Introduction
There is a substantial amount of literature on electrical nerve stimulation for xerostomia, which includes both intra as well as extra oral techniques that has been used so far. A systematic review would provide a wide knowledge about the use of electrical stimulation as a treatment for xerostomia patients.
Aim
To provide a detailed report on the original research in field of electrical nerve stimulation used as a therapy for patients with xerostomia.
Materials and Methods
The primary database used was Medline (via PubMed) and Cochrane Central Register of Clinical Trials (CENTRAL). The article selection was carried out by two authors in order to avoid bias. Eligibility criteria for the studies were: it should be an original research, patients with xerostomia and the patients should have undergone any type of electrical nerve stimulation intervention. The finalised list of studies meeting the inclusion criteria was assessed for data extraction. A total of 11 studies was included after thorough verification of the guidelines and inclusion criteria.
Results
A total of 10 of the studies reported to show increase in the salivary flow on application of electrical stimulation for those patients with dry mouth irrespective of the aetiology. However high quality studies (i.e., detail recording of the history of dryness, onset, severity etc.,) with more precision about the impulse used and patient details is required for evaluating the effectiveness of the device to be used as an adjuvant treatment. Overall the results observed from this systematic review are that, the use of electrical nerve stimulation technique for treatment of xerostomia is a suitable modality as it is widely accepted by the patients, is a non-invasive procedure and has little or no adverse effects.
Conclusion
Electrostimulation is an effective way of triggering reflex salivary stimulation even in a partially atrophied gland or hypo secretion irrespective of its aetiology. The benefits being ease of usage and the acceptability of the patients among the current devices as it is noninvasive makes it an ideal therapeutic device for treating xerostomia.
Electrical stimulation, Hyposalivation, Mouthdryness
Introduction
The prime role of saliva is lubrication, protection and defense of the oral cavity. Saliva has digestive functions as it moistens the food bolus which can be swallowed easily. Salivary amylase breaks down starch into maltose and dextrin, thus, the digestion commence in the oral cavity even before it reaches the stomach. Xerostomia, in general terms known as dry mouth, is reduced salivary flow rate along with change in composition of saliva [1]. The rationale of this review is to provide a complete systematic review on the non-pharmacological treatment modalities that has been intervened over the years. This is first of its kind to report a systematic review on this topic. Several studies have been published in literature showing the use of nonpharmacological techniques to treat xerostomia. One of the most common issues faced by the geriatric population is dryness of the oral cavity. The prevalence rate is about 10 to 29%, with a female predominance [2]. With age there is definite change in the morphology and function of salivary glands. Major local causative factors of xerostomia include Sjogrens syndrome, dysfunction of the salivary gland, radiation therapy to head and neck cancer patients. Other nonspecific local causes are mouth breathing, nasal destruction, stress anxiety, smoking. Systemic conditions that affect the salivary gland functions include auto immune disease (Acquired immune deficiency syndrome, Systemic Lupus Erythymatosis, rheumatoid arthritis, scleroderma), neurological disorders and psychological illness (depression, drug abuse). Sjogrens syndrome is the most common disease affecting the salivary gland with an occurrence rate of 0.1% to 4.8% presenting as primary or secondary sjogrens. Primary Sjogrens syndrome involves dry eyes and mouth, not associated with any other illness. Secondary Sjogrens includes the presence of other autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus etc., [3]. Drugs that cause xerostomia are diuretics (Chlorothiazide, Hydrochlorothiazide), antihistaminic agents (Clemastine), bronchodilators (B2-Adrenomimetics, Inhalatory Glucocorticoids, Inhalatory Cholinolytics), cholinolytic agents (Atropine, Homatropine, Scopolamine) etc. Xerostomia majorly affects the patients dietary habits, speech, taste, tolerance to dental prosthesis and increased susceptibility to dental caries [4]. Signs of xerostomia are dry, cracked peeling lips, dry and course tongue, cracks in corners of the mouth, mucositis, oral candidiasis, ulcers etc. The symptoms which patient experience are difficulty in swallowing and chewing dry food substances, burning sensation, lack of taste perception, coughing episodes, speech difficulties, nocturnal discomfort, increased liquid intake etc. Other conditions which mimic the signs of xerostomia are stress, anxiety, smoking tobacco, using marijuana, tranquilisers, botulism poisoning. Numerous treatment strategies have been attempted for treating patients with xerostomia like the use of lubricants (mineral oil, vegetable oil etc.,) and salivary substitutes (oral spray-Oasis mouth moisturising spray, saliva replacement gel, moiturising gel-Biotene Oral balance, paste, aerosol-Aquoral etc.,) when the treatment is interrupted or discontinued the symptoms recur. The primary cause for xerostomia needs to address because xerostomia can also occur due to polypharmacy, sicca syndrome, celiac disease or it could be due to mere stress. Most widely used drug for treatment is Para sympathomimetic, muscarinic agonist such as such as Pilocarpine (“SALAGEN” 5 milligrams (mg) three or four times a day) and Cevimeline (“EVOXAC” 30 milligrams three times a day) but has its own adverse effects (trembling, headache, diarrhoea, stomach cramps etc.,). Pharmacological treatment for xerostomia provides only symptomatic relief once the medications are discontinued the symptoms recur. Non pharmacological interventions increase the salivary flow rate and improve the symptoms related to xerostomia. In order to overcome the drawbacks of earlier mentioned treatment modalities, Transcutaneous Electrical Nerve Stimulation (TENS) was advocated as an alternative treatment choice owing to its stimulatory effect on the salivary flow caused due to the release of endorphins in the opiate receptors [5]. Apart from TENS other non-pharmacological treatment modality for xerostomia includes the use of low level laser therapy (A diode laser (780 nm, 3.8 J/cm2, 15 mW to irradiate the parotid, submandibular, and sublingual glands) [6]. TENS is non-invasive and it has been used over the years for pain management in oro facial region and temporomandibular joint disorders. TENS is the use of electric current delivered via specific device for therapeutic purposes. It produces electrical impulses which can be adjusted for frequency, pulse and intensity. In dentistry TENS has been widely used for treating oro facial pain and temporomandibular joint disorders [7]. In the past, numerous studies have been done for evaluating the effect of electrical nerve stimulation on the salivary flow of xerostomia patients [8-17]. Fedele S et al., reported a review on TENS for xerostomia patients [18]. This systematic review is a compilation of the available evidences of the utility of electrostimulation for treating xerostomia patients. Electrostimulation has been a treatment option for xerostomia and has been under research from early 1988 [19]. Literature reports majority of the studies have proven increase in salivary secretion with the use of TENS regardless of the aetiology [8,10,13,14]. This complication would help the clinicians to get an overall knowledge and clear-cut understanding about the application and advantages of using electrostimulation therapy for xerostomia patients.
Materials and Methods
Eligibility Criteria
In this review we included only patients with xerostomia (due to any aetiology) and having undergone any form of Transcutaneous electrical nerve stimulation therapy. Most of the studies used normal population (healthy subjects) as control. All the studies included were of interventional type. The search included studies and case report from Electronic search results which were consolidated and duplicates were removed. All study titles were reviewed and those which were not eligible were eliminated. No specific exclusion criteria were set due to very few availability of research in this field. Reference list of all the eligible studies were reviewed to find out appropriate studies which were missed by the electronic search. All the eligible studies were on adult (more than 18 years) participants and all the reports were in English.
Information Sources
The primary database used were Medline (via Pubmed) and Cochrane Central Register of Controlled Trials (CENTRAL).
Literature Search
The search was started on May 2018 and completed on 15 June 2018, studies included were between the period 1986 to 2016 and only studies published in English language were included for this systematic review. MeSH terms used were Nerve stimulation or Electrical stimulation AND xerostomia. Furthermore the search was supplemented by hand searching of relevant references from selected articles and other eligible studies which met the inclusion and exclusion criteria were also included.
Data Collection and Review Process
The finalised list of studies meeting the inclusion criteria was assessed for data extraction. Tabulation of the citation information was done which included the objective, participants, intervention, location, outcome, limitations, side effects and discussion.
Synthesis of Results
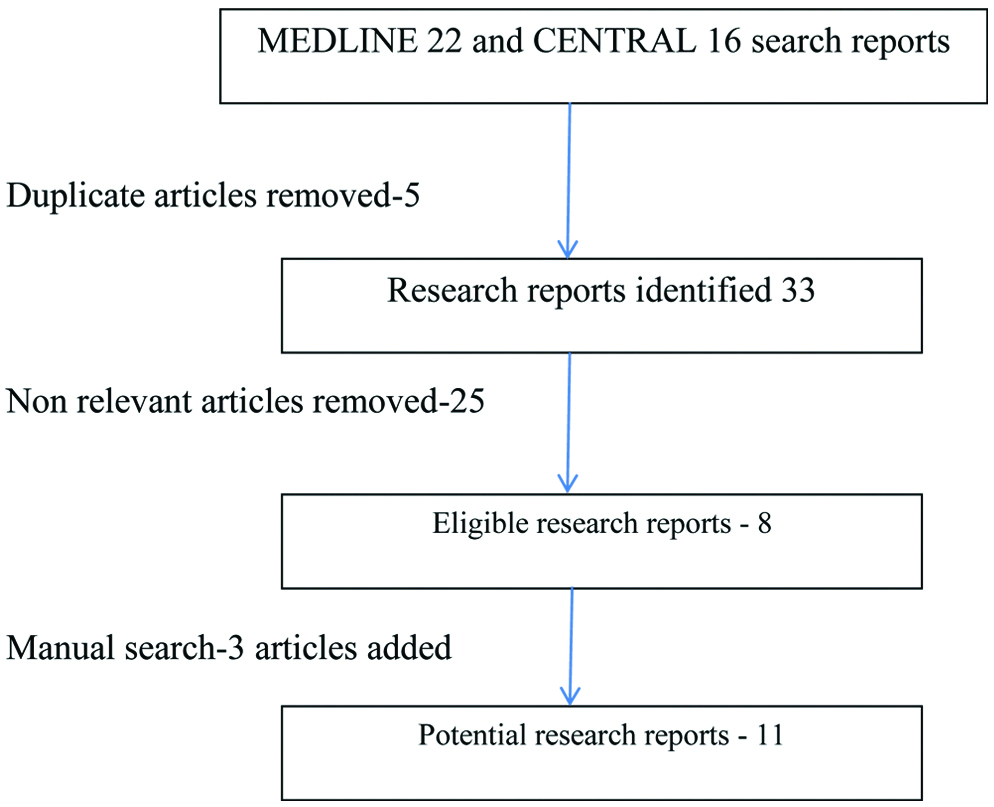
Study selection: Initial search from MEDLINE and Cochrane Central Register of Controlled Trials (CENTRAL) gave 22 and 16 articles, respectively. Duplication (5) and irrelevant articles (25, after reading the abstract) were removed. Finally, a total of 8 articles were identified. The abstracts of the articles were reviewed to check the inclusion criteria. Additionally 3 more articles were added based on manual search from the back reference of these 8 articles which were selected from the title screening. In order to check and reconfirm the eligibility all these 11 articles were read entirely. [Table/Fig-1] shows the literature search methodology.
Flow chart of literature search methodology.
Study Characteristics
For all the studies the main objective, participants included, intervention done, site of intervention, the outcome and the limitations were analysed.
[Table/Fig-2] shows the results of individual studies [8-17,20].
Tabulation of the results of all studies included in the systematic review [8-17,20].
| S. No. | Author | Objective | Participants | Intervention | Location | Outcome | Limitations and side effects |
|---|
| 1. | Weiss WW et al., [15] | To treat xerostomia patients through normal physiogic mechanisms with a device that provides electrical stimulation to oral and pharyngeal afferent nervous system | Rabbit oral mucosa24 xerostomia patients(11 active 13 placebo) | Rabbit oral mucosa (to ensure safety)-anaesthetized and stimulated 3 min for varying Volts (5 to 40V)40V-3,6,12,24 min24 xerostomia pts11 active 13 placebo (3 stimulations, 3 weeks). | Dorsum of the tongue | 20% slight improvement50%-moderate improvement30%-substantial improvement | No evidence of saliva collection prior to the use of device |
| 2. | Steller M et al., [8] | Determine whether an electrical stimulusapplied to the tongue and hard palate by a battery-operateddevice could stimulate salivary flow in subjectsWith generally severe Sjogren’s syndrome . | Total 29 patients with Sjogren’s syndrome14-Active 15-Placebo | Week 0-saliva collectedSubjects used the device at home three times a day. morning, afternoon, and evening, and recorded the time of day and intensity setting after each use.Week 2&4-saliva was collected post stimulation | Oral mucoosa0-10 (max intensity was used) | Increase post stimulation saliva in active group (mainly due to 3 patients in the group) | No response from patients with low/Nil whole salivaFew contraindications and effect of long term use is unknown |
| 3. | Talal N et al., [14] | To evaluate the ability to increase the production of saliva and reduce clinical symptomatology. | 77 Sjogren’s syndrome patients40-active device37-placebo device | The patient was instructed to place the probe electrodes at the midline of the tongue, about 3/4 inch from the tip, then press the tongue up to the roof of the mouth, positioning the electrodes between the tongue and the roof of the mouth. Shut off after 3 min.3 times a day for 4 weeks | Middle of the tongue | Whole saliva flow rates measured at weeks 0, 2 and 4 by collection of whole saliva before and after stimulation | Few patients-no response for active device |
| 4. | Hargitai IA et al., [17] | To assess the effectiveness of transcutaneous electric nerve stimulation (TENS) as a means of stimulating salivary function in healthy adult subjects. | 22 healthy patients | Unstimulated saliva was collected then activation with TENS later stimulated saliva was collected for 5 min | TENSelectrode pads were placed externally on the skin overlying the parotid glands | Increase in salivary flow rate | Size of electrodes were large which caused twitching of facial musculature in few cases |
| 5. | Strietzel FP et al., [9] | Evaluate the safety and effectiveness of a recently developed electrostimulating device mounted on an individualised intra oral removable device | 20 patients with xerostomia | Total 100 experimentsEach patient-10 experimentPrior to experiment-Blood pressure and heart rate was checkedExperiment-one active stimulation and one sham test (random order)5 min and 10 min experiment was carried out-compared both with oral dryness and ans were the questionnaire. | Customised try-electrodes were placed close to the lingual nerve. | Good reponse to the electrostimulation | Erythema was observed in the oral mucosa.Active and sham exot were randomised-patients memory was an influence on the feedback |
| 6. | Ami S and Wolff A, [10] | To evaluate the effect of Saliwell Crown device on an implant placed in the lower third molar area | 81-year-old Female with xerostomia | The device, named SaliwellGenNarino (Saliwell Ltd., Harutzim, Israel), is a removable appliance, combining microelectronics, software, and wireless communication, and applies stimulating signals on the lingual nerve, leading to enhanced salivary secretion. | Lower third molar area-mounted on a commercially available dental implant | Constant slight but significant increase in the salivary secretion and in the patient’s personal feelings as presented in the questionnaires. | Has to be customised for each patient |
| 7. | Strietzel FP et al., [11] | To evaluate the efficacy and safety of an intraoral electrostimulation device, consisting of stimulating electrodes an electronic circuit, and a power source, in treating xerostomia. | Xerostomia due to Sjogren’s Syndrome(n=114) | Stage 1-double blinded crossover (active and sham device used for 1 month)Stage 2-3 month open label stage, asses the long term effects of active device | Casted individually to fit the mandibular dental arch and an infrared remote control.Elctrodes contact the oral mucosa in mandibular third molar area, proximity to lingual nerve.Patient advised to use not more than once in an hour(except this any no. of times they wish to) | Pri end point-improvement in severity of xerostomiaSec end point-(improvements in the other symptoms, increased salivary output, and event-free use | 27% oral mucosal lesions (erythema, apthae)No explanation for Drop out patients (9) |
| 8. | Wong RK et al., [12] | Assess the feasibility and preliminary efficacy of acupuncture-like transcutaneous electrical nerve stimulation (ALTEN) in reducing radiation-induced xerostomia | Patients with Head and Neck Cancer-received radiation therapy±chemo (less than 2 yrs from the time of study)Placebo-(not possible to use ALTENS(n=48) | Acupuncture points were utilised, each was stimulated 10 sec at a time-24 sessions for 12 weeks (not to exceed 3/week) | LI4 • He Gu • Large Intestine 4SP6 • San Yin Jiao • Spleen 6ST36 • Zu San Li • Stomach 36CV24 • Cheng Jiang Conception Vessel 24 | ALTENS appears to be well tolerated without significant toxicities. | 5 patients-gastrointestinal toxicity1 patients-facial pain |
| 9. | Vijayan A et al., [13] | To evaluate the effectiveness of TENS delivered using an extraoral device in patients with radiation induced xerostomia | 30 patientsPost radiation therapy | TENS-5 min 50 Hz | Placed external on the skin, 1 cm in front of the tragus of the ear | Improved salivary flow rate | Saliva collection prior to start of treatment was not done.No major side effects |
| 10. | Lakshman AR et al., [16] | Evaluate the effectiveness of a Transcutaneous Electrical Nerve Stimulation (TENS) unit in stimulating the whole salivary flow rate in radiation induced xerostomia patients. | Total-40 patientsSI-20S1A-10(underwent Head & Neck radiotherapy with TENS during the commencement of radiotherapyS1B (n=10) full course of radiotherapyControl-10 healthy individuals | TENS activated and saliva collected for 10 minsS1 and S1A-3rd, 6th week and after a month of completion of radiotherapyS1B-stimulation daily, full course of radiotherapy | Electrodes were placed externally on the skin overlying the parotid glands | Intially the comparison between Stimulated and unstimulated salivary flow rate was non significant. 3rd and 6th week-significant | Not effective in those patients with absolute absence of saliva |
| 11. | Ojha S et al., [21] | To determine the effectiveness of transcutaneous electrical nerve stimulation (TENS) in stimulating salivary flow in post radiated oral cancer patients, and to compare the salivary flow rate between unstimulated saliva and saliva stimulated with TENS in post-radiated oral cancer patients. | 30-patients who underwent radiation for oral cancer | Unstimulated saliva was collected then activation with TENS later stimulated saliva was collected for 5 min | The surface electrode pads were placed externally on the skin overlying the parotid, submandibular, and sublingual glands | Increase in salivary flow rate | Mild twitching of the facial musculature |
Discussion
The purpose of this systemic review was to compile all the studies related to electrical nerve stimulation on salivary flow so that it serves better understanding about this intervention. Also, further this method could serve as an effective treatment method for xerostomia, because all the other currently available treatment options provide only an intermittent relief and persist upon discontinuation. Other drugs (pilocarpine or cevimeline) that are widely used are not advised because of their own side effects.
Numerous causes have been reported which includes drugs, radiation therapy to the head and neck, salivary gland pathology like Sjogrens syndrome etc. Consequences of xerostomia vary from mild to severe in few cases. It also has major effect on the quality of life of the patient affecting the speech, swallowing of food, leads to dental caries and infection [21]. Despite affecting the quality of life of the patients it also interferes with the outcome of few dental treatments. Hence the dentist should be aware of the treatment as it is challenging for him. Several treatments are available, like lubricants or salivary substitutes. These provide only an intermittent relief and persist upon discontinuation.
Electrical nerve stimulation for xerostomia patients has reported to increase production of saliva and reduce the symptoms of the patients with dry mouth [10]. In most of the studies the stimulation is applied for the patients through the oral mucosa while in few studies on the skin covering the salivary glands. In cases of devices wherein the stimulation is intraoral i.e., through the oral mucosa, the impulse generated is carried to the salivary nuclei in the medulla oblongata from where the signals are directed to efferent part of the reflex leading to salivation. Intraorally, the electrodes are usually cotton rolled electrodes, clamp electrodes or adhesive electrodes. The electrodes are adapted to the oral mucosa. The most commonly used are the adhesive electrodes as they are very flexible and thin, hence they adapt well to the mucosal surface of the oral cavity. Intraoral TENS stimulates the oral mucosa on afferent neuronal receptors and pathways thereby increasing salivary production.
The effective and permissible dosage of frequency would be 50-80 H2, which is considered to be safe above the head and neck region. This dosage is effective to stimulate saliva when used for about 5-10 minutes for about twice or thrice a day.
Electrodes placed extra orally are of two types: 1) Tin plate or aluminium electrodes; 2) carbon impregnated silicone rubber electrode. Usually, the extra oral electrodes are placed in the parotid region, coupled to the skin surface with the use of electrical conductivity gel. TENS placed over the parotid gland directly stimulates the auriculotemporal nerve that supplies secretomotor drive to the parotid gland. It is believed that afferent nerves transmit such impulses to the salivary nuclei (salivation center) in the medulla oblongata which consequently directs signals to the efferent part of the reflex leading to initiation of salivation. Overall from this systemic review evidences show that both intraoral and extraoral devices have the potential to increase the salivary flow in patients with xerostomia. However, the most preferred and easy to use with patient compliance is extra oral device.
The main center for regulation of saliva secretion is autonomic nervous system. Increase in saliva production is due to the parasympathetic nervous system while the sympathetic system decreases their production. In xerostomia, there is a marked decrease in the salivary flow rate and alteration in the salivary composition [22].
From the compilation of literature available, there is little or no effect in saliva stimulation, as reported by few studies. The size of the electrode should be taken into major consideration as it leads to twitching in few cases. In case of inta-oral TENS customization for each patient is a major limitation.
A meta-analysis of electrical nerve stimulation for xerostomia has been reported however very few studies have been compiled under the review [7]. Overall, from this systematic analysis we infer that electrostimulation is an effective way of triggering reflex salivary stimulation even in a partially atrophied gland. The benefits being ease of usage and the acceptability of the patients among the current devices as it is non-invasive.
Limitation
One of the major limitation of this systematic review is the limited number of original research in this topic of concern. Hence conclusion drawn has limitations. Probably a broader approach to this area of research should have ideally been taken into consideration.
Conclusion
This review provides a detailed systematic analysis of the various approaches for both intra oral as well as extra oral electrostimulation which is an effective way of triggering reflex salivary stimulation even in a partially atrophied gland. It is well accepted by the patients as it is non-invasive and easy to use.
Proper stratification of the onset of oral dryness should be done in future studies so that it would help in understanding the treatment response better. (To analyse if the less affected glands respond better). Studies can also implement the documentation of patient acceptance in the form of questionnaire. One vital suggestion is to reduce the size of electrodes in the TENS equipment so that even the minimal side effect of tingling sensation can be overcome. Studies can be done to compare the usefulness of electrical stimulator alone as a treatment and also combination with other sialogogues.
[1]. Pinna R, Campus G, Cumbo E, Mura I, Milia E, Xerostomia induced by radiotherapy: an overview of the physiopathology, clinical evidence, and management of the oral damageTherapeutics and Clinical Risk Management 2015 11:17110.2147/TCRM.S7065225691810 [Google Scholar] [CrossRef] [PubMed]
[2]. Porter SR, Scully C, Hegarty AM, An update of the etiology and management of xerostomiaOral Surg Oral Med Oral Pathol Oral Radiol Endod 2004 97:28-46.10.1016/j.tripleo.2003.07.010 [Google Scholar] [CrossRef]
[3]. Cooke C, Ahmedzal S, Mayberry J, Xerostomia-a reviewPalliative Medicine 1996 10(4):284-92.10.1177/0269216396010004038931063 [Google Scholar] [CrossRef] [PubMed]
[4]. Sarapur S, Shilpashree HS, Salivary Pacemakers: a reviewDent Res J 2012 9(Suppl 1):S20-S25. [Google Scholar]
[5]. Daniels B, McNally M, Matthews D, Sketris I, Hayden JA, Management of Xerostomia in older adults: A systematic reviewJournal of Pharmacy Technology 2013 29(1):13-22.10.1177/875512251302900104 [Google Scholar] [CrossRef]
[6]. Pavlić V, The effects of low-level laser therapy on xerostomia (mouth dryness)Med Pregl 2012 65(5-6):247-50.10.2298/MPNS1206247P [Google Scholar] [CrossRef]
[7]. Sivaramakrishnan G, Sridharan K, Electrical nerve stimulation for xerostomia: A meta-analysis of randomised controlled trialsJ Tradit Complement Med 2017 7(4):409-13.10.1016/j.jtcme.2017.01.00429034187 [Google Scholar] [CrossRef] [PubMed]
[8]. Steller M, Chou L, Daniels TE, Electrical stimulation of salivary flow in patients with Sjögren’s syndromeJournal of Dental research 1988 67(10):1334-37.10.1177/002203458806701017013262637 [Google Scholar] [CrossRef] [PubMed]
[9]. Strietzel FP, Martín-Granizo R, Fedele S, Lo Russo L, Mignogna M, Reichart PA, Wolff A, Electrostimulating device in the management of xerostomiaOral Diseases 2007 13(2):206-13.10.1111/j.1601-0825.2006.01268.x17305624 [Google Scholar] [CrossRef] [PubMed]
[10]. Ami S, Wolff A, Implant-supported electrostimulating device to treat xerostomia: a preliminary studyClinical Implant Dentistry and Related Research 2010 12(1):62-71.10.1111/j.1708-8208.2009.00180.x19681934 [Google Scholar] [CrossRef] [PubMed]
[11]. Strietzel FP, Lafaurie GI, Mendoza GR, Alajbeg I, Pejda S, Vuletić L, Efficacy and safety of an intraoral electrostimulation device for xerostomia relief: a multicenter, randomized trialArthritis & Rheumatism 2011 63(1):180-90.10.1002/art.2776620882668 [Google Scholar] [CrossRef] [PubMed]
[12]. Wong RK, James JL, Sagar S, Wyatt G, Nguyen-Tân PF, Singh AK, Phase II results of RTOG 0537: A Phase II/III study comparing acupuncture-like transcutaneous electrical nerve stimulation versus pilocarpine in treating early radiation-induced xerostomiaCancer 2012 118(17):424410.1002/cncr.2738222252927 [Google Scholar] [CrossRef] [PubMed]
[13]. Vijayan A, Asha ML, Babu S, Chakraborty S, Prospective phase II study of the efficacy of transcutaneous electrical nerve stimulation in post-radiation patientsClin Oncol 2014 26(12):743-47.10.1016/j.clon.2014.09.00425262845 [Google Scholar] [CrossRef] [PubMed]
[14]. Talal N, Quinn JH, Daniels TE, The clinical effects of electrostimulation on salivary function of Sjögren’s syndrome patientsRheumatol Int 1992 12(2):43-45.10.1007/BF00300975 [Google Scholar] [CrossRef]
[15]. Weiss WW, Brenman HS, Katz P, Bennett JA, Use of an electronic stimulator for the treatment of dry mouthJournal of oral and maxillofacial surgery 1986 44(11):845-50.10.1016/0278-2391(86)90219-33490558 [Google Scholar] [CrossRef] [PubMed]
[16]. Lakshman AR, Babu GS, Rao S, Evaluation of effect of transcutaneous electrical nerve stimulation on salivary flow rate in radiation induced xerostomia patients: a pilot studyJ Cancer Res Ther 2015 11(1):229-33.10.4103/0973-1482.13800825879367 [Google Scholar] [CrossRef] [PubMed]
[17]. Hargitai IA, Sherman RG, Strother JM, The effects of electrostimulation on parotid saliva flow: a pilot studyOral Surg Oral Med Oral Pathol Oral Radiol Endod 2005 99(3):316-20.10.1016/j.tripleo.2004.06.08015716838 [Google Scholar] [CrossRef] [PubMed]
[18]. Fedele S, Wolff A, Strietzel F, López RM, Porter SR, Konttinen YT, Neuroelectrostimulation in treatment of hyposalivation and xerostomia in Sjögren’s syndrome: a salivary pacemakerJ Rheumatol 2008 35(8):1489-94. [Google Scholar]
[19]. Thorselius I, Emilson CG, Osterberg T, Salivary conditions and drug consumption in older age groups of elderly Swedish individualsGerodontics 1988 4(2):66-70. [Google Scholar]
[20]. Ojha S, Bhovi TV, Jaju PP, Gupta M, Singh N, Shrivastava K, Effectiveness of transcutaneous electrical nerve stimulation on saliva production in post-radiated oral cancer patientsJournal of Indian Academy of Oral Medicine and Radiology 2016 28(3):24610.4103/0972-1363.195664 [Google Scholar] [CrossRef]
[21]. Tanasiewicz M, Hildebrandt T, Obersztyn I, Xerostomia of various etiologies: a review of the literatureAdv Clin Exp Med 2016 25:199-206.10.17219/acem/29375 [Google Scholar] [CrossRef]
[22]. von Bültzingslöwen I, Sollecito TP, Fox PC, Daniels T, Jonsson R, Lockhart PB, Salivary dysfunction associated with systemic diseases: systematic review and clinical management recommendationsOral Surg Oral Med Oral Pathol Oral Radiol Endod 2007 103:S57-e1.10.1016/j.tripleo.2006.11.01017379156 [Google Scholar] [CrossRef] [PubMed]