Introduction
Smooth muscle tumours are rare in vulva comprising of 0.03% of all gynaecologic neoplasms [1] and malignant variety i.e., sarcomas accounting for only 1% to 2% of vulvar tumours [2].
Here we present three cases, two of vulvar leiomyomas and third of vulvar leiomyosarcoma with an aim to emphasise the need for broad vision of differentials and clinical suspicion to avoid missing out on malignant ones and provide the best prognosis to patients.
Case Series
Case I
A 26-year-old primigravida at 18 weeks gestation presented with complaints of discomfort due to a mass in perineum which appeared first when she was eight-year-old. Clinical examination revealed a spongy mass of size 6.5×4 cm on right labia majora in the region of bartholin gland with absence of inguinal adenopathy. It had well defined borders and was non-tender, soft in consistency. There was no organomegaly. Haemogram, urinalysis, and blood chemistry reports were normal.
A clinical diagnosis of bartholin cyst was made and planned for day care surgery. Incision at the mucocutaneous junction was given and a soft, fleshy, and well defined mass was removed. Cut surface of the lesion was white, whorled, and rubbery, without hemorrhage or necrosis [Table/Fig-1a]. The patient had a good recovery postoperatively and delivered a healthy baby vaginally at term gestation. Patient is regularly followed up with no recurrence till 2.5 years now.
(a) Encapsulated soft tissue mass showing white, whorled, rubbery surface on cut section without hemorrhage or necrosis; (b) Tumour cells are oval to elongated in shape arranged in fascicles with eosinophilic cytoplasm (20x); (c) Tumour cells are positive for Progesterone Receptor (PR).
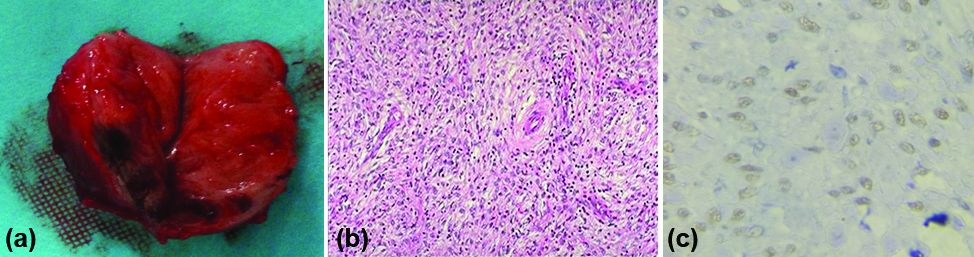
Sections stained with haematoxylin and eosin stain showed spindle shaped cells arranged in fascicles with eosinophilic cytoplasm [Table/Fig-1b]. Focal myxoid change was seen with no atypical mitosis. Tumour cells were positive for vimentin, Smooth muscle actin, Progesterone Receptor [Table/Fig-1c] and negative for keratin and Estrogen Receptor. Hence a diagnosis of vulvar leiomyoma with focal myxoid change was made.
Case II
A 31-year-old, third gravida woman presented to us at third trimester of pregnancy at term and in labour. She had no complaints and the vulvar mass was discovered during routine examination [Table/Fig-2]. The mass was around 5×6×4 cm soft and non-tender on left vulva. Patient delivered vaginally and was discharged with instruction to follow-up at six weeks. After six weeks, the mass was excised and defect was closed. Immunohistochemistry and microscopic study confirmed it to be benign vulvar leiomyoma.
Vulvar mass on left labia.

Case III
A 38-year-old, para 3 woman presented with complaints of pain, ulceration of a gradually growing mass in vulva for the last eight months. Her BMI was 26 with no significant medical history and no previous gynaecologic illness. On examination 8×6.5×5 cm sized soft, ulcerated, tender mass on right upper vulva was seen. Biopsy revealed the diagnosis of malignant sarcoma. Lymphangiographic studies revealed normal inguinal and iliac nodes. No abnormality was detected in proctoscopy, cystoscopy, barium enema study, intravenous pyelography, bone scan, pelvic and chest roentgenograms. Positron Emission Tomography-Computed Tomography (PET-CT) revealed no distant metastasis. A wide local excision was performed and defect was closed without graft with satisfactory appearance. In view of the absence of lymphovascular space invasion and metastasis on imaging, inguinal lymphadenectomy was decided not to be done. Patient recovered well and postoperative period was uneventful.
Final pathologic study revealed a highly cellular tumour underlying dermis [Table/Fig-3a], showing infiltration and extensive areas of haemorrhage and necrosis [Table/Fig-3b]. The tumour cells were spindle in shape arranged in fascicles and bundles [Table/Fig-3c] showing high degree of pleomorphism and atypical mitosis (4-5/hpf) along with many tumour giant cells [Table/Fig-3d]. There was no lymphovascular invasion. Tumour cells were positive for vimentin [Table/Fig-3e], SMA [Table/Fig-3f] and negative for CK, desmin, S-100, HMB-45, CD34, ER and PR all features suggestive of pleomorphic sarcoma more specifically MFH (Malignant Fibrous Histiocytoma).
(a) Skin lined tissue showing spindle cell tumour underlying dermis (20x); (b). Tumour along with area of necrosis (20x); (c) Highly cellular spindle cell tumour where tumour cells arranged in fascicles and bundles (20x); (d) showing pleomorphic tumour cells, atypical mitosis (yellow arrow) and tumour giant cell (blue arrow) (40x); (e) Tumour cells are positive for vimentin (100x); (f) Tumour cells are positive for SMA (100x).

Patient was given chemoradiation in the postoperative period. The case was discussed further in oncology board meet of the institution where decision for regular follow-up and surveillance was taken after reviewing pathology and imaging. Patient has since then been followed up every four months with no evidence of disease 21 months now postvulvectomy.
Discussion
Smooth muscle tumours of vulva are rare. Reidel found an incidence of 0.7% of leiomyoma in a review of 144 vulvar tumours [3]. Diagnosis poses a challenge in view of its rarity apart from distinguishing benign from malignant ones. This is due to different diagnostic criterion used for smooth muscle tumours of gynaecologic and nongynaecologic origin. Microscopy showing significant mitotic activity, focal degenerative cellular atypia, and/or hyaline necrosis can be normal finding in benign gynaecologic leiomyoma but the same features may suggest leiomyosarcoma in smooth muscle tumours of nongynaecologic origin [4].
Tavassoli FA et al., in 1979 reviewed the histologic slides of 32 smooth muscle tumours, seven of them being leiomyoma found in pregnant patients and seven cases of leiomyosarcoma. He predicted three determinants of prognosis which were tumour, size, contour and mitotic activity. Tumours with size more than 5 cm, having infiltrative margins, and ≥5 mitotic figures per 10 hpf were likely to recur and should be regarded as sarcomas. But the sample size was too small to validate the role of mitotic activity in predicting the tumour histology [5]. Nielsen GP et al., in 1996 did an analysis of clinical and pathological features of 25 smooth muscle tumours out of which two cases were leiomyoma in pregnant patients and five cases were that of leiomyosarcoma. It was observed that the tumour which recurred or metastasized had certain common features viz., size more than 5 cm, an infiltrative margin, a mitotic count of 5 or more per 10 hpf, and grade 2 to 3 nuclear atypia. If at least three out of these four features were present, leiomyosarcoma was diagnosed, if only two were present, atypical leiomyoma was diagnosed and if only one or none of the features were present, it was assumed to be leiomyoma. They hence added moderate to severe cytological atypia as a fourth feature to distinguish benign from malignant smooth muscle growth [6]. Considering these criterion, our first and second cases were diagnosed as benign leiomyoma in second and third trimester of pregnancy respectively. The tumours were well circumscribed with no atypical mitosis. Although the size crossed the 5 cm mark, in the absence of other 3 features, leiomyoma was diagnosed and local excision was done in both cases. [Table/Fig-4] summarises the 13 cases of leiomyoma in pregnant patients including our present cases [5-8].
Cases of vulvar leiomyoma diagnosed during pregnancy [5-8].
| No of cases | Serial no: | Age | Size (cm) | Atypia | Mitotic figures per 10 hpf | Margins | SMA | Vimentin | Desmin | Cytokeratin | S 100 | ER | PR | Cell type | Myxoid change | Diagnosis | Treatment | Follow-up |
|---|
| Tavassoli FA et al, [5] | 7 | 1 | 30 | 11.5 | 1+ | 0 | WC | ND | ND | ND | ND | ND | ND | ND | SC | P | L | WLE | NR |
| 2 | 24 | 1.5 | 1+ | 0 | WC | ND | ND | ND | ND | ND | ND | ND | SC | P | L | EN | NR, 7 years |
| 3 | 28 | 4.5 | 1+ | 2 | WC | ND | ND | ND | ND | ND | ND | ND | SC | P | L | EN | NR, 7 years |
| 4 | 26 | 1.5 | 1+ | 2 | ID | ND | ND | ND | ND | ND | ND | ND | SC | P | L | EN | NR, 7 years |
| 5 | 35 | 6 | 1+ | 1 | WC | ND | ND | ND | ND | ND | ND | ND | SC | P | L | EN | Lost to FU |
| 6 | 31 | 4 | 1+ | 1 | WC | ND | ND | ND | ND | ND | ND | ND | SC | P | L | EN | Lost to FU |
| 7 | 25 | 3 | 0 | 0 | WC | ND | ND | ND | ND | ND | ND | ND | SC | P | L | EN | Lost to FU |
| Nielson GP et al., [6] | 2 | 8 | 40 | 8 | 2 | 3 | U | P | P | P | N | N | N | N | SC | N | AL | LE | NR till 19 years |
| 9 | 20 | 2.8 | 3 | 2 | FI | P | P | P | N | N | P | P | SC | P | AL | LE | NR till 3 years |
| Kajiwara H et al., [7] | 1 | 10 | 29 | 4×4×4.5 | 0 | 0 | NTR | P | P | P | N | N | N | N | SC | P | L | LE | NR |
| Zhou J et al., [8] | 1 | 11 | 29 | 8.5×7.5×6.5 | 0 | <1 | NTR | P | P | P | N | ND | P | P | SC | P | L | LE | NR till 29 months |
| Our cases, 2019 | 2 | 12 | 26 | 6.5×4 | 0 | 0 | WC | p | p | p | N | N | N | P | SC | P | L | LE | NR till 2.5 years |
| 13 | 31 | 5×6×4 | 0 | 0 | WC | P | P | P | N | N | N | P | SC | P | L | LE | NR till date |
C: Well circumscribed; ID: Indeterminate; FI: Focally infiltrating; U: Unknown; SC: Spindle cell; NTR: Not reported; ND: Not done; L: Leiomyoma; AL: Atypical leiomyoma; WLE: Local wide excision; EN: Enucleation; LE: Local excision; P: Positive; N: Negative; NR: No recurrence; S 100: Homodimeric proteins used as marker; FU: Follow-up
Kawaguchi K et al., observed that ER expression was suppressed in the secretory phase and during pregnancy both in myometrium and in leiomyoma’s whereas PR was expressed both in the myometrium and leiomyoma’s throughout the menstrual cycle and pregnancy [9]. Our case was positive for progesterone receptor and negative for ER receptors. Hence there may be a significant role of progesterone receptors in the growth of smooth muscle tumours arising in uterus and vulva. This may explain why tumour in our case grew during pregnancy under the influence of increased level of progesterone. Even Kajiwara H et al., in his literature review found PR expression in 85.0% in contrast to ER expression in 73.7% smooth muscle tumours of the vulva [7]. However, the other 4 cases [Table/Fig-4] were equivocal in determining this fact as 2 cases (cases 9 and 11) stained positive for both ER and PR receptors and other 2 cases (cases 8 and 10) negative for both of them. More studies have to be undertaken to validate the role of PR receptors in the probable role of growth of vulvar SMTs [6-8].
Myxoid change was evident in 11 cases who were less than 35-year-old. Only one case of Nielsen GP et al., series (case 8) who was 40-year-old had no myxoid change [6]. This finding calls for research related to influence of young age and pregnancy on degeneration of tumours. The manifold hormonal changes of pregnancy may induce myxoid change in smooth muscle tumours of vulva which is yet to be established. Newman PL et al., noted that myxoid or hyalinizing changes were found more commonly in smooth muscle tumours of the vulva than those that occurred in scrotum and nipple [10].
All of them had spindle cells in microscopy. Follow-up records were available for 10 patients and none of them had recurrence after enucleation or local excision. Local excision is hence recommended as initial therapy and for recurrences as well.
However, our third case had all the four features viz., size greater than 5cm, margin with infiltration, cellular atypia, atypical mitosis of 4-5/hpf, hence leiomyosarcoma more specifically malignant fibrous histiocytoma was diagnosed and partial radical vulvectomy was done. This rare variant of leiomyosarcoma of the vulva (MFH) comprise of 20-24% of all soft-tissue sarcomas, first described by O’Brien and Stout way back in 1964 [11]. With less than 10 cases reported mostly in younger and middle age women, pathogenesis of the neoplasm remains a riddle [12,13]. The tumour clinically presents as a gradually enlarging painful mass mostly found in labia majora and reaching 3-6 cm in diameter [12,14]. As a characteristic feature of sarcomas, the tumour metastasizes by haematogenous route mainly to lungs and occasionally to bones [15]. In view of the high chances of recurrence in our patient, regular follow-up of the patient is done with no recurrence till 21 months now after surgery. No specific treatment protocols have been formulated for this rare entity. However, the standard treatment recommended is surgical excision with confirmed negative margins followed by radiation therapy [16,17]. Chemotherapy may reduce the chances of recurrence and metastasis although its administration is not mandatory [18].
[Table/Fig-5] summarises the cases of leiomyosarcoma from literature. As evident it occurs in women of middle and older ages, the mean age at presentation being 42-year-old and youngest patient reported was 14-year-old [19-36]. Wide local excision was treatment of choice in most of the cases at first presentation as well as after recurrence. Metastasis to lung was observed in four cases who were treated with excision/vulvectomy with radiotherapy and chemotherapy (cases 5,6,7,8: [Table/Fig-5]). However, all of them succumbed to their disease despite receiving best treatment thus showing metastasis as the poorest prognostic factor.
Cases of vulvar leiomyosarcoma [19-36].
| Serial no. | Author | Year | Age | Size (cm) | First line tx | LR | M | Tx of recurrences | Follow-up |
|---|
| 1 | Davos I et al., [19] | 1976 | 41 | NS | WLE | - | - | - | 28 months, NR |
| 2 | 49 | NS | LE | + | - | WLE | 9 years, NR |
| 3 | Audet-Lapointe P et al., [20] | 1976 | 48 | 4 | Tumourectomy, | + | - | Radical vulvectomy+b/l inguinal LN resection | 24 months, NED |
| 4 | Guérard MJ et al., [21] | 1976 | 48 | 4 | Simple excision | + | _ | Radical vulvectomy | NED 6 months after recurrence |
| 5 | Bakri YN et al., [22] | 1979 | 17 | 15 | Local excision | + | lung | Local excision+ CT | DOD 9 yr |
| 6 | 1978 | 29 | 9 | Local excision | + | lung | Local excision+CT+RT | DOD 10 yr |
| 7 | 1982 | 41 | 10 | Local excision | + | lung | Local excision+CT+RT | DOD 7.5 yr |
| 8 | Guidozzi F et al., [23] | 1984 | 47 | 6 | Radical vulvectomy with B/L inguinal LN resection | + | lung | CT+RT | DOD 5 months |
| 9 | Lenaz MP et al., [24] | 1984 | 58 | NS | LE | + | - | Anterior vulvectomy with groin dissection. | NS |
| 10 | Patel S et al., [25] | 1986 | 60 | 6 | Radical vulvectomy with B/L inguinal LN dissection | + | _ | Local reexcision | NED 4 months after recurrence |
| 11 | Młler LBK et al., [26] | 1990 | 54 | 8 | Radical vulvectomy+inguinofemoral adenectomy | - | - | - | NED 30 months |
| 12 | Aartsen EJ et al., [27] | 1994 | 15 | 7 | RT | + | - | 1. RT 2. WLE | 24 years, NR |
| 13 | Tawfik O et al., [28] | 1994 | 52 | 15 | LE+RT | _ | _ | _ | NED 14 months |
| 14 | Torres Lobaton A et al., [29] | 2000 | 14 | 6 | LE | + | - | 1. WLE 2. WLE + CT 3. WLE + RT 4. Vulvectomy + Hysterectomy + RT | 22 years, NR |
| 15 | Di Gilio AR et al., [30] | 2004 | 36 | 6 | WLE + ipsilateral lymphadenectomy | - | - | - | 30 months, NR |
| 16 | Dewdney S et al., [31] | 2005 | 36 | 5 | Vulvectomy | - | - | - | 13 months, NR |
| 17 | González Bugatto F et al., [32] | 2009 | 52 | 6 | Hemivulvectomy + ipsilateral lymphadenectomy + RT + CT | + | - | WLE | 4 years, NR |
| 18 | Salehin D et al., [33] | 2011 | 71 | 2 | Hemivulvectomy + hysterectomy and salpingo - oophorectomy + inguinal lymphonodectomy. | - | - | - | NTR |
| 19 | Mowers EL et al., [34] | 2014 | 48 | 4 | Radical hemivulvectomy | - | - | - | 18 months, NR |
| 20 | Levy RA et al., [35] | 2014 | 57 | 4×2 | WLE | - | - | - | - |
| 21 | Korkmaz V et al., [36] | 2015 | 65 | 5.5 | LE | - | - | - | 6 months, NR |
| 22 | Our case | 2019 | 38 | 8×6.5×5 | WLE | - | - | - | 21 months, NR |
NR: No recurrences; CT: Chemotherapy; LE: Local excision; LR: Local recurrence; M: Metastasis; NS: Non-specified; RT: Radiotherapy; WLE: Wide local excision; NTR: Not reported; DOD: Died of disease; WC: Well circumscribed; ID: Indeterminate; FI: Focally infiltrating; U: Unknown; SC: Spindle cell; NTR: Not reported; ND: Not done; L: Leiomyoma; AL: Atypical leiomyoma; tx: Treatment, LN: Lymph node; NED: No evidence of disease
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study and for publication of their case reports.
Conclusion
Since this is a rare entity, chances to miss the diagnosis are high which in turn increases morbidity and mortality too. Any woman presenting with vulvar mass need to be closely monitored with rapid diagnosis and definite treatment.
C: Well circumscribed; ID: Indeterminate; FI: Focally infiltrating; U: Unknown; SC: Spindle cell; NTR: Not reported; ND: Not done; L: Leiomyoma; AL: Atypical leiomyoma; WLE: Local wide excision; EN: Enucleation; LE: Local excision; P: Positive; N: Negative; NR: No recurrence; S 100: Homodimeric proteins used as marker; FU: Follow-up
NR: No recurrences; CT: Chemotherapy; LE: Local excision; LR: Local recurrence; M: Metastasis; NS: Non-specified; RT: Radiotherapy; WLE: Wide local excision; NTR: Not reported; DOD: Died of disease; WC: Well circumscribed; ID: Indeterminate; FI: Focally infiltrating; U: Unknown; SC: Spindle cell; NTR: Not reported; ND: Not done; L: Leiomyoma; AL: Atypical leiomyoma; tx: Treatment, LN: Lymph node; NED: No evidence of disease
[1]. Youssef A, Neji K, M’Barki M, Ben Amara F, Malek M, Reziga H, Leiomyoma of the vulvaTunis Med 2013 91:78-80. [Google Scholar]
[2]. DiSaia PJ, Pecorelli S, Gynaecological sarcomasSemin Surg Oncol 1994 10(5):369-73.10.1002/ssu.29801005107997731 [Google Scholar] [CrossRef] [PubMed]
[3]. Riedel V, Zysten und Geschwulste des ausseren Genitale undder VaginaZentralblatt für Gynãkologie 1964 86:1597-608. [Google Scholar]
[4]. Miettinen M, Fetsch JF, Evaluation of biological potential of smooth muscle tumoursHistopathology 2006 48:97-105.10.1111/j.1365-2559.2005.02292.x16359541 [Google Scholar] [CrossRef] [PubMed]
[5]. Tavassoli FA, Norris HJ, Smooth muscle tumours of the vulvaObstet Gynaecol 1979 53:213-17. [Google Scholar]
[6]. Nielsen GP, Rosenberg AE, Koerner FC, Young RH, Scully RE, Smooth-muscle tumours of the vulva. A clinicopathological study of 25 cases and review of the literatureAm J Surg Pathol 1996 20:779-93.10.1097/00000478-199607000-000018669526 [Google Scholar] [CrossRef] [PubMed]
[7]. Kajiwara H, Yasuda M, Yahata G, Yamauchi I, Satoh S, Tirasawa T, Myxoid leiomyoma of the vulva: A case reportTokai J Exp Clin Med 2002 27(3):57-64. [Google Scholar]
[8]. Zhou J, Ha BK, Schubeck D, Moonja CP, Myxoid epithelioid leiomyoma of the vulva: a case reportGynaecol Oncol 2006 103:342-45.10.1016/j.ygyno.2006.04.00116765425 [Google Scholar] [CrossRef] [PubMed]
[9]. Kawaguchi K, Fujii S, Konishi I, Iwai T, Nanbu Y, Nonogaki H, Immunohistochemical analysis of oestrogen receptors, progesterone receptors and Ki-67 in leiomyoma and myometrium during the menstrual cycle and pregnancyVirchows Arch A Pathol Anat Histopathol 1991 419:309-15.10.1007/BF016065221949613 [Google Scholar] [CrossRef] [PubMed]
[10]. Newman PL, Fletcher CDM, Smooth muscle tumours of the external genitalia; clinicopathological analysis of a seriesHistopathology 1991 18:523-29.10.1111/j.1365-2559.1991.tb01479.x1879812 [Google Scholar] [CrossRef] [PubMed]
[11]. O’Brien JE, Stout AP, Malignant fibrous xanthomasCancer (Philadelphia) 1964 17:1445-55.10.1002/1097-0142(196411)17:11<1445::AID-CNCR2820171112>3.0.CO;2-G [Google Scholar] [CrossRef]
[12]. Iwakawa T, Tsuji T, Hamada T, Kamio M, Matsuo T, Yoshinaga M, Pleomorphic type of malignant fibrous histiocytoma with myxoid stroma of the vulva in a young womanJ Obstet Gynaecol Res 2011 37:1474-77.10.1111/j.1447-0756.2011.01528.x21564409 [Google Scholar] [CrossRef] [PubMed]
[13]. Santala M, Suonio S, Syrjanen K, Uronen MT, Saarikoski S, Malignant fibrous histiocytoma of the vulvaGynaecologic Oncology 1987 27:121-26.10.1016/0090-8258(87)90239-3 [Google Scholar] [CrossRef]
[14]. Sabesan T, Xuexi W, Yongfa Q, Malignant fibrous histiocytoma:outcome of tumours in the head and neck compared with those in the trunk and extremitiesBritish Journal of Oral and Maxillofacial Surgery 2006 44:209-12.10.1016/j.bjoms.2005.06.00616026908 [Google Scholar] [CrossRef] [PubMed]
[15]. Vural B, Ozkan S, Yildiz K, Malignant fibrous histiocytoma of the vulva: A case reportArchives of Gynaecology and Obstetrics 2005 273:122-25.10.1007/s00404-005-0047-516059739 [Google Scholar] [CrossRef] [PubMed]
[16]. Williams NP, Williams E, Fletcher H, Smooth muscle tumours of the vulva in JamaicaWest Indian Medical Journal 2002 51:228-31. [Google Scholar]
[17]. Patnayak R, Manjulatha B, Srinivas S, Leiomyosarcoma of the vulvaIndian Journal of Pathology and Microbiology 2008 51:448-49.10.4103/0377-4929.42525 [Google Scholar] [CrossRef]
[18]. Otoide V, Okobia M, Aligbe J, Vulvar leiomyosarcoma: A case report in a Nigerian womanSurgical Technology International 2002 10:71-73. [Google Scholar]
[19]. Davos I, Abell MR, Soft tissue sarcomas of vulvaGynaecol Oncol 1976 4:70-86.10.1016/0090-8258(76)90009-3 [Google Scholar] [CrossRef]
[20]. Audet-Lapointe P, Paquin F, Guerard MJ, Charbonneau A, Methot F, Morand G, Leiomyosarcoma of the vulvaGynaecol Oncol 1980 10:350-55.10.1016/0090-8258(80)90104-3 [Google Scholar] [CrossRef]
[21]. Guérard MJ, Paquin F, Audet-Lapointe P, Charbonneau A, Les sarcómes de la vulveL’Union Médicale du Canada 1979 108:501-05. [Google Scholar]
[22]. Bakri YN, Akhtar M, El-Senoussi M, Wierzbicki R, Vulvar sarcoma: a report of four casesGynaecol Oncol 1992 46:384-90.10.1016/0090-8258(92)90238-E [Google Scholar] [CrossRef]
[23]. Guidozzi F, Sadan O, Koller AB, Marks SR, Combined chemotherapy and irradiation therapy after radical surgery for leiomyosarcoma of the vulvaS Afr Med J 1987 71:327-28. [Google Scholar]
[24]. Lenaz MP, Nguyen TC, Hewett WJ, Leiomyosarcoma of the vulvaConn Med 1987 51:705-06. [Google Scholar]
[25]. Patel S, Kapadia A, Desai A, Dave KS, Leiomyosarcoma of the vulvaEur J Gynaecol Oncol 1993 14:406-07. [Google Scholar]
[26]. Młler LBK, Nielsen MN, Trolle C, Leiomyosarcoma vulvaeActa Obstet Gynaecol Scand 1990 69:187-89.10.3109/000163490090061662386022 [Google Scholar] [CrossRef] [PubMed]
[27]. Aartsen EJ, Albus-Lutter CE, Vulvar sarcoma: Clinical implicationsEur J Obstet Gynaecol Reprod Biol 1994 56:181-89.10.1016/0028-2243(94)90168-6 [Google Scholar] [CrossRef]
[28]. Tawfik O, Huntrakoon M, Collins J, Owiety T, Seoud MAF, Weed J, Leiomyosarcoma of the vulva: report of a caseGynaecol Oncol 1994 54:242-49.10.1006/gyno.1994.12028063255 [Google Scholar] [CrossRef] [PubMed]
[29]. Torres Lobaton A, Cruz Ortiz H, Rojo Herrera G, Avila Medrano L, Sarcomas of the vulva. Report of 2 casesGinecol Obstet Mex 2000 68:429-34. [Google Scholar]
[30]. Di Gilio AR, Cormio G, Resta L, Carriero C, Loizzi V, Parisi AM, Rapid growth of myxoid leiomyosarcoma of the vulva during pregnancy: A case reportInt J Gynaecol Cancer 2004 14:172-75.10.1136/ijgc-00009577-200401000-00026 [Google Scholar] [CrossRef]
[31]. Dewdney S, Kennedy CM, Galask RP, Leiomyosarcoma of the vulva: A case reportJ Reprod Med 2005 50:630-32. [Google Scholar]
[32]. González-Bugatto F, Añón-Requena MJ, López-Guerrero MA, Báez-Perea JM, Bartha JL, Hervías-Vivancos B, Vulvar leiomyosarcoma in Bartholin’s gland area: A case report and literature reviewArch Gynaecol Obstet 2009 279:171-74.10.1007/s00404-008-0652-118437406 [Google Scholar] [CrossRef] [PubMed]
[33]. Salehin D, Haugk C, William M, Hemmerlein B, Thill M, Diedrich K, Friedrich M, Leiomyosarcoma of the vulva, case reportEuropean Journal of Gynaecological Oncology 2012 33(3):306-08. [Google Scholar]
[34]. Mowers EL, Shank JJ, Frisch N, Reynolds RK, Myxoid leiomyosarcoma of the Bartholin glandObstet Gynaecol 2014 124(2 Pt 2 Suppl 1):433-35.10.1097/AOG.000000000000033725004325 [Google Scholar] [CrossRef] [PubMed]
[35]. Levy RA, Winham WM, Bryant CS, Quick CM, Smooth muscle neoplasms of the vulva masquerading as Bartholin gland duct cystsProc (Bayl Univ Med Cent) 2014 27(1):25-27.10.1080/08998280.2014.1192904324381397 [Google Scholar] [CrossRef] [PubMed]
[36]. Korkmaz V, Kurdoğlu Z, Karadag B, Arslanca T, Caydere M, Ergun Y, A rare case of leiomyosarcoma localized in the Bartholin’s gland area and review of the literatureJ Obstet Gynaecol Res 2016 42(5):589-92.10.1111/jog.1294326889877 [Google Scholar] [CrossRef] [PubMed]