Introduction
Family planning is a proven and cost-effective health intervention. Use of contraception has been reported to be low in developing countries.
Aim
To determine the trend of acceptance of contraception and the preferred methods of modern contraception in the new fertility research unit of Usmanu Danfodiyo university teaching hospital Sokoto, Nigeria.
Materials and Methods
This was a 10-year retrospective study involving all acceptors of modern contraceptive methods from the January 2008 to the December 2017. All case notes and theatre records were accessed. The data extracted were analysed using IBM SPSS version 23.0. Data were analysed using frequencies and percentages. Chi-square test was used for associations and level of significance was set at p<0.05.
Results
There were 11,577 acceptors of family planning during the study period. Of these 5762 were new acceptors. There were 30,721 deliveries. The contraceptive prevalence rate and annual acceptor rate were 18.8% and 576.2 per annum respectively. There was a steady rise in the number of acceptors over the years of study. All the clients were female and married. The housewives constituted 78.4% (4487) of the clients and (59.7%) of them had completed secondary level of education. The Implanon® was the preferred contraceptive method of choice in 2698 (46.%) of the new clients Jadelle® was next with 942 (16%) clients using it.
Conclusion
There was a rise in trend in the use of modern contraception followed by a plateau in the last two years of study. Most clients were young, educated and of low parity. Implants were the most preferred methods.
Introduction
Contraception involves all actions aimed at either preventing fertilisation of the gametes or implantation of the zygote. It is immaterial whether the means of doing so are traditional or orthodox or even whether they are effective or not [1]. The use of family planning should be an informed decision that should be made by couples. This is in order to limit the number, timing and spacing of the children that they want, to promote the health and welfare of the family group and contribute to the advancement of the society [1-3]. It essentially refers to practices that help individuals or couples to attain the objectives of, avoiding unwanted births, bring about wanted births, regulate intervals between pregnancies, control the time at which births occur in relation to the ages of the parents and to determine the number of children in the family [1,2].
There is a lot of evidence on the benefits of family planning [1-9]. The main aim of family planning is to improve the quality of life of the populace. Family planning empowers women and is a proven and cost-effective health intervention [3-5,7]. It can reduce up to 32% of all maternal deaths and nearly 10% of childhood deaths if it were readily available [1-5].
Family planning directly reduces the number of maternal deaths because it reduces the chance of pregnancy and its associated complications [5-7]. Furthermore, it lowers the risk of having an unsafe abortion for unintended pregnancy, delays first pregnancy in young women who might have premature pelvic development, and reduces hazards of frailty from high parity and closely spaced pregnancies [5,6].
Contraception has the potential to ensure optimum spacing between successive pregnancies thereby improving perinatal, infant, and child health [5-7]. Evidence shows that, in developing countries, when conception occurs within six months of a previous birth the risk of prematurity and low birthweight doubles [1,2,4,6]. Contraception improves health, economic and social outcomes for women and their families as well as impacting positively on public and environmental health [6-8].
Reports suggest that contraception has been a contributor to halving the number of maternal deaths worldwide between 1990 and 2010 [5,6]. For example, east Asia has made the maximum advancement in preventing maternal deaths and has a contraceptive frequency rate of 84%; in contrast, sub-Saharan Africa, which has the highest rates of maternal death, has an average Contraceptive Prevalence Rate (CPR) of 22% [5,6]. Despite the high maternal mortality rates in Nigeria the use of modern contraception has been found to be low especially in the area under study, the Northwest [8,9]. The low CPR is due to interplay of social, economic, cultural and religious factors with a persistent strong preference for large families [9-13].
The aim of this study was to find out the preferred methods of modern contraception and to determine the trend of acceptance of contraception in the new Fertility Research Unit (FRU) of the Department of Obstetrics and Gynaecology Usmanu Danfodiyo University Teaching Hospital (UDUTH) Sokoto, Nigeria.
Materials and Methods
Usmanu Danfodiyo university teaching hospital is the tertiary hospital in Sokoto. It has all the major clinical departments and provides all levels of care. The Department of Obstetrics and Gynaecology has four units which operate the antenatal, postnatal and gynaecological clinics on all weekdays. The average annual delivery rate was 3000. This is a 10-year retrospective study involving women attending the Fertility Research unit (the family planning unit) of the Department of Obstetrics and Gynaecology (O&G) of UDUTH Sokoto. The unit was fully setup in November 2007, to run family planning services and it is located within the O&G complex. Prior to this, the Department of Community health was providing family planning services in the hospital thrice a week. The fertility research unit is overseen by the consultants from the fertility regulation unit of the department and a resident Doctor rotates through the unit every month. The unit is manned by three Nurses and Midwives trained in the provision of family planning services and an average of 30 patients were seen daily. The unit receives clients primarily from the postnatal gynaecological and outpatient clinics. Furthermore, clients also come from Sokoto metropolis, neighbouring states and even nearby Niger republic. The clinic runs from 8 am to 4 pm on Mondays to Fridays. Services provided include counselling on the various modern methods of family planning, administration of such services following informed choice as well as periodic follow-up after a choice has been made. Contraceptive methods available at the unit include hormonal agents like the contraceptive pills, the monthly combined injectable (Norigynon®), the monthly injectable norethisterone oenanthate (Noristerat®) the three-monthly injectable depo medroxy progesterone acetate (Depo-Provera®) the single rod etonorgestrel containing subdermal implant (Implanon®) and the two rod levonorgestrel containing subdermal implant (Jadelle®). In addition, the levonorgestrel intrauterine system (LNG IUS) and Copper T intrauterine devices were also available. Tubal ligation and other sterilisation methods are performed by the various units within the department either during obstetric emergencies or as elective procedures from referrals from the research unit. At inception in 2007, the commodities were bought and therefore had to be paid for by the clients. However, since 2012 most commodities are provided free of charge by the federal government except for norigynon which was bought from society for family health and LNG IUS bought from multiple sources.
On presentation, socio-demographic data of the clients are recorded and registered. They receive detailed counselling on the various methods of contraception available, their benefits, risks and side-effects, so that informed choices could be made relative to a particular method. Their bio-data was obtained and a brief history was also taken. A general physical examination was performed and a recording of the pulse, blood pressure was performed. The clients’ choice of contraception was noted and entered in a register. All the registers and case notes of all clients in the unit were reviewed. The theatre case notes of patients who preferred tubal ligation as a mode of contraception were also followed-up. The total deliveries during the study period was obtained from the labour ward and theatre records. The period of study was for the entire 10 years of existence of the unit from 1st January 2008 to 31st December 2017. Approval of ethical committee was obtained.
Statistical Analysis
The data extracted were analysed using IBM SPSS version 23.0. Data were analysed using frequencies and percentages. Chi-square test was used for associations and level of significance was set at p<0.05.
Results
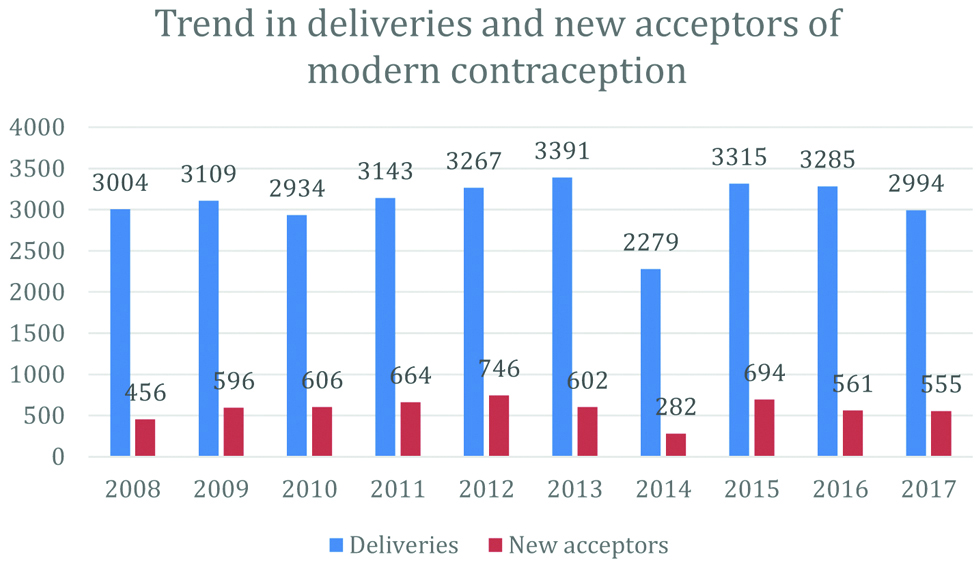
There were 11,577 acceptors of family planning during the study period. Of these 5762 were new acceptors while the rest had either changed their contraceptive methods or they were continuing with their previous method. There were 30,721 deliveries during the study period. This gives a contraceptive prevalence rate of 18.8% and an annual acceptor rate of 576.2 for modern contraception. The [Table/Fig-1] shows the trend in the number of deliveries and the new acceptors of modern contraceptive methods over the years of study. For the new acceptors from a modest 456 clients at inception in 2008, there was a steady rise in new acceptors to reach a peak of 746 in 2012. Thereafter, barring the dip in 2014, the number of new acceptors has plateaued to 561 and 555 in the last two years of the study. This rise in trend was statistically significant χ2=562.64 p<0.001. The reduction in 2014 was as a result of the multiple industrial actions that affected the activities in the unit and hospital in that year.
The trend in the number of new acceptors.
The mean age of the clients was 27.2±6.77 years. Up to 400 (6.9%) clients were teenagers and 53 (0.9%) were 14-year-old [Table/Fig-2]. Other socio-demographic profile of all new acceptors of contraception are given in [Table/Fig-2].
Sociodemographic Profile of All New Acceptors of Contraception.
| Variable | Frequency | Percent (%) |
|---|
| AGE | | |
| <=14 | 53 | 0.9 |
| 15-19 | 347 | 6.0 |
| 20-24 | 1578 | 27.4 |
| 25-29 | 1564 | 27.1 |
| 30-34 | 1175 | 20.4 |
| 35-39 | 712 | 12.4 |
| 40-44 | 262 | 4.5 |
| 45-49 | 62 | 1 |
| 50+ | 10 | 0.2 |
| Total | 5762 | 100.0 |
| TRIBE | | |
| Hausa/Fulani | 4848 | 84.2 |
| Yoruba | 237 | 4.1 |
| Igbo | 197 | 3.4 |
| Others | 480 | 8.3 |
| Total | 5762 | 100.0 |
| PARITY | | |
| Nullipara | 50 | 0.9 |
| Primipara | 1554 | 27 |
| Multipara | 2119 | 36.8 |
| Grand multipara | 1671 | 29 |
| Great grand multipara | 368 | 6.1 |
| Total | 5762 | 100.0 |
| OCCUPATION | | |
| Housewife | 4487 | 78 |
| Civil servant | 757 | 13.1 |
| Business | 83 | 1.4 |
| Student | 435 | 7.5 |
| Total | 5762 | 100.0 |
| EDUCATIONAL STATUS | | |
| Primary | 766 | 13.3 |
| Secondary | 1622 | 28.1 |
| Tertiary | 1821 | 31.6 |
| Quranic | 50 | 1.0 |
| Not educated | 1101 | 19.1 |
| Not available | 402 | 6.9 |
| Total | 5762 | 100.0 |
| REASON FOR CONTRACEPTION | | |
| Spacing | 4807 | 83.3 |
| Limit family size | 858 | 15 |
| Post abortion care | 97 | 1.7 |
| Total | 5762 | 100.0 |
The [Table/Fig-3] highlights the preferred methods of contraception during the entire study period. The Implanon® was the preferred contraceptive method of choice in 2698 (46%) of the new clients Jadelle® was next with 942 (16%) clients using it. The least preferred methods were the LNG IUS in 76 (1.6%) clients, Norigynon in 73 (1.2%) clients and the female condom in 73 (1.2%) clients respectively. The introduction of the single rod implant Implanon® in Sokoto coincided with the inception of the clinic. It made the highest contribution among all the methods in 2008 and it has steadily maintained this highest contribution to reach a peak contribution of 59.8% in the last year of study. It was consistently the dominant method during the entire period of study.
Percentage contribution of each method over the period of study.
| Method | 2008 (%) | 2009 (%) | 2010 (%) | 2011 (%) | 2012 (%) | 2013 (%) | 2014 (%) | 2015 (%) | 2016 (%) | 2017 (%) | Total |
|---|
| Implanon | 179 (39.3) | 298 (54.5) | 222 (36.6) | 345 (51.9) | 297 (39.8) | 262 (43.5) | 94 (26.2) | 348 (50.1) | 314 (55.9) | 332 (59.8) | 2698 |
| Jadelle | 0 (0) | 0 (0) | 4 (0.6) | 48 (7.2) | 187 (25.0) | 137 (22.7) | 65 (23.0) | 239 (34.4) | 140 (24.9) | 122 (21.9) | 942 |
| Noristerat | 110 (24.1) | 83 (13.9) | 134 (22.1) | 35 (5.2) | 37 (4.9) | 33 (5.4) | 31 (10.9) | 15 (2.1) | 10 (1.7) | 9 (1.6) | 497 |
| Bilateral tubal ligation | 43 (9.4) | 49 (8.2) | 57 (9.4) | 14 (2.1) | 21 (2.8) | 41 (6.8) | 26 (9.2) | 21 (3.5) | 43 (7.6) | 46 (8.2) | 362 |
| Cu T IUD | 39 (8.6) | 52 (8.8) | 68 (11.2) | 58 (8.8) | 47 (6.3) | 14 (2.4) | 19 (6.7) | 12 (1.7) | 18 (3.2) | 8 (1.4) | 338 |
| Depo provera | 22 (4.8) | 11 (1.8) | 81 (13.3) | 30 (4.5) | 69 (9.2) | 38 (6.3) | 17 (6.0) | 19 (2.7) | 19 (3.3) | 19 (3.4) | 325 |
| Pills | 49 (10.7) | 65 (10.9) | 22 (3.6) | 33 (4.9) | 28 (3.7) | 14 (2.4) | 17 (6.0) | 30 (4.3) | 10 (1.7) | 15 (2.7) | 284 |
| Male condom | 0 (0) | 6 (1.0) | 7 (1.1) | 47 (7.0) | 4 (0.6) | 5 (0.9) | 9 (3.1) | 8 (1.2) | 3 (0.5) | 2 (0.3) | 94 |
| LNG IUS | 2 (0.4) | 0 (0) | 3 (0.5) | 9 (1.3) | 19 (2.6) | 22 (3.6) | 14 (4.9) | 0 (0) | 4 (0.7) | 2 (0.3) | 76 |
| Female condom | 2 (0.4) | 0 (0) | 3 (0.5) | 29 (4.3) | 28 (3.7) | 1 (0.1) | 10 (3.5) | 0 (0) | 0 (0) | 0 (0) | 73 |
| Noriygynon | 10 (2.2) | 4 (0.6) | 5 (0.8) | 15 (2.2) | 7 (0.9) | 32 (5.3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 73 |
| Total | 413 | 547 | 549 | 650 | 725 | 561 | 256 | 672 | 518 | 509 | 5762 |
Jadelle® was introduced into the contraceptive method mix in the year 2010. Prior to this period, it was not available at all in Sokoto. It made a modest contribution of 0.6% in that year. It steadily increases to reach a peak of 34% in 2015 and thereafter plateaued to 24.9% and 21.9% in the last two years of the study.
Noristerat® at the outset made its maximal contribution of 24.1% in 2008. However, it slowly and steadily plummeted to 1.7% and 1.6% in the last years of study.
Female sterilisation made its maximal contribution of 9.4% in 2008 but thereafter has gradually plateaued to 7.6% and 8.2% in 2016 and 2017, respectively.
The Copper T intrauterine device contributed 8.4% at the beginning of the study but steadily reduced to 1.4% at the end of the period of study. A similar pattern of decline was noticed for the Depo-Provera® and the oral contraceptive pills.
There was no particular pattern noticed for the male condom for apart from a peak of 7% noted in 2011 in the three years preceding that and all the subsequent years its use has been consistently low in about 0.5-1% of clients.
The LNG IUS made an initial contribution of 0.4% to the contraceptive method mix. It had a peak of 4.9% in 2014 but dropped to 0.3% in 2017. However, it didn’t add anything in 2009 and 2015.
Norigynon® made a contribution of 2.1% at the outset in 2008 it had a peak of 5.2% in 2013 and abruptly ceased from then up till the end of the period under study.
The female condom made a modest contribution of 0.4% in 2008. It had a peak of 4.3% in 2011 a dip in 2013 and resurged to reach 3.5% in 2014. Since then it abruptly ceased up till the end of the period under study [Table/Fig-3].
Discussion
The average number of new acceptors of modern contraceptive methods at the fertility research unit of Usmanu Danfodiyo university Sokoto is 576.2 per annum. This is more than thrice the annual acceptor rate of 167 reported in the same centre about a decade earlier [11,12]. For the new acceptors of modern contraceptive methods over the years of study from a modest 456 clients at inception in 2008 there was a steady rise in new acceptors to reach a peak of 746 in 2012 and then plateaued to 561 and 555 in the last two years of the study. These findings suggest an increase in acceptance of the modern contraceptive methods. Several reasons could account for this. Perhaps the general increase in enlightenment and awareness campaigns all over the state has had an impact. In addition, patients are referred directly to the unit from the postnatal clinic. Furthermore, an increase in access to services by the introduction of the fertility research unit that provides daily services may have also contributed to an increase in acceptance. The plateau observed in the last two years is most likely because the number of returning clients who would use their old case notes has now greatly exceeded the new clients. This is evident from the difference observed between all the clients seen in the unit over the 10 years (11,577) and the new acceptors (5760).
All the clients were female and all of them were married. The age range of the women was 14-54 years. The mean age was 27.2 years and about 7.4% were less than 20-year-old. This represents the active reproductive age that are actually in need of family planning. This finding also reflects the practice of early marriage which is common in the cultural setting of the area of study. This could also mean younger women were accessing and accepting modern contraceptive methods in our conservative environment. The age is similar to findings reported from Kano [13,14] Nasarawa [15] and Maiduguri [16] all in northern Nigeria. Similar sociocultural settings may account for this. The mean age is however lower than that reported from Lagos [17] and Port Harcourt [18] in southern Nigeria.
Women of low parity constituted 64.7% of new clients. About 50 (0.9%) clients were nulliparous and 27% were primiparas. The clients were mainly housewives (78.5%) and more than half of them (59.7%) had secondary and tertiary level of education. This is similar to findings from other studies [11-18]. It is a known fact that the more educated a woman is the more likely she is to use modern contraceptive methods.
Implanon® was the preferred contraceptive method of choice amongst the new acceptors. Its introduction into the contraceptive method in Sokoto coincided with the inception of the new clinic in November 2007. It has maintained its position as the preferred method among new and returning clients over the entire duration of study. Despite the fact that Jadelle® was introduced into the unit in 2010 its use has gradually and steadily increased over the 10-year period to make it the second preferred method. The implants are therefore the preferred methods amongst the study group. This was regardless of the cost of the implants because they were still the preferred choices even when commodities were not free of charge. It seems the implants are slowly replacing the injectables like Noristerat, the Copper TIUD and the pills which were popular in the first two years of study. This is a paradigm shift from what had been reported from earlier studies in the same centre [11,12] where the Copper T intrauterine device was the most popular followed by the injectables. This finding is also at variance with what has been reported in Port Harcourt [17], Kano [13], Zaria [19] and Maiduguri [16], where the injectables were the preferred methods. In Ilorin [20] and Jos [21] the IUDs were the preferred methods. Most of the above studies were conducted prior to 2008 when the implants were just newly introduced. Newer studies in Lagos [17] and Nasarawa [15] also found implants as the preferred methods amongst their clients. The implants are highly effective, safe, convenient and do not require partner involvement. However, despite the fact that the implants are long-acting reversible contraceptive methods the clients in this study were using them for spacing (89.4%).
It’s not surprising that IUDs have fallen into disfavour as the exposure it requires for it to be inserted is something that is found culturally unacceptable in a conservative society like ours [14,16,19].
In contrast to what was found in other studies [22] where contraceptive pills were the most accepted, the pills were not popular in this study. Probably the burden of swallowing a tablet every day when one could choose other options may be an explanation. Furthermore, the study population were all married women. The young sexually active unmarried population amongst whom the pills are popular can easily purchase them off the counter and may not need to come and subject themselves to scrutiny in a hospital setting. This could be similar to why the male condoms were also not popular. The use of male condoms in the marital setting may suggest a lack of trust [22-24]. It was however interesting to note that female condom was accepted by up to 73 patients from 2008 to 2014 when it was available. It was out of stock thereafter. Although it’s no longer preferred by the new clients it is noteworthy that there are old patients of the unit who still use them till date.
About 73 clients (1.3%) preferred Norigynon when it was available. This low uptake is similar to 1.6% reported from port Harcourt [25]. This product was purchased from Society for Family Health (SFH) from 2008-2013. Unfortunately, its production and supply abruptly ceased thereafter.
The LNG IUS was preferred by 1.3% of clients. It was never supplied amongst the free commodities and its purchased when a client demands it. In 2009 and 2015 it wasn’t even available for purchase. Its exorbitant cost is a major limitation to its use. It was interesting to note that these least preferred methods viz. LNG IUS, Norigynon and female condom did not feature in the contraceptive method option in most of the studies in Nigeria [18-22]. The Fertility Research unit therefore appears to have a wider contraceptive method mix.
There were no male clients and no vasectomies. Similarly, although female sterilisation was accepted by about 6.3% over the 10-year period majority of them were for treatment of ruptured uterus and completed families following repeated cesarean sections. Its permanent nature and sociocultural barriers make sterilisation unpopular in our environment [13-18].
Limitation
A limitation of the study was that it was a retrospective review therefore complete information was not available in all aspects. A prospective study in the same centre and population-based studies in the Sokoto community would be more informative. Furthermore, in-depth studies on the profiles and effects of the subdermal implants on the women in this locality are also recommended.
Conclusion
There was a rise in trend in the use of modern contraception in the fertility research unit of Usmanu Danfodiyo university teaching hospital Sokoto. Most clients were young, educated and of low parity. The most preferred methods were Implanon®, Jadelle® and Noristerat® while the least preferred methods were the LNG IUS, Norigynon and the female condom.
[1]. Smith R, Ashford l, Gribble J, Clifton D Family planning saves lives. 4th edn Population Reference Bureau 2009 :01-22. [Google Scholar]
[2]. Cleland J, Conde-Agudelo A, Peterson H, Ross J, Tsui A, Contraception and healthLancet 2012 380:149-59.10.1016/S0140-6736(12)60609-6 [Google Scholar] [CrossRef]
[3]. WHO. Report of a WHO technical consultation on birth spacing: Geneva, Switzerland, 13-15 June, 2005. WHO/RHR/07.1. Geneva: World Health Organization, 2007 [Google Scholar]
[4]. Stover J, Ross J, How increased contraceptive use has reduced maternal mortalityMatern Child Health J 2010 14:687-95.10.1007/s10995-009-0505-y19644742 [Google Scholar] [CrossRef] [PubMed]
[5]. Cleland J, Bernstein S, Ezeh A, Faundes A, Glasier A, Innis J, Family planning: the unfinished agendaLancet 2006 368:1810-27.10.1016/S0140-6736(06)69480-4 [Google Scholar] [CrossRef]
[6]. Ahmed S, Li Q, Liu L, Tsui AO, Maternal deaths averted by contraceptive use: an analysis of 172 countriesLancet 2012 380:111-25.10.1016/S0140-6736(12)60478-4 [Google Scholar] [CrossRef]
[7]. Osotimehin B, Family planning save lives, yet investments falterLancet 2012 380:06-07.10.1016/S0140-6736(12)60906-4 [Google Scholar] [CrossRef]
[8]. Monjok E, Smesny A, Ekabua J, Essien J, Contraceptive practices in Nigeria: literature review and recommendation for future policy decisionsOpen access Journal of Contraception 2010 (1):09-22.10.2147/OAJC.S9281 [Google Scholar] [CrossRef]
[9]. Adeokun LA, Sociocultural aspects of family planning and HIV/AIDS in Nigeria 2009 61st ednABBI Ibadan:148 [Google Scholar]
[10]. Tunau KA, Awosan KJ, Adamu H, Muhammad U, Hassan M, Nasir S, Comparative assessment of modern contraceptives’ knowledge and utilization among women in urban and rural communities of Sokoto State, NigeriaJournal of Medicine and Medical Sciences 2016 7(1):006-14. [Google Scholar]
[11]. Ibrahim MI, Okolo RU, Profile of contraceptive acceptors in UDUTH Sokoto NigeriaNigerian Med Prac 1997 33:913 [Google Scholar]
[12]. Isah AY, Nwobodo EI, Family Planning Practice in tertiary health institution in north-western NigeriaNigeria Journal of Clinical Practice 2009 12:281-83. [Google Scholar]
[13]. Muhammad Z, Maimuna DG, Contraceptive trend in a tertiary facility in North Western Nigeria: A 10-year reviewNiger J Basic Clin Sci 2014 11:99-103.10.4103/0331-8540.140358 [Google Scholar] [CrossRef]
[14]. Yakassai IA, Yusuf AM, Contraceptive choices amongst women in Kano, Nigeria: A five (5) year reviewJ Med Trop 2013 15:113-16.10.4103/2276-7096.123586 [Google Scholar] [CrossRef]
[15]. Ogbe AE, Ayeni HAD, Ononuju C, Oyeniran OF, Modern contraceptive preferences among women accessing family planning services at a specialist hospital in North central NigeriaJos Journal of Medicine 2014 8(2):01-06. [Google Scholar]
[16]. Mairiga AG, Kyari O, Audu B, Lawuwa M, Socioclinical characteristics of modern contraceptive users at the university of Maiduguri teaching hospitalNigeria Journal of Clinical Practice 2007 10:152-55. [Google Scholar]
[17]. Okunade KS, Daramola E, Ajepe A, Sekumade A, A 3-year review of the pattern of contraceptive use among women attending the family planning clinic of a University Teaching Hospital in Lagos, NigeriaAfr J Med Health Sci 2016 15:69-73.10.4103/2384-5589.198317 [Google Scholar] [CrossRef]
[18]. Ojule JD, Abam DS, Contraceptive Trends and Preferred Methods among Users in Port Harcourt, Niger Delta Region of NigeriaJournal of Biosciences and Medicines 2017 5:97-107.10.4236/jbm.2017.58008 [Google Scholar] [CrossRef]
[19]. Ameh N, Sule ST, contraceptive choices among women in Zaria, NigeriaNiger J Clin Pract 2007 10:205-07. [Google Scholar]
[20]. Idowu OA, Munir’deen AI, Recent trend in pattern of contraceptive usage at a Nigeria tertiary HospitalJ Clin Med Res 2010 2:180-84. [Google Scholar]
[21]. Mutihir JT, Pam VC, Overview of contraceptive use in Jos University Teaching Hospital, north central NigeriaNiger J Clin Pract 2008 11:139-43.10.4314/jmt.v9i2.35208 [Google Scholar] [CrossRef]
[22]. Mutihir JT, Dashala HL, Madaki JKA, Contraceptive pattern at a comprehensive Health Centre in a Sub-Urban SettingTrop J Obstet Gynaecol 2005 22:144-46.10.4314/tjog.v22i2.14514 [Google Scholar] [CrossRef]
[23]. Iliyasu Z, Mandara MU, Mande AT, Community leaders\perception of reproductive health issues and programmes in Northeastern NigeriaTrop J Obstet Gynaecol 2004 21:83-87.http://dx.doi.org/10.4314/tjog.v21i2.1447310.4314/tjog.v21i2.14473 [Google Scholar] [CrossRef]
[24]. Keele JJ, Forste R, Flake DF, Hearing native voices: Contraceptive use in Matamwe village, East AfricaAfr J Reprod Health 2005 9:32-41.10.2307/358315816104653 [Google Scholar] [CrossRef] [PubMed]
[25]. Dimkpa OJ, Okwudili OE, Experience with combined injectable contraceptive (Norigynon) in Port HarcourtBritish Journal of Medicine & Medical Research 2017 19(1):01-06.10.9734/BJMMR/2017/29727 [Google Scholar] [CrossRef]