum of three sessions with at least a two-week interval. The volunteer dentists recorded their prediction results for each IMC according to four methods separately and the dentists’ synthesised decision from these four methods constituted the fifth method: the "combined method". After the prediction session ended, answers of volunteer dentists were organised and prepared for statistical analysis. In each method, prediction results of volunteers for sagittal location of each IMC were compared with the true location, which was determined by CBCT. Then the correct predictions of 25 volunteer dentists for each IMC for a method were counted. The calculated percentage of correct answers for each IMC, for each method were used for the statistical assessment of method’s success. During the prediction of the sagittal location of IMC on OPG by each method, the requirement of "need for CBCT" had been answered with two-choice questionnaire (yes/no). In each method for each IMC, need for CBCT was questioned to 25 volunteer dentists. In each method for each IMC, positive answers were counted and the calculated percentage was used for statistical assessment. During the prediction of the location of the IMCs on the OPGs with different methods, “contentment with method” that reflects the method’s fulfilment of prediction and ease of use for volunteers were evaluated with Visual Analogue Scale (VAS) for each method. A straight horizontal line 100 mm- in length, oriented from the left (worst) to the right (best), was used for VAS method. With each method, volunteers reflected their own experience. The volunteers marked on the line, the point that they feel represented their perception of their current contentment with method. In each method for each IMC, mean value of VAS scores for the contentment with method of 25 volunteer dentists was calculated and used for statistical assessment.
First, frequency distributions of IMC samples used in this study were assessed. Then the success of prediction methods that were used by 25 volunteer dentists was assessed. The answers of questionnaire, which obtained during the prediction of sagittal location of each IMC with each method on OPG by 25 volunteer dentists, were also assessed.
Statistical Analysis
For statistical analysis, SPSS program (SPSS Statistics 20.0, Chicago, USA) was used. The similarities between each frequency distribution of impacted canines for methods and the true position by CBCT were examined by Kappa test. Positive Predictive Value (PPV), Negative Predictive Value (NPV), sensitivity, specificity was calculated with binary diagnostic test by means of cross-tabs. Reverse-angle (arcsine) transformation was applied to the correct answer, need for CBCT, and contentment with method data of the five prediction methods. Arcsine (inverse/angular) transformation stabilises variance and normalises proportional data. The use of arcsine transformation is useful in analysis of proportion data that tends to be skewed when the distribution is not normal. The Mann-Whitney U test for two independent groups, Kruskal-Wallis test when there were more than two independent groups and Friedman test when there were more than two dependent groups were used as non-parametric tests. The Bonferroni-Dunn test was used for the multiple comparison methods after the Kruskal-Wallis test, and the CF multiple comparison test was used after the Friedman test.
Results
On the panoramic radiograph, superimposition method has the highest PPV, magnification method has the highest NPV for predicting the location of IMC. Angulation method is the most sensitive predicting method, besides superimposition method is the most specific predicting method for detecting the IMC in palatal position [Table/Fig-5].
Validity of 3 predicting methods compared with true position in CBCT scans for the localisation of impacted canines.
| Superimposition | Magnification | Angulation |
|---|
| Positive predictive value | 0.96 | 0.90 | 0.86 |
| Negative predictive value | 0.41 | 0.50 | 0.47 |
| Sensitivity | 0.66 | 0.82 | 0.85 |
| Specificity | 0.89 | 0.67 | 0.50 |
| (Kappa) P | 0.381 | 0.443 | 0.347 |
Positive Predictive Value, probability that the palatal position is present when the test is positive; Negative Predictive Value, probability that the palatal position is not present when the test is negative; Sensitivity, probability that a test result will be positive when the palatal position is present (true positive rate); Specificity, probability that a test result will be negative when the palatal position is not present (true negative rate); Kappa< 0.20, poor agreement; 0.20 <Kappa < 0.40, fair agreement; 0.40 <Kappa <0.60, moderate agreement; 0.60 <Kappa < 0.80, good agreement; 0.80 <Kappa <1.00, very good agreement
The success of all five prediction methods for the sagittal location of IMCs was similar (p >0.05) [Table/Fig-6]. The highest mean rank values, related to need for CBCT, were found for the magnification and combined methods. The lowest values were found for the superimposition method (p<0.001). The highest contentment with method was for the superimposition method and the lowest contentment with method was for the magnification method (p<0.001).
Descriptive statistics, mean rank values and statistical analysis results of four methods according to correct answer, need for CBCT, and contentment with method in predicting the position of impacted canines evaluated by 25 volunteer dentists.
| | N | Mean | SD | Median (min-max) | Mean rank | p-value |
|---|
| Correct answer | Superimposition | 85 | 0.72 | 0.35 | 0.92 (0.00-1.00) | 3.19 | 0.117 |
| Sector | 85 | 0.70 | 0.36 | 0.92 (0.04-1.00) | 2.98 |
| Magnification | 85 | 0.72 | 0.25 | 0.84 (0.00-1.00) | 2.96 |
| Angulation | 85 | 0.67 | 0.34 | 0.88 (0.04-1.00) | 2.66 |
| Combined | 85 | 0.74 | 0.28 | 0.88 (0.04-1.00) | 3.20 |
| Need for CBCT | Superimposition | 85 | 0.34 | 0.16 | 0.32 (0.08-0.68) | 2.09 C | <0.001 |
| Sector | 85 | 0.37 | 0.17 | 0.36 (0.12-0.72) | 2.38 BC |
| Magnification | 85 | 0.50 | 0.17 | 0.52 (0.16-0.92) | 3.66 A |
| Angulation | 85 | 0.40 | 0.16 | 0.40 (0.08-0.71) | 2.80 B |
| Combined | 85 | 0.51 | 0.20 | 0.52 (0.12-0.84) | 4.06 A |
| Contentment with method | Superimposition | 85 | 0.62 | 0.08 | 0.63 (0.45-0.78) | 3.79 A | <0.001 |
| Sector | 85 | 0.60 | 0.09 | 0.60 (0.37-0.77) | 2.76 BC |
| Magnification | 85 | 0.56 | 0.09 | 0.54 (0.35-0.74) | 2.24 C |
| Angulation | 85 | 0.60 | 0.08 | 0.59 (0.44-0.76) | 3.08 BC |
| Combined | 85 | 0.60 | 0.08 | 0.59 (0.45-0.81) | 3.12 AB |
N: Number; SD: Std. deviation; Min: Minimum; Max: Maximum; Combined, decision-making by evaluating the four methods together; P, friedman test; (post-hoc, CF test), significance levels are indicated with letters; capital letters on the right side indicate significance levels of statistical differences
Vertical position and angulation differences of the IMCs did not affect the success of the prediction methods, need for CBCT and contentment with method (p>0.05). The success of the prediction methods were the highest in Sectors 1 and 5. Sector 3 is the worst area (p<0.01) [Table/Fig-7]. Need for CBCT was the highest and contentment with method was the worst for Sector 3.
Mean rank values and statistical analysis results of the effect of vertical position, sector location, and angle classification on each method according to correct answer, need for CBCT and contentment with method evaluated by 25 volunteer dentists.
| Vertical position | p-value | Sector position | p-value | Angle classification (α) | p-value |
|---|
| Mean rank | Mean rank | Mean rank |
|---|
| Vertical position | Sector | Classification |
|---|
| Apical | Middle | Cervical | Sector 1 | Sector 2 | Sector 3 | Sector 4 | Sector 5 | α <65° | α >65° |
|---|
| N=30 | N=45 | N=10 | N=9 | N=13 | N=15 | N=29 | N=19 | N=65 | N=20 |
|---|
| SuperpositionCorrect answer | 44.80 | 42.69 | 39.00 | 0.802 | 59.50 A | 22.15 C | 21.37 C | 44.60 B | 64.08 A | <0.01 | 45.09 | 36.20 | 0.153 |
| SuperpositionNeed for CBCT | 45.27 | 40.58 | 47.10 | 0.616 | 35.72 B | 51.12 B | 67.27 A | 45.03 B | 18.63 C | <0.01 | 42.45 | 44.80 | 0.708 |
| SuperpositionContentment with method | 41.13 | 45.19 | 38.75 | 0.663 | 45.89 B | 34.54 B | 16.30 C | 41.29 B | 71.11 A | <0.01 | 44.72 | 37.43 | 0.248 |
| SectorCorrect answer | 44.97 | 42.06 | 41.35 | 0.858 | 62.33 A | 25.46 C | 20.83 C | 43.09 B | 63.21 A | <0.01 | 45.15 | 36.00 | 0.143 |
| SectorNeed for CBCT | 43.72 | 41.41 | 48.00 | 0.732 | 32.44 C | 45.77 BC | 64.13 A | 52.40 B | 15.08 D | <0.01 | 43.31 | 42.00 | 0.835 |
| SectorContentment with method | 41.30 | 45.23 | 38.05 | 0.633 | 53.83 B | 41.15 BC | 17.87 D | 33.93 C | 72.82 A | <0.01 | 43.00 | 43.00 | 1.000 |
| Magnification Correct answer | 39.38 | 44.89 | 45.35 | 0.605 | 57.78 A | 32.62 B | 32.07 B | 46.10 AB | 47.00 AB | 0.050 | 41.06 | 49.30 | 0.191 |
| MagnificationNeed for CBCT | 47.38 | 43.50 | 27.60 | 0.087 | 31.50 | 47.00 | 55.10 | 38.22 | 43.45 | 0.134 | 44.55 | 37.98 | 0.296 |
| MagnificationContentment with method | 38.33 | 42.31 | 60.10 | 0.052 | 52.39 | 43.50 | 34.43 | 44.43 | 42.79 | 0.523 | 41.59 | 47.58 | 0.343 |
| AngulationCorrect answer | 41.43 | 46.02 | 34.10 | 0.347 | 45.89 AB | 29.5B B | 28.73 B | 43.62 B | 61.18 AB | 0.001 | 45.35 | 35.38 | 0.112 |
| AngulationNeed for CBCT | 45.82 | 41.03 | 43.40 | 0.711 | 21.28 D | 42.46 BC | 65.30 A | 47.36 BC | 29.39 CD | <0.01 | 46.30 | 32.28 | 0.026 |
| AngulationContentment with method | 39.65 | 44.82 | 44.85 | 0.652 | 62.22 A | 50.15 A | 20.13 C | 35.34 B | 58.74 A | <0.01 | 39.78 | 53.45 | 0.030 |
| CombinedCorrect answer | 44.15 | 43.92 | 35.40 | 0.580 | 54.72 AB | 22.58 C | 22.73 C | 45.60 B | 63.45 AB | <0.01 | 45.52 | 34.83 | 0.088 |
| CombinedNeed for CBCT | 45.57 | 41.86 | 40.45 | 0.767 | 23.17 C | 40.58 BC | 66.47 A | 47.45 BC | 28.74 C | <0.01 | 43.51 | 41.35 | 0.732 |
| CombinedContentment with method | 39.18 | 44.61 | 47.20 | 0.549 | 60.94 A | 46.77 AB | 16.70 C | 38.59 B | 59.42 A | <0.01 | 41.57 | 47.65 | 0.335 |
N: number; Combined, decision-making by evaluating the four methods together; (Vertical position and Sector position, P, kruskal Wallis test; (post-hoc, bonferonni-dunn test), significance levels are indicated with letters; capital letters on the right side indicate differences in terms of sectors); (Angle classification (α), P, Mann Withney U; (α) < 65°, palatally positioned impacted canine; (α) > 65°, labially positioned impacted canine
Discussion
Since CBCT is a 3-D imaging system, the relationship between IMC and neighbouring structures, the true location and accurate position of impacted teeth can be determined successfully with CBCT [22]. However, OPGs are used more frequently in the general evaluation of jaws and teeth by all dentists [23]. The orthodontist is more likely to detect palatal or labial location of the IMC with panoramic X-ray [24], as the most sensitive technique, followed by the occlusal and periapical X-ray [25]. Therefore, determination of safe zones for identifying the true sagittal location of IMC in OPG may reduce the use of CBCT in accordance with the ALARA principle [26].
In previous studies, it was reported that 75-85% of IMC localised palatally [9,19]. The present sample is in accordance with the reported percentages. Ethnicity could be the reason for different reports [10].
In this study, superimposition method has the highest PPV, which means that when the impacted canine crown overlaps with the root or cervical part of the central incisor, this IMC is mostly localised in the palatal region. Additionally, superimposition method is found more specific. In other words, when the IMC is located labially, superimposition method’s test result will be negative [Table/Fig-5]. According to the present study, 96% PPV was the highest score for detecting palatally located IMC with superimposition method. Therefore, “usage of superimposition method only as an adjunct to the other methods” [10] could not be accepted according to the present results. The angulation method is the most sensitive predicting method for detecting the IMC in palatal position [Table/Fig-5]. Briefly, when the IMC is located palatally, angulation of IMC will be smaller than 65° [Table/Fig-1b]. Superimposition, magnification and angulation methods are effective in predicting the location of palatally localised IMC in particular [Table/Fig-5] [16]. Owing to palatal canine displacement being much more frequent than labial displacement [27], easy diagnosis is enabled with these methods. The kappa values obtained in the study are similar to those of Wriedt S et al., [21]. Despite using OPG and additionally dental casts for predicting location in this aforementioned study [21], similar results have been obtained with the present study. Using five different methods for predicting in the present study could be the reason of this similarity.
Twenty-five volunteer dentists predicted the sagittal locations as “palatal” or “labial” using five different prediction methods. The success was similar [Table/Fig-6]. The percentage of correct answers in the present study ranged from 67% to 74%, that was within the similar level (66%-94%) with literature [9-14,16-18,21,28]. In this study, only palatally or labially located IMCs were included, and prediction of one of these two locations was requested. In general, probability of an event is the ratio of the number of observations of the event to the total number of observations. In the present study, the probability of being in palatal or labial location for an IMC was half. This means that the probability of predicting IMC as palatal or labial without using the prediction methods is 50%. The highest correct answer percentage obtained in this study was 74%. However, the possibility of correct tooth location prediction is 50% without using location prediction methods. Therefore, it is unfortunately not possible to report that the correct answer results of prediction methods were successful. According to the results of the study, the success rate of the prediction methods is lower than that of the CBCT [21]. This is in agreement with the Kappa test results obtained in the present study. Contradictorily, Chaushu S et al., and Chalakkal P et al., stated that the magnification method, which is performed on OPGs, is adequate for initial assessment of canine location [14,28]. Methodological differences, as that study focused only on the palatally placed tooth, could be the reason for these divergent results.
The highest need for CBCT was found for the combined method, followed by the magnification method. The combined method not only was a decision-making by evaluating the other four methods together, but also reflected the final decision of the dentists. In the superimposition method, need for CBCT was lowest. The highest PPV and increased specificity for superimposition method [Table/Fig-5] that were obtained in the present study can explain the lesser demand by dentists for need for CBCT using this prediction method. This finding was also similar in contentment with method results [Table/Fig-6]. The dentists were less satisfied with magnification method and the need for CBCT was the highest. In the study, dentists evaluated OPGs in JPEG format on computer and no milimetric or angular measurements were done. Perhaps evaluating OPGs one after another with a quick decision by eye without measuring, causes dentists to lack confidence in using the magnification method [Table/Fig-6]. The validation results were obtained for superimposition, magnification and angulation methods. Because of the angulation and sector method had two or more than two positions, the sector method had been evaluated with Kruskal Wallis test and the angulation method had been evaluated with Mann-Withney U test.
The results of this study show that the difference in vertical level of the impacted tooth on OPG has no effect on likelihood of a correct answer data, need for CBCT, or the contentment in each method [Table/Fig-7]. It has been reported in the literature that the vertical level and the rotation of the implanted tooth had a negative effect on the success of this method. Especially, sagittal location of IMC in the apical zone cannot be determined by this method [14,17]. Rotated teeth were excluded from the present study. However, difference in vertical level did not affect the mean ranks of correct answers [11]. Opposite results [14,17] may arise from the methodological differences.
Differences in sector location affected the prediction method’s success. Volunteers correctly predicted the true locations of IMCs that were in Sector 1 and in Sector 5 in all methods. This finding is in agreement with the literature [9,12]. Need for CBCT was lower, and contentment with method was higher for these sectors. Sector 5 surrounds an area where IMC crowns are closer to the midline and overlapped with the root of central incisor. Labially located IMCs are less likely to approach to the midline due to insufficient bone thickness in the vestibule, regardless of the vertical level. Additionally, images of the labially located IMC move in the same direction as the tube and can be projected onto apex of lateral incisor in OPG [29,30]. Although both Sector 4 and Sector 5 surround an area in which IMC crowns overlapped with the root of central incisor, Sector 5 is a safer zone in the diagnosis of palatinally located IMCs [9,12]. Sector 1 encompasses the area of deciduous canine teeth. Palatally IMCs often move closer to the midline due to insufficient guidance by lateral incisor. However, this is not possible for labially located teeth due to insufficient bone thickness. Thus, the farthest area from the midline is expected to be a safer zone for the diagnosis of labially impacted teeth [12].
Because of the technique of obtaining radiographs, the image of labially IMC crown is projected onto apex of lateral incisor in OPG [29,30], and both palatally and labially located IMCs can localise in Sector 3. Therefore, Sector 3 is the most complex area to diagnose the sagittal location, and in the present study the highest CBCT requirement and the worst contentment with method level was revealed for this area [Table/Fig-7].
The difference in angle between impacted tooth axis and occlusal plane above or below 65° has no effect on likelihood of correct answer, additional diagnostic request, or satisfaction with each method [Table/Fig-7]. Quick decision by eye without measuring the angle during prediction by the volunteer dentists or need for improvement to the angulation method could be the reasons of this result. This is because, when the labially located IMC are at apical level and in horizontal position, the angle between the tooth axis and the occlusion plane may decrease, contrary to the angulation method. An S et al., reported that many actually labially located IMCs were predicted in palatal location according to angulation method [10].
Limitation
In this study, only a single OPG was used for determining the sagittal location of IMC. In the future, adding other diagnostic tools as occlusal, periapical and/or cephalometric radiographs, dental casts during prediction could increase the accuracy of prediction.
Conclusion
The prediction methods used in this study were more successful in predicting palatally localised IMC on OPGs. The success of the methods used to predict the true location of IMC on OPG is similar. The lowest need for CBCT and the highest contentment with method were found for the superimposition method. Clinicians can predict the sagittal location of IMC’s with high accuracy on OPG where the IMCs are in Sector 1 (canine cusp tip corresponds to the deciduous canine) and Sector 5 (canine cusp tip corresponds to the midline of the central incisor) areas. On the other hand the sagittal location of IMCs that are placed in Sector 3 should be examined carefully with CBCT, which is the most complex area to predict the location of IMC on OPG.
N: Number; α: Angle between IMC axis and occlusal plane; (+): positive; (-): negative; (%): percent
N: Number
Positive Predictive Value, probability that the palatal position is present when the test is positive; Negative Predictive Value, probability that the palatal position is not present when the test is negative; Sensitivity, probability that a test result will be positive when the palatal position is present (true positive rate); Specificity, probability that a test result will be negative when the palatal position is not present (true negative rate); Kappa< 0.20, poor agreement; 0.20 <Kappa < 0.40, fair agreement; 0.40 <Kappa <0.60, moderate agreement; 0.60 <Kappa < 0.80, good agreement; 0.80 <Kappa <1.00, very good agreement
N: Number; SD: Std. deviation; Min: Minimum; Max: Maximum; Combined, decision-making by evaluating the four methods together; P, friedman test; (post-hoc, CF test), significance levels are indicated with letters; capital letters on the right side indicate significance levels of statistical differences
N: number; Combined, decision-making by evaluating the four methods together; (Vertical position and Sector position, P, kruskal Wallis test; (post-hoc, bonferonni-dunn test), significance levels are indicated with letters; capital letters on the right side indicate differences in terms of sectors); (Angle classification (α), P, Mann Withney U; (α) < 65°, palatally positioned impacted canine; (α) > 65°, labially positioned impacted canine